Normal pressure hydrocephalus, abbreviated as NPH, is a special form of hydrocephalus and is also referred to as age-related brain pressure. Typical for NPH is a chronically delayed absorption of cerebrospinal fluid without permanently increased intracranial pressure. Affected individuals suffer from gradually increasing symptoms such as gait disturbances, cognitive impairments, and urinary incontinence. With the help of a surgical procedure to restore cerebrospinal fluid drainage, normal pressure hydrocephalus can be effectively treated.
How common is normal pressure hydrocephalus?
Normal pressure hydrocephalus has an incidence of 5.5 per 100 000 per year. With 47%, normal pressure hydrocephalus is by far the most common form of hydrocephalus in adults and is thought to be responsible for up to 6% of all dementias and a high percentage of walking disorders in the elderly. The condition peaks in the 7th decade of life and predominantly affects men.
What are the causes of normal pressure hydrocephalus?
One distinguishes the more common primary idiopathic forms without identifiable cause from the rarer secondary forms, which are attributable to a trigger such as bleeding, trauma, inflammation, or a tumor.
The cause of idiopathic normal pressure hydrocephalus (iNPH) is not yet fully understood. It is now believed to be a disorder of brain parenchyma rather than a primary disturbance of cerebrospinal fluid absorption.
Patients with idiopathic normal pressure hydrocephalus often also exhibit vascular diseases such as hypertension, leading to discussion of these as risk factors.
Explanation according to Fichtner et al *:
It has been demonstrated that in patients with iNPH, cerebral blood flow is disturbed due to reduced venous compliance, and perfusion pressure in the periventricular watershed regions is reduced. The latter leads to progressive damage to the affected brain areas. * Conversely, vascular diseases such as arterial hypertension are thus risk factors for the occurrence of iNPH *. Ultimately, cerebrospinal fluid absorption disorder is only the result of all these factors. The exclusion of other differential diagnoses (e.g.as vascular dementia) is therefore difficult, the boundaries are fluid, and a clear separation of causes is often not possible.
Explanation according to the German Society of Neurology (DGN):
In normal pressure hydrocephalus, there is intermittent intracranial pressure elevation, primarily affecting the arachnoid villi located at the convexity. Elasticity differences and physical properties of the brain result in gravitational forces initiating a sluggish "outward movement" of brain mass despite communicating internal and external CSF spaces, ultimately leading to the typical picture of NPH.
What are the symptoms of normal pressure hydrocephalus?
The characteristic features of normal pressure hydrocephalus - even if not always all occur or are equally pronounced - are a triad consisting of
- gait disturbance
- urinary incontinence
- dementia
This symptomatology is also referred to as Hakim's triad, named after the Colombian neurosurgeon Solomon Hakim. The first description of the clinical picture was made in 1965 by Hakim and Adams *, hence the name Hakim-Adams syndrome is also common. The symptoms increase in severity over weeks and months.
Usually, the first and most common symptom is gait disturbance. It is present in approximately 88% of all patients with idiopathic normal pressure hydrocephalus. The gait of affected patients is typically shuffling and small-stepped, the feet seem to stick to the ground like magnets, and there are significant problems with turning.
Bladder emptying disorder in the form of urinary incontinence occurs in about every second patient during the course of the disease. This is a neurogenic bladder emptying disorder, meaning that bladder dysfunction is due to disturbances and damage in nerve supply.
The symptoms of cognitive decline typically include orientation disorders, general psychomotor slowing, as well as lack of drive and affective flattening. Cognitive impairments are observed in approximately 83% of patients and usually occur in a later stage of the disease.
Untreated, the disease progresses slowly and chronically.
Imaging
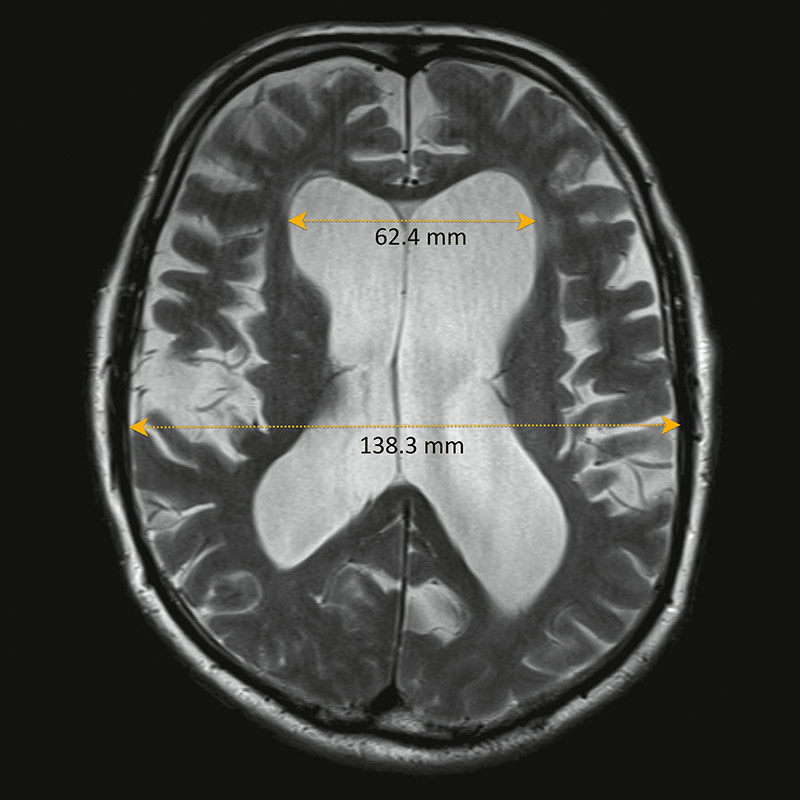
In computed tomography (CT), there is typically a disproportionate enlargement of the lateral ventricles without recognizable loss of brain substance (cortical atrophy) as seen, for example, in Alzheimer's disease. Also typical are bulges in the anterior part of the lateral ventricles and rounding of the temporal horns in the lower part of the lateral ventricles with little or no atrophy (tissue loss) of the hippocampus.
Magnetic resonance imaging (MRI) provides additional, more in-depth information than CT for differentiating normal pressure hydrocephalus from other conditions such as obstructive hydrocephalus or Alzheimer's disease.
Imaging also allows for determination of the corpus callosum angle. This angle is used as an aid in the diagnosis of normal pressure hydrocephalus. Normal values for this angle range between 100° and 120°, with the threshold being 90°. In patients with normal pressure hydrocephalus, however, it is flattened and typically measures 50–80°.
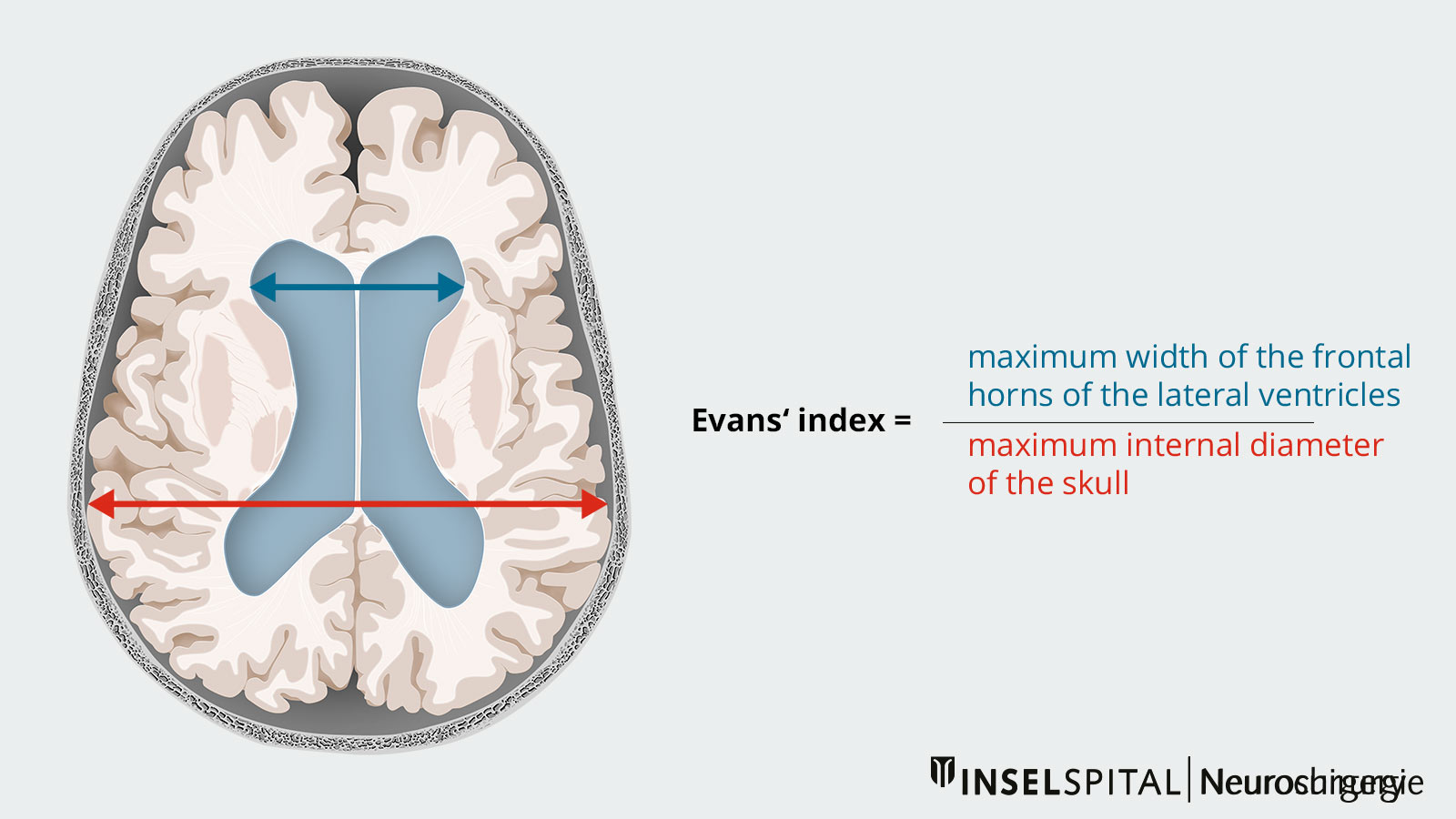
Measurement of the Evans index in cross-sectional imaging is also helpful in diagnosis. This involves measuring the ratio between the maximum width of the frontal horns of the lateral ventricles and the maximum inner diameter of the skull. If the Evans index value is > 0.3, ventricular enlargement is present. However, the value is not specific to normal pressure hydrocephalus, but serves only as a general quantitative criterion for the width of the cerebrospinal fluid spaces.
CSF tap test
During the CSF tap test a diagnostic lumbar puncture with pressure measurement is performed. The single CSF sampling conducted as part of this test aims to simulate a shunt effect to assess whether the patient could benefit from permanent CSF drainage. The test is simple to perform and widely used, although controlled studies on it are scarce. As part of the test, 30–50 ml of CSF is typically withdrawn. Improvement in symptoms mainly involves gait disturbances and may occur hours after the puncture and last for days. Standardized gait analyses and cognitive tests are conducted before and after the puncture and evaluated to accurately assess the effect of CSF drainage.
Multi-day lumbar CSF drainage
As an additional diagnostic measure, for example, in cases where the results of the tap test are inconclusive, continuous CSF drainage can be performed over 3 days. Approximately 150–300 ml of cerebrospinal fluid is drained daily, and gait analyses and cognitive tests are conducted and evaluated before and after insertion of the drainage.
CSF infusion test
Cerebrospinal fluid infusion tests involve a continuous volume loading of the CSF space with simultaneous measurement of intracranial pressure, i.e. the pressure inside the skull. After reaching a plateau-like flow equilibrium, the CSF outflow resistance is calculated from the difference between the resting pressure and the plateau pressure, as well as from the infusion rate of the cerebrospinal fluid (Rout in mm Hg/ml/min).
Conceptually, this value directly indicates how much cerebrospinal fluid can be absorbed per unit of time under a given intracranial pressure. The CSF outflow resistance (Rout) is typically elevated in patients with idiopathic normal pressure hydrocephalus (iNPH). An increased CSF outflow resistance serves as a predictive variable for a better surgical outcome.
How is normal pressure hydrocephalus treated?
Meaningful conservative options for the long-term treatment of normal pressure hydrocephalus do not exist. Lumbar punctures can provide temporary relief and contribute to diagnosis and surgical decision-making.
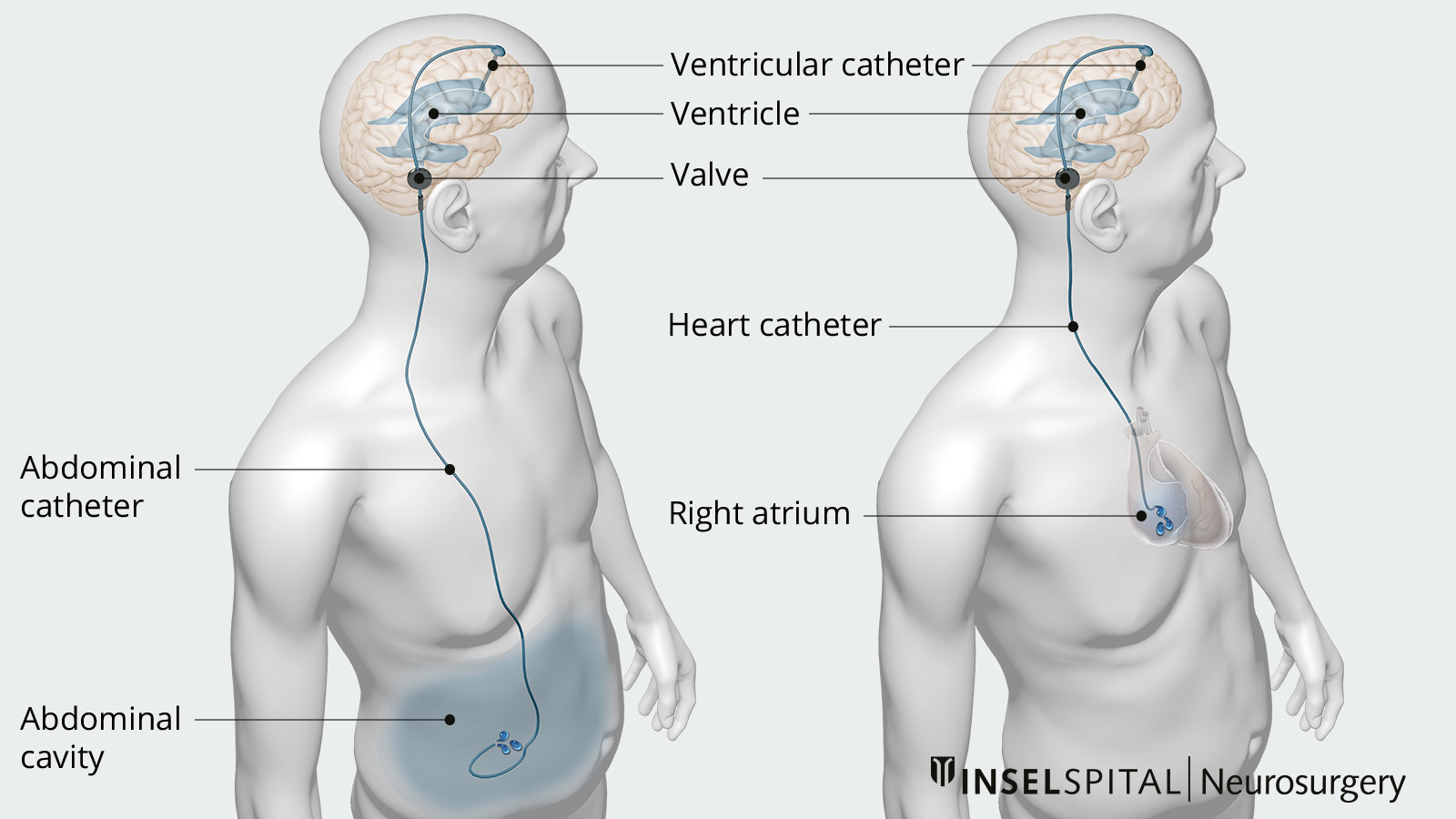
Surgery is the treatment of choice. The treatment principle is to permanently drain the excess cerebrospinal fluid from the cerebral ventricles to an alternative resorptive compartment of the body, typically the abdominal cavity. This is achieved using a device called a ventriculoperitoneal shunt (VP shunt).
Usually, an adjustable valve is implanted behind the ear to regulate the pressure level of CSF drainage. Additionally, a gravitational unit may be implanted to counteract overdrainage in the upright position.
This type of surgery is a standard neurosurgical standard procedure frequently performed worldwide and is associated with a good prognosis, particularly when diagnosed early.
In rare cases, the shunt catheter may be implanted into the right atrium of the heart (ventriculoatrial shunt or VA shunt), or cerebrospinal fluid may be diverted from the lower spinal canal (lumboperitoneal shunt). Selected patients may undergo an endoscopic third ventriculocisternostomy to establish a connection between the internal and external cerebrospinal fluid spaces.
Potential complications include infection, intracerebral hemorrhage, epileptic seizures, and, in the course, disconnection or obstruction.
Why you should seek treatment at Inselspital
In our clinic, we work very closely with colleagues from the Department of Neurology. Our patients receive comprehensive diagnostics and, if necessary, a clear indication for surgical treatment of their normal pressure hydrocephalus. All the above-mentioned treatment procedures are carried out by our specialists with extensive experience and using the latest technical methods.
Shunt therapy provides an effective option for patients. Six months after implantation, 83% of our patients show an objective improvement in walking ability. This is demonstrated through a timed walking test.
-
Fichtner, J., Hni, L., Raabe, A. and ZGraggen, W., 2019. Normaldruck-Hydrozephalus. Swiss Medical Forum ‒ Schweizerisches Medizin-Forum.
-
Momjian S, Owler B, Czosnyka Z, Czosnyka M, Pena A, Pickard J. Pattern of white matter regional cerebral blood flow and autoregulation in normal pressure hydrocephalus. Brain. 2004;127(5):965-972.
-
Krauss JK, Regel JP, Vach W, Droste DW, Borremans JJ, Mergner T. Vascular risk factors and arteriosclerotic disease in idiopathic normal-pressure hydrocephalus of the elderly. Stroke. 1996;27:24–9.
-
Adams R, Fisher C, Hakim S, Ojemann R, Sweet W. Symptomatic Occult Hydrocephalus with Normal Cerebrospinal-Fluid Pressure. New England Journal of Medicine. 1965;273(3):117-126.
Further reading
Brean A, Eide PK. Prevalence of probable idiopathic normal pressure hydrocephalus in a Norwegian population. Acta Neurol Scand. 2008;118:48-53.
Graff-Radford NR, Jones DT. Normal Pressure Hydrocephalus. Continuum (Minneap Minn). 2019;25:165-186.
Greenberg MS. Handbook of Neurosurgery. Thieme; 2016:1664.
Kojoukhova M, Koivisto AM, Korhonen R et al. Feasibility of radiological markers in idiopathic normal pressure hydrocephalus. Acta Neurochir (Wien). 2015;157:1709-18; discussion 1719.
Normaldruckhydrozephalus: Leitlinien für Diagnostik und Therapie in der Neurologie. Deutsche Gesellschaft für Neurologie; 2017
Peterson KA, Savulich G, Jackson D, Killikelly C, Pickard JD, Sahakian BJ. The effect of shunt surgery on neuropsychological performance in normal pressure hydrocephalus: a systematic review and meta-analysis. J Neurol. 2016;263:1669-1677.
Schniepp R, Trabold R, Romagna A et al. Walking assessment after lumbar puncture in normal-pressure hydrocephalus: a delayed improvement over 3 days. J Neurosurg. 2017;126:148-157.
Udvarhelyi GB, Wood JH, James AE, Bartelt D. Results and complications in 55 shunted patients with normal pressure hydrocephalus. Surg Neurol. 1975;3:271-275.