Spinal cord stimulation (SCS) is an alternative procedure for treating chronic back and leg pain which is used when conservative and surgical treatment options have been exhausted and have not provided sufficient relief from pain. Spinal cord stimulation relieves pain through the electrical activation of pain-inhibiting neurons in the brain. The patients' perception of pain is superimposed, and chronic pain is reduced.
When is spinal cord stimulation used?
We use spinal cord stimulation at Inselspital for the following conditions:
Patients with limited quality of life and high levels of suffering who have been treated conservatively, with medication or surgically are the main candidates for this procedure. They are first evaluated by an interdisciplinary team of pain therapists, psychiatrists and neurosurgeons to determine whether they are suitable candidates for spinal cord stimulation.
How does spinal cord stimulation work?
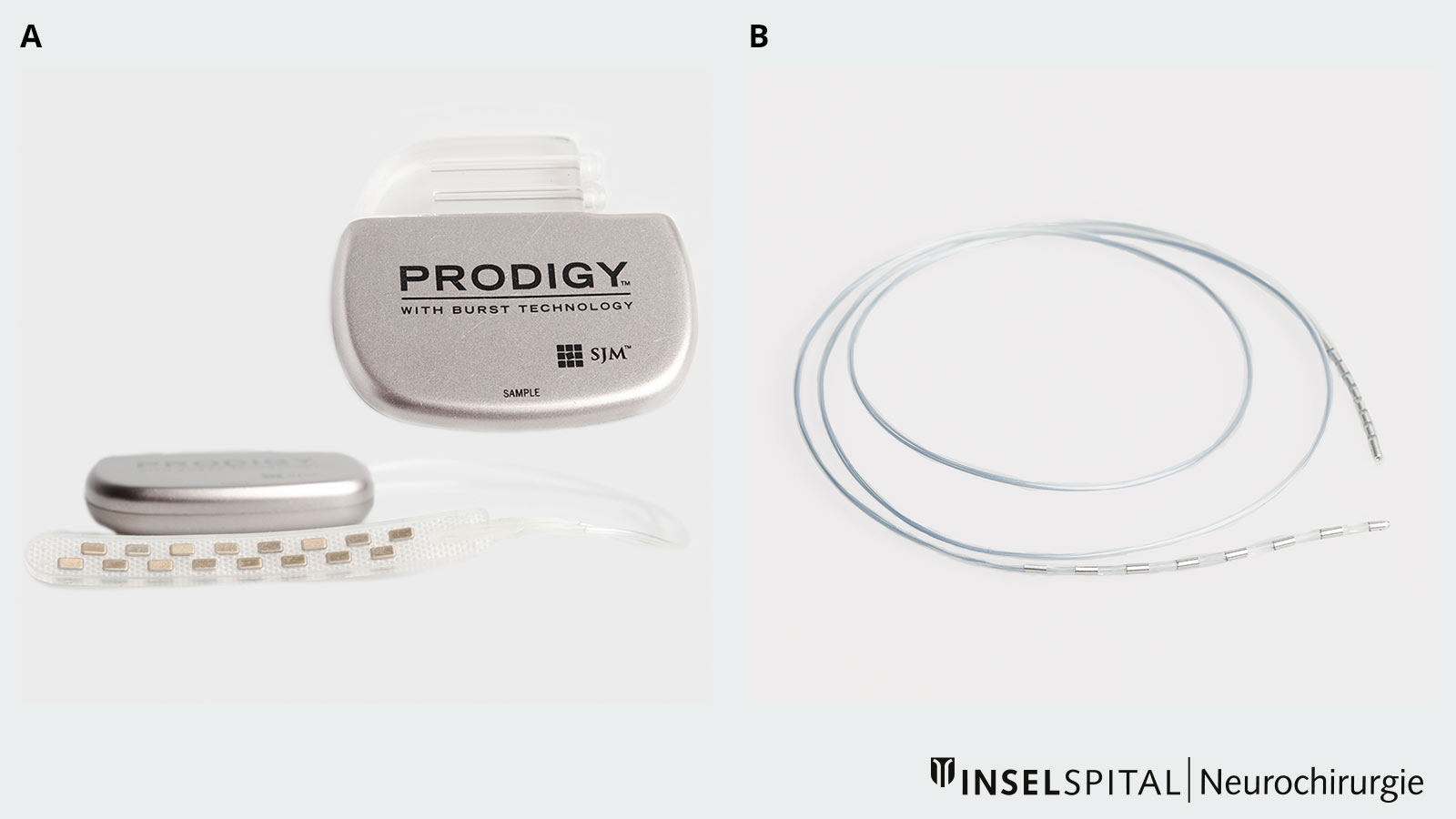
A spinal cord stimulation system consists of two components: neurostimulator and electrodes.
The neurostimulator is used to generate programmed electrical impulses. It is connected under the skin to electrodes (rod or plate electrodes) that the neurosurgeon implants directly onto the spinal cord in a minimally invasive procedure. Through these electrodes, the current is directed to the spinal cord, which leads to a change in pain generation and processing, and subsequently to pain reduction. The patient feels the current as a fine, pleasant tingling sensation, which we doctors call paresthesia.
However, there are now also new forms of stimulation such as high-density stimulation, Burst deep brain stimulation or 10 kHz stimulation that are virtually free of paresthesia.
What is the goal of spinal cord stimulation?
The primary goal is to improve quality of life. This includes:
- a 50% reduction in pain
- Reduction of pain medication
- Improvement in sleep quality
- Increase in physical activity
- reintegration into the work process
- general improvement in psychological well-being
Although freedom from pain can be achieved in rare cases, this is not a realistic goal. Nor is it expected from this therapy.
Before the surgery
Before the procedure, a magnetic resonance imaging (MRI) of the thoracic and lumbar spine is performed.
Furthermore, an appointment at our anesthesia consultation is necessary.
It is also discussed with the patient whether an MRI-compatible system should be implanted and whether the system used will be rechargeable.
We will apply for approval from the health insurance company to cover the costs.
Day of surgery
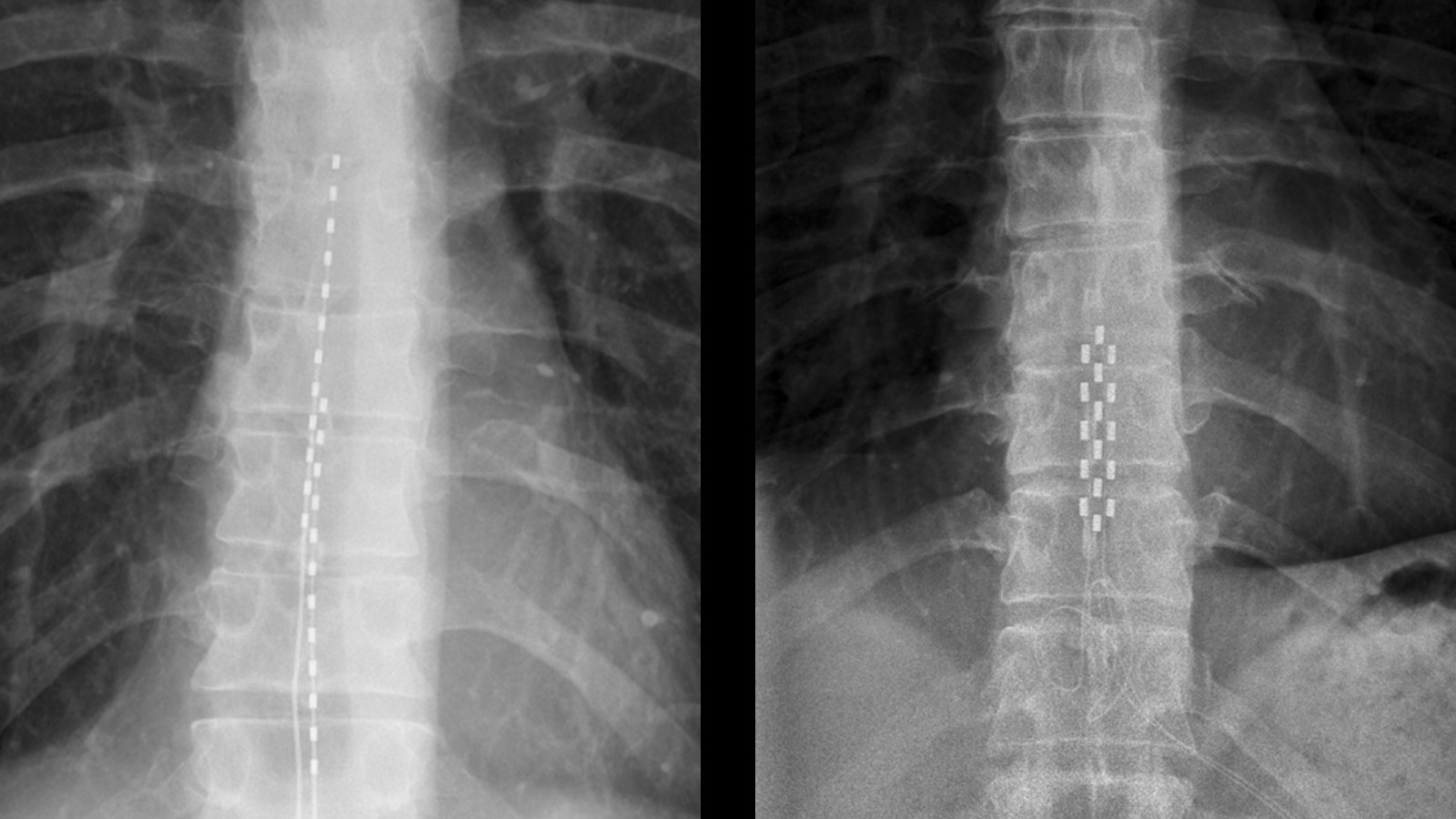
The patient arrives fasting in the morning for the operation. It is usually performed under local anesthesia, but this can be adjusted individually. In the operating room, the electrodes are placed on the spinal cord under X-ray control. During the operation, the patient provides feedback on whether the painful area is well covered by the paresthesia. If the area is covered by at least 80%, the electrodes are connected under the skin to an extension that is led out of the skin in the trunk area. An external test stimulator is connected to this extension. The patient stays overnight in the hospital for monitoring and can go home the next day.
Patients who are candidates for spinal cord stimulation undergo a trial phase before the neurostimulator is definitively implanted. The trial phase lasts one to two weeks. Showering and bathing are not allowed during this time. Home care nursing is arranged for regular dressing changes and wound checks.
If the patient benefits from the stimulation, a definitive implantation of the neurostimulator, also known as the battery, is performed on an outpatient basis. This means the patient comes in the morning for the procedure and can go home in the evening. Before the patient is discharged, an X-ray examination is performed to check the position of the electrodes.
If the patient does not respond to the therapy, the electrodes are removed again.
Aftercare
The patient comes to our clinic after 2 weeks for suture removal and wound control. The stimulator is checked and the stimulation is adjusted. Regular check-ups take place after 6 weeks, 3, 6 and 12 months, then at annual intervals. When the battery is empty, it must be replaced by a small operation under local anesthesia.
What are the complications?
The complication rate is low. However, as with any procedure, complications can occur.
In the early phase
- Bleeding, which can lead to temporary or, rarely, permanent paralysis and require surgical relief
- Infections during the test phase
- Electrode displacements
- Connection problems of the electrodes with the battery
- Battery malfunctions
In the late phase
- Loss of effect of stimulation
- Infections
- Electrode displacement
- Electrode breakage
- Cable breakage
- Battery malfunctions
- Pain in the area of the battery pocket
What are the chances of success?
According to literature, the long-term success rate is about 70–80 %. The earlier spinal cord stimulation is performed, the higher the chances of success.
In about 20–30 % of patients, a loss of effect may occur over time - due to a habituation effect. 60 % of these patients can benefit again from spinal cord stimulation by using newer forms of stimulation such as high-density stimulation, Burst deep brain stimulation or 10 kHz stimulation.