Craniopharyngeomas are tumors that usually develop in the area of the pituitary gland (hypophysis). A craniopharyngeoma develops from cell remnants from the embryonic period and therefore often occurs in children. Although craniopharyngeomas are benign and grow slowly, they may be heavily fused with surrounding structures such as the pituitary gland, pituitary stalk, optic nerves, and vessels.
How common is a craniopharyngeoma and who is affected?
Craniopharyngeomas account for approximately 2.5–4 % of all brain tumors. About half of craniopharyngeomas occur in childhood, the majority between the ages of 5 and 10. The other half of these tumors are found in adults, mostly after the age of 40. Women and men are affected with equal frequency.
What are the causes of craniopharyngeoma?
Craniopharyngeomas develop when residual cells of the Rathke's pouch suddenly proliferate. The Rathke's pouch is a structure from the embryonic development of the pituitary gland that normally regresses.
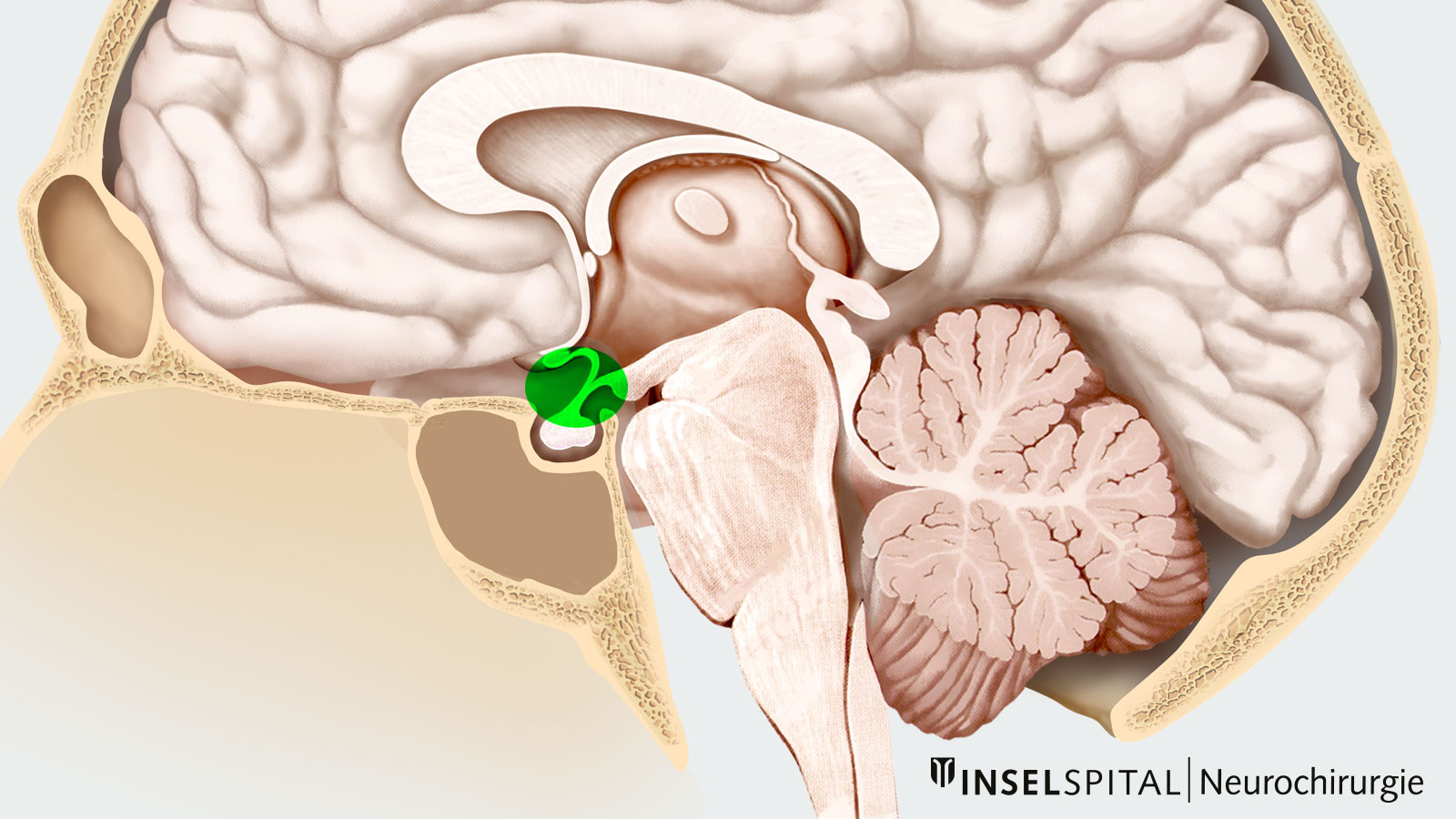
Craniopharyngeomas usually arise in the region of the pituitary stalk and may extend from there in different directions (suprasellar, parasellar, or sellar). A minority of craniopharyngeomas (about 5%) grow purely intraventricular (in the 3rd ventricle).
Physicians distinguish two forms of craniopharyngeomas based on their fine tissue structure:
- Adamantine craniopharyngeoma is more common in children, is often hard and calcified, and has a higher risk of recurrence.
- Papillary craniopharyngeoma occurs mainly in adults, is extremely rarely calcified, and has a lower risk of recurrence.
What symptoms does a craniopharyngeoma cause?
Because of the close proximity to the optic nerves, the junction of the optic nerves called the optic chiasm, the pituitary gland, the pituitary stalk, the hypothalamus (part of the diencephalon), and the brainstem, a whole range of symptoms can occur:
- headache
- visual disturbances and/or visual field restrictions
- hormonal disorders, especially diabetes insipidus (increased drinking and excretion, thirst)
- nausea and vomiting
- neurocognitive deficits
- hypothalamic disorders, especially weight gain
How is a craniopharyngeoma diagnosed?
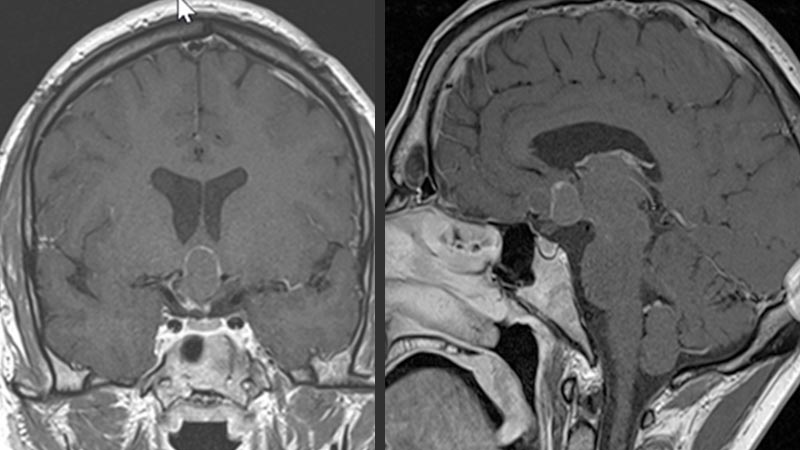
Magnetic resonance imaging (MRI) with contrast medium is the diagnostic procedure of first choice. The MRI image provides information about the localization and extent of the tumor.
Sometimes a complementary computed tomography (CT) scan is helpful to assess the presence of calcifications.
In all patients with suspected craniopharyngeoma, an endocrinologic workup is recommended to diagnose and treat possible hormonal imbalances.
Ophthalmologic examination becomes necessary if the MRI image shows that the tumor is in contact with the optic chiasm, the site where the optic nerves of the eyes cross.
How is a craniopharyngeoma treated?
Due to their displacing growth, the tumors can lead to permanent damage of the surrounding brain structures. The treatment of choice is therefore complete surgical resection of the tumor. If complete resection is not possible due to proximity to important surrounding structures, concomitant radiotherapy or radiosurgery should be discussed to reduce the risk of recurrence.
Medical research is also currently working on the development of chemotherapeutic agents as a complementary therapy. Currently, drugs are being tested for the therapy of papillary craniopharyngeoma. These are so-called BRAF inhibitors such as vemurafenib and dabrafenib.
There are two surgical approaches for craniopharyngeoma surgery:
- the transcranial approach
- the transnasal transsphenoidal approach
For classic craniopharyngeomas, both the transcranial and transnasal transsphenoidal approaches can be chosen.
With transcranial approach, an opening is made in the skull, a so-called craniotomy. The tumor can then be removed microsurgically. This is the recommended technique, especially for purely intraventricular craniopharyngeomas that lie completely or partially in the cerebral ventricles (ventricles) or for tumors that show extensive growth.
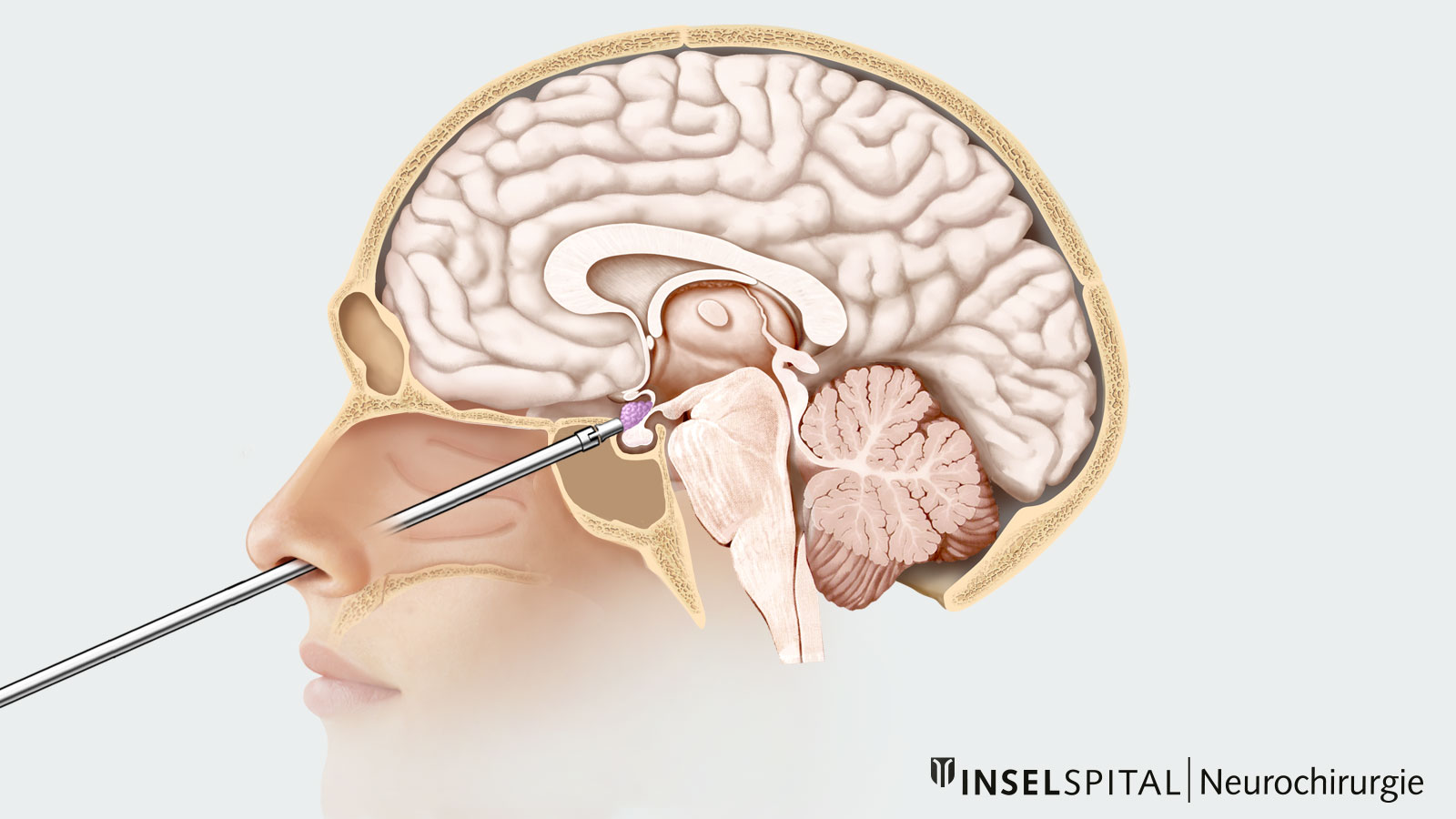
In the transnasal transsphenoidal approach, the surgical access route is through the nose.
Possible complications after resection of a craniopharyngeoma are mainly disturbances of the electrolyte and hormone balance. These disturbances may be temporary or permanent. In the postoperative period, blood values and water balance are closely monitored. If necessary, a hormone deficiency must be replaced with medication.
Why you should seek treatment at Inselspital
Our specialized neurosurgical team has many years of surgical experience in the operation of craniopharyngeomas. Depending on the location and extent of the tumor, we offer our patients the safest and most effective surgical technique
.Neurosurgery at Inselspital works closely with the specialist departments of endocrinology, ophthalmology and radio-oncology. In this way, we can guarantee you comprehensive and high-quality care – before, during and after surgery.
In addition, each case is discussed within the framework of our interdisciplinary pituitary board and neuro-oncological tumor board, where neurosurgeons work together with endocrinologists, oncologists and radiation oncologists to develop an individualized treatment plan tailored to each patient.
Further reading
- Greenberg MS. Handbook of Neurosurgery. Thieme; 2016:1664.
- Komotar RJ, Starke RM, Raper DMS, Anand VK, Schwartz TH. Endoscopic endonasal compared with microscopic transsphenoidal and open transcranial resection of craniopharyngiomas. World neurosurgery. 2012;77:329-341.
- Liubinas SV, Munshey AS, Kaye AH. Management of recurrent craniopharyngioma. Journal of Clinical Neuroscience. 2011;18:451-457.
- Minamida Y, Mikami T, Hashi K, Houkin K. Surgical management of the recurrence and regrowth of craniopharyngiomas. Journal of neurosurgery. 2005
- Moussazadeh N, Prabhu V, Bander ED et al. Endoscopic endonasal versus open transcranial resection of craniopharyngiomas: a case-matched single-institution analysis. Neurosurgical Focus. 2016;41:E7.
- Müller HL. Craniopharyngioma. Endocrine reviews. 2014;35:513-543.
- Ottenhausen M, Rumalla K, La… EC. Treatment strategies for craniopharyngiomas. Journal of Neurosurgical Sciences. 2017