The operating area with 4 state-of-the-art operating rooms is the heart of our clinic. Our surgical team includes anesthetists, experts in anesthesia and positioning care as well as highly qualified operating surgical nurses who guarantee professional assistance during operations.
Our status as a university hospital and surgical center allows us to be equipped with the latest technologies. We can therefore introduce new surgical techniques at an early stage and provide innovative intraoperative procedures with the necessary experience.
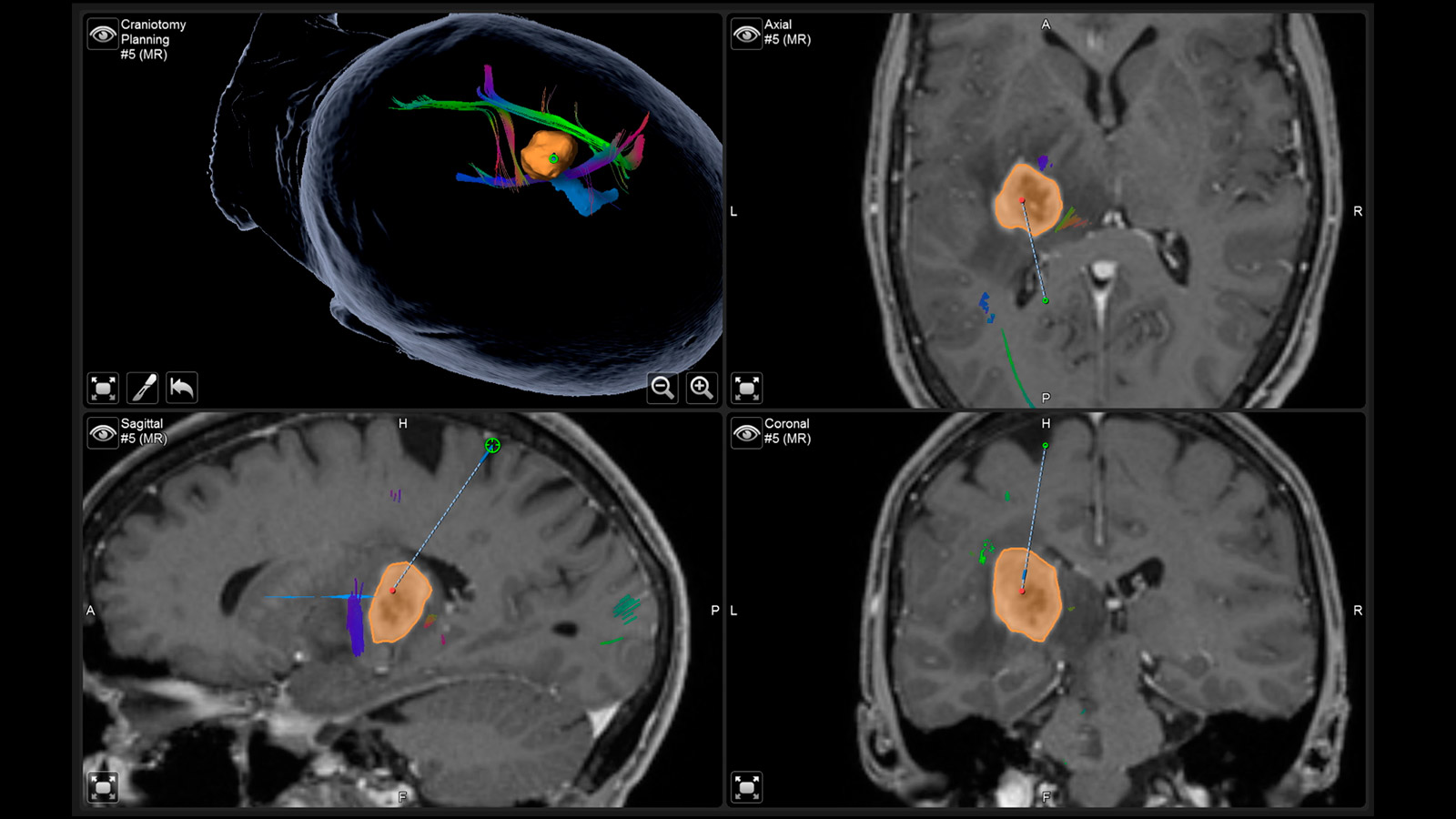
The advent of computers and navigation in the operating room, the use of microscope and endoscope, and the ever-improving imaging even during an intervention allow for submillimeter surgical precision. Functional neuronavigation, fiber tracking and pathway navigation, intraoperative imaging such as ultrasound, 5-ALA fluorescence and indocyanine green infrared angiography or electrophysiological techniques such as mapping and SEP-/MEP-/D-Wave monitoring are now indispensable in the OR. The latter procedures in particular have become indispensable for us in many operations from the point of view of safety.
The further development and perfection of intraoperative techniques is an essential prerequisite for cutting-edge medicine and an important research focus of our clinic, for which we are also internationally recognized.
Intraoperative Imaging
Methods for imaging during surgery, such as ultrasound, fluorescence techniques, but above all imaging examinations such as computer tomography (CT) or magnetic resonance imaging (MRI) using large devices with the best image quality play a special role. In contrast to the subjective assessment of the surgeon, intraoperative imaging allows an objective representation of the success of the operation and is thus the highest quality control.

The Inselspital concept: high-precision surgery
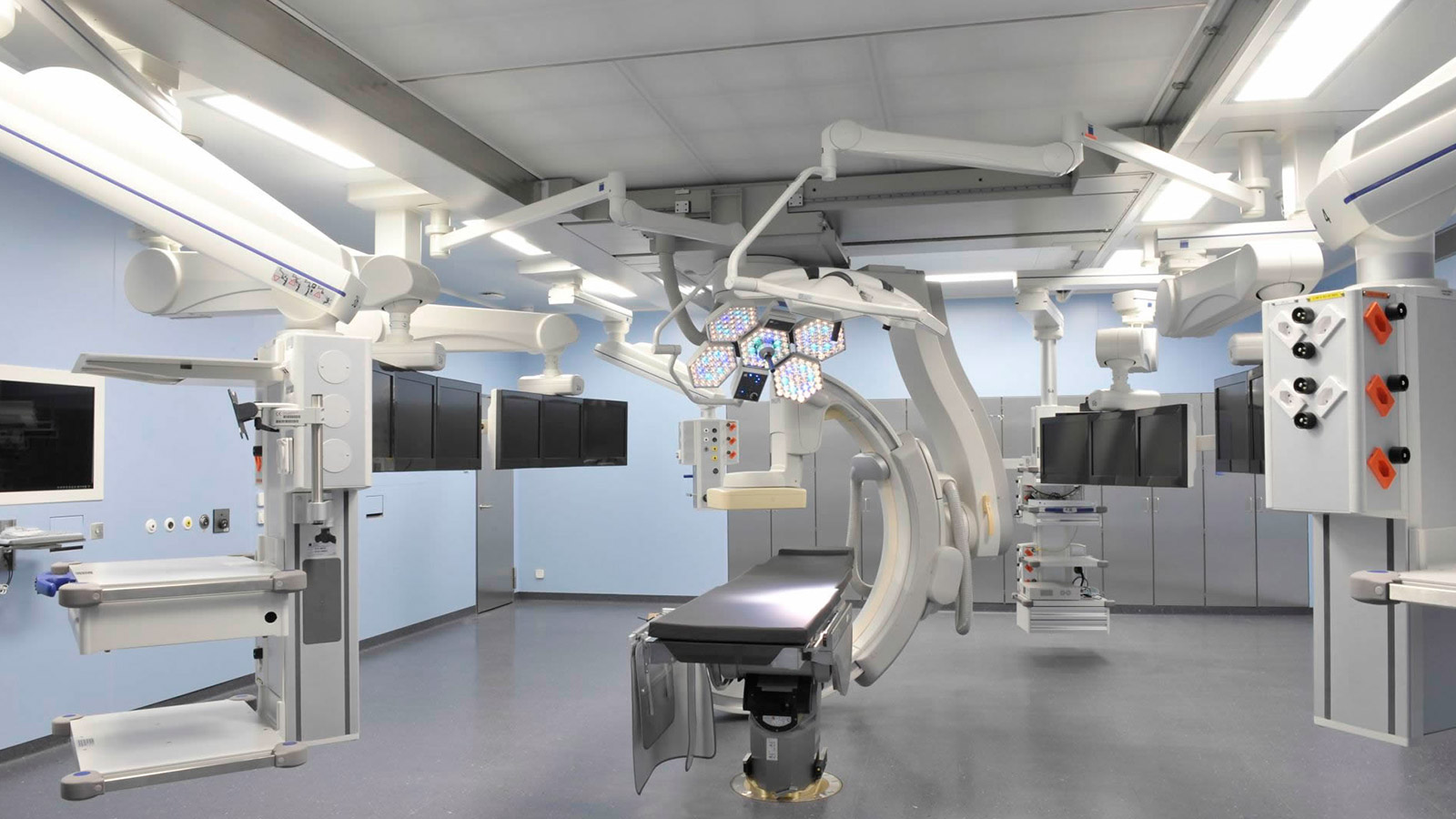
At Inselspital, a surgical concept has been implemented that allows each specialty to perform optimal imaging during surgery. For this purpose, all 3 major modalities were installed: MRI, CT, and angiography. These high-precision rooms are used jointly and variably as needed. Each device in the operating rooms is linked to a navigation system. This platform was deliberately designed to be open to allow for research and development of new innovative surgical procedures.
Why is intraoperative imaging useful in special cases?
Both tumors and functions in the brain are often not visible and localizable for the surgeon with the bare eye or under the operating microscope. Incisions are made on the spine, cages are placed or screws are inserted at depths that are no longer visible to the surgeon. Despite the most careful planning, residual tumor tissue can remain after an operation, or a screw or cage can be placed incorrectly. For this reason, the control with imaging after the operation is often a standard procedure and can lead to the decision to perform a revision surgery if the findings are appropriate. In selected operations, it makes sense to perform this result check during the operation when a correction of the result is still possible.
However, imaging with CT, MRI or intraoperative digital subtraction angiography is only used in special operations where there is a certain probability of a suboptimal result despite the best planning. This direct effect on the quality of the operation is not to be expected in every operation, but rather helps to increase the rate of surgeries with optimal results.
Intraoperative computed tomography (iCT)
An iCT is used to visualize bony structures. This most frequently concerns operations on the spine. Here, the surgeon often has to place screws in the biomechanically most stable part of a single vertebra in order to achieve short- or long-range position correction and stabilization. Intraoperative imaging helps to place these screws optimally and to monitor other corrective steps.

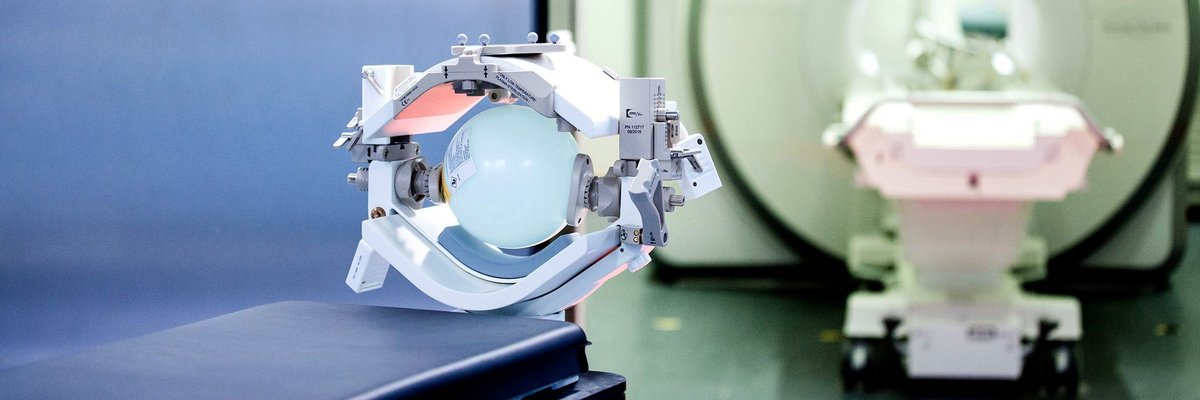
Intraoperative magnetic resonance imaging (iMRI)
Intraoperative MRI is the procedure we use most frequently in brain tumor surgery. Although every operation is carried out with precise pre-planning and navigation, thus making the patient «transparent», parts of the brain are displaced during the operation because tumor tissue is removed. Therefore, at the end of the operation, residual tumor may remain in the depths if it is not visible. An iMRI is used for real-time imaging and can reveal possible residual tumor. With the updated images, the surgeon is guided to this spot with pinpoint accuracy, again controlled by navigation.

Intraoperative digital subtraction angiography (iDSA)
The imaging of vessels and vascular diseases with contrast medium during surgery is used to assess whether, for example, an aneurysm or an arteriovenous malformation has been completely eliminated and the normal brain vessels have remained unaffected. Especially in complex findings, this method leads to a correction of the clip that closes the aneurysm in 20% of cases. An operating room with iDSA is also called a hybrid OR because cardiology and heart surgery or neurosurgery and neuroradiology can each operate together.
Operating with neuronavigation
Neuronavigation is a computer-assisted procedure that allows neurosurgeons to precisely plan an operation and orient the patient with millimeter accuracy during surgery on the brain, skull base or spine.
Operating with augmented reality
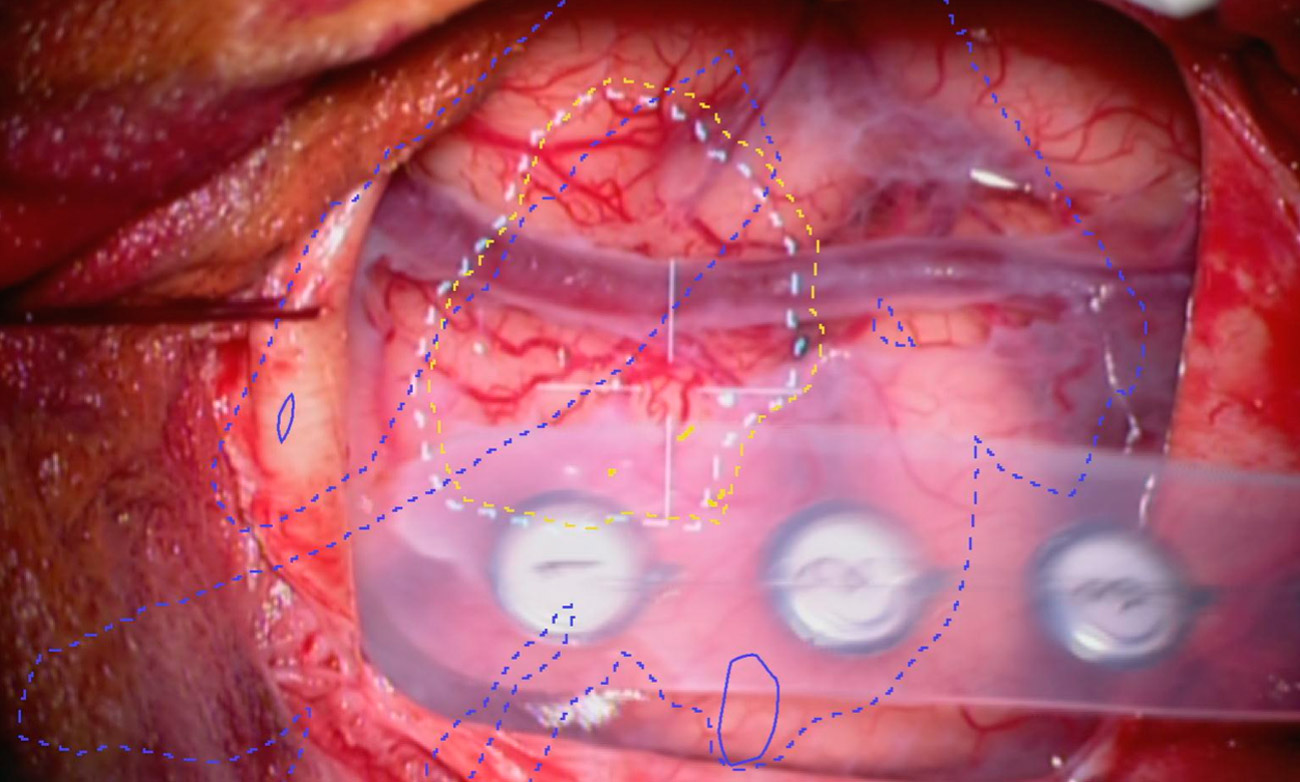
Augmented reality (AR) is one of the modern and innovative surgical techniques used and further developed at our neurosurgery center. With the help of this computer-assisted enhancement of reality perception, the neurosurgeon can orient himself better and operate more precisely.