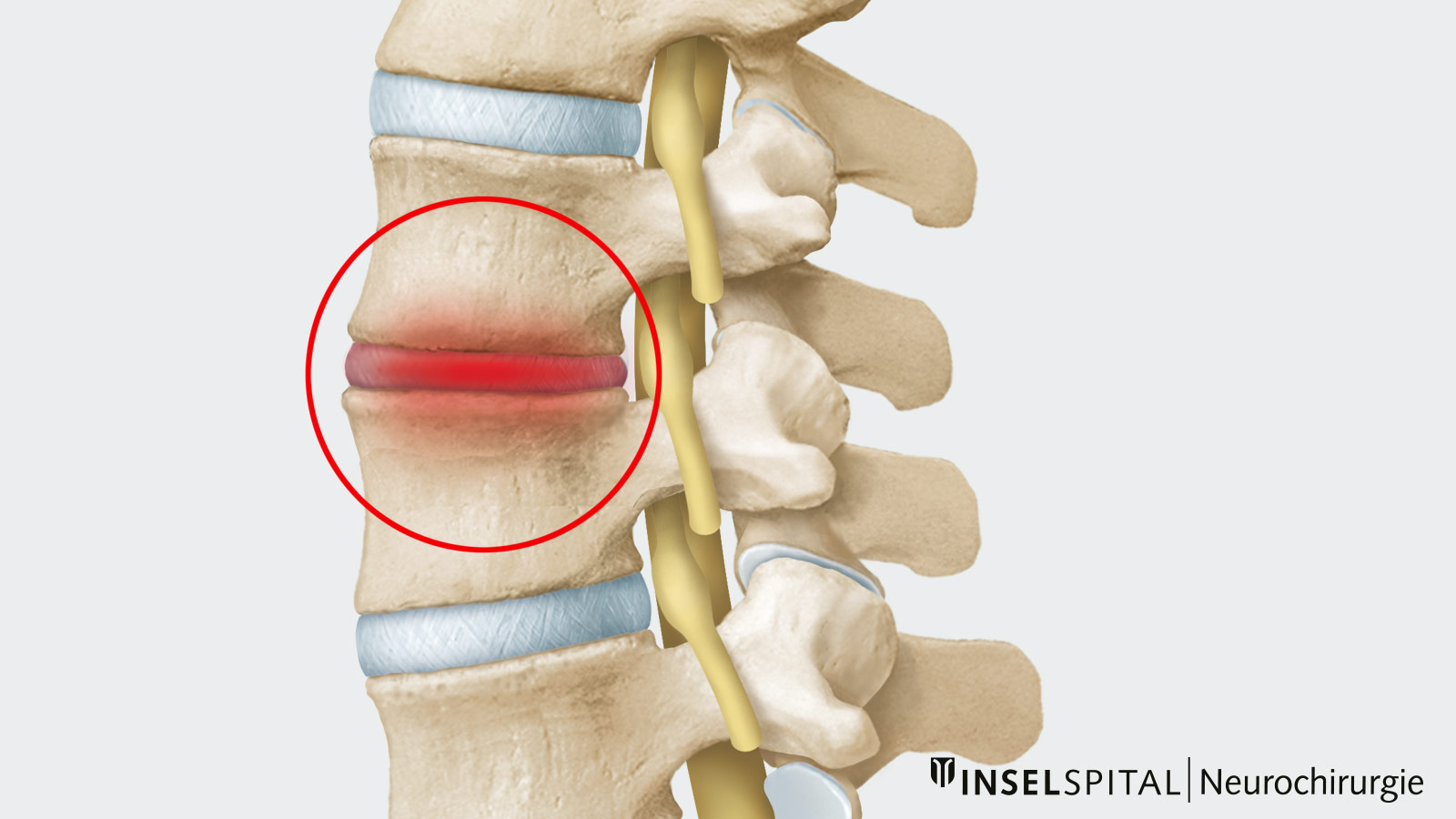
Spondylodiscitis is an infection of an intervertebral disc and adjacent vertebrae, usually caused by bacteria. It leads to severe load-dependent back pain. If nerve roots are affected, leg pain and neurological deficits may also occur. In addition to targeted antibiotic therapy, treatment in advanced cases requires stiffening of the affected vertebrae (spondylodesis) to immobilize the mobile segment.
What is the cause of spondylodiscitis?
Bacteria are usually responsible for the infectious infestation of the intervertebral disc and adjacent vertebrae. These bacteria can spread via the bloodstream from distant entry points and infection sites (e.g. mouth and throat, skin, lungs) to the heavily perfused spinal column, where they can become established.
Furthermore, bacterial spondylodiscitis can also be caused by previous spinal surgery, mainly if foreign material (screws and implants) was used. In these cases, skin bacteria most frequently settle in the wound or even on the implants. Chronically ill patients, immunosuppressed or immunocompromised patients have an increased risk of developing spondylodiscitis.
What are the symptoms of spondylodiscitis?
In most cases, load- and movement-dependent pain first occurs in the area of the affected spinal segment. The pain can be very pronounced, and patients are increasingly restricted in their mobility as a result. If an accumulation of pus in the spinal canal presses on the nerve roots or the spinal cord, there are also corresponding neurological deficits:
- radiating pain in the arms (in the case of the cervical spine)
- radiating pain in the legs (in the case of the lumbar spine)
- paralysis
- sensory disturbances in the area of arms and/or legs
In addition, there is often a general feeling of malaise and illness with fever and chills.
How is spondylodiscitis diagnosed?
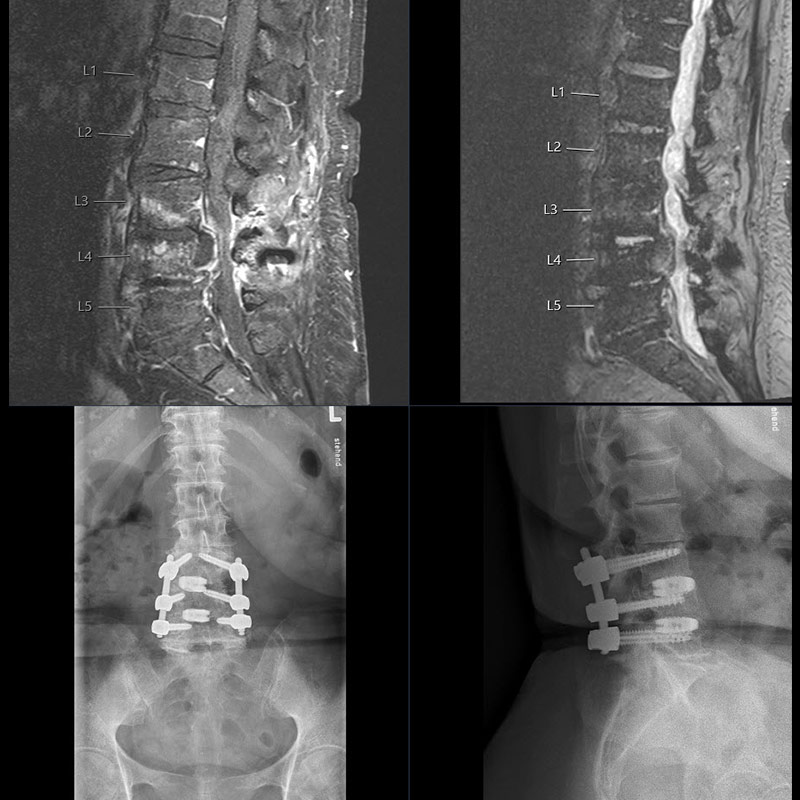
In addition to a detailed questioning on the medical history by the physician, a thorough physical examination is performed. Already after this, the suspected diagnosis of spondylodiscitis can be made. Analysis of the inflammatory levels in the blood also provides information about the presence of an infection. Thanks to blood cultures, the causative bacteria can be identified, which is necessary for targeted antibiotic therapy. The diagnosis can usually be confirmed after magnetic resonance imaging (MRI). A computed tomography (CT) scan can be added for a more accurate assessment of possible bone damage.
It is also important to clarify the cause of spondylodiscitis if previous spinal surgery is not a possible trigger. This includes, for example, a thorough examination of the skin (search for an entry point for bacteria), the throat and teeth, and a cardiac examination (question of bacterial infestation of the heart valves) using ultrasound (echocardiography). In the case of negative blood cultures, small pus collections can be punctured to identify the causative germ.
How is spondylodiscitis treated?
In bacterial spondylodiscitis, targeted antibiotic therapy at the beginning of treatment plays the most crucial role.
In advanced cases with larger pus accumulations and an infestation of the spinal canal, surgery is usually necessary to remove these accumulations and to free nerves. In this case, the infected tissue is examined in the laboratory, and the causative germs can usually be detected.
In very advanced cases or patients with severe pain, the infected disc must be removed, and the affected vertebrae stabilized using a screw-rod system. In place of the infected disc, antibiotic-impregnated bone substitute material with a titanium implant is used. In pre-operated patients, the infected foreign material usually has to be removed and, if necessary, replaced by new material.
Why you should seek treatment at Inselspital
The chosen treatment strategy and the duration and type of antibiotic therapy are, in each case, tailored to the individual patients and their disease course. Infectious disease specialists are consulted at an early stage in the clarification and treatment of patients with spondylodiscitis.
