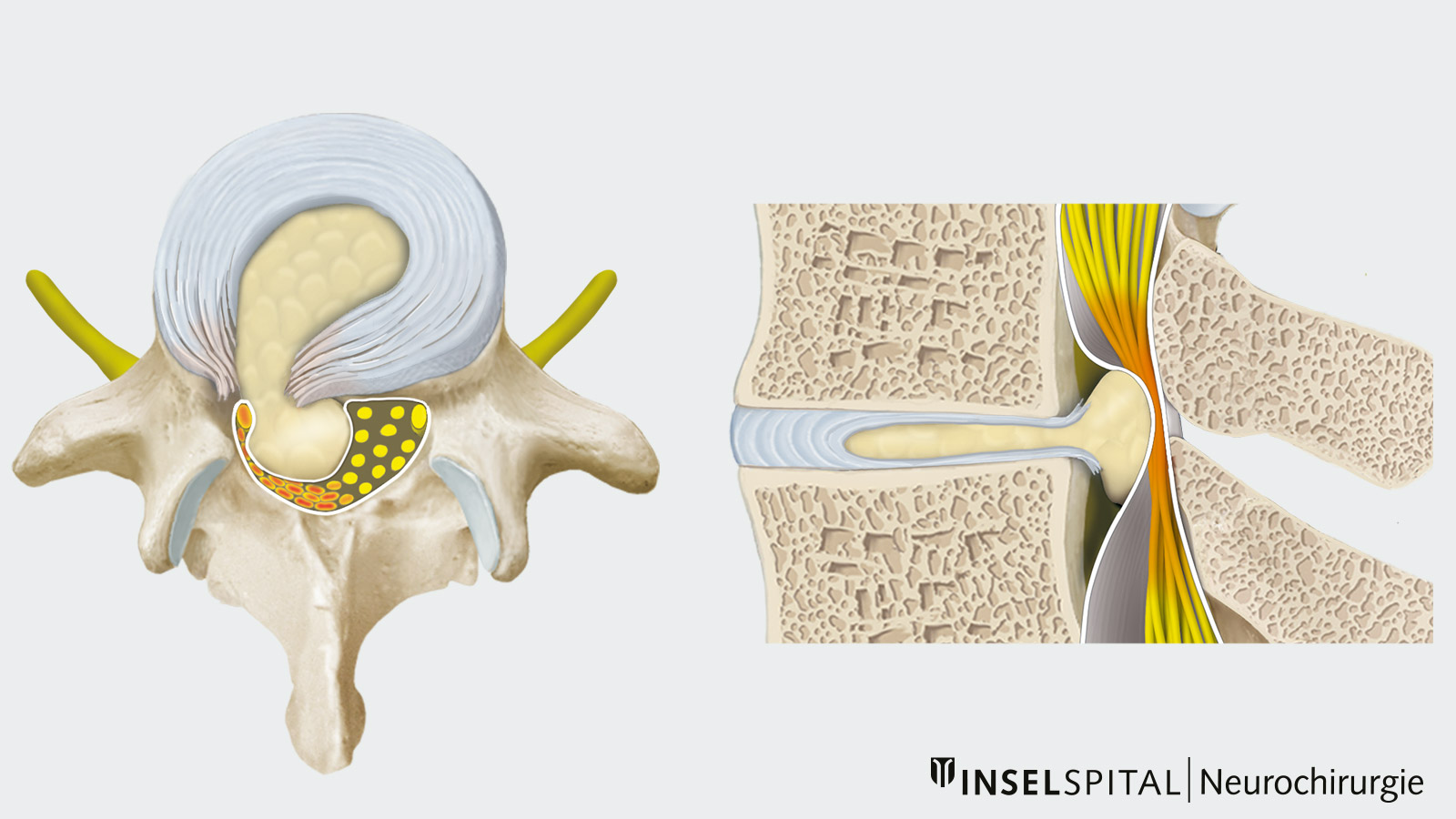
The herniated disc of the lumbar spine, also known as lumbar disc herniation or lumbar disc hernia, is the most frequent disc herniation, as the total weight of the spinal column rests most heavily on the two lowest discs. Tears in the fibrous ring allow tissue from inside the disc to protrude into the spinal canal where it presses on nerves. A typical symptom is an sciatic nerve pain that extends over the buttocks and the outside of the leg to the foot. Most herniated discs improve within 6–12 weeks on their own or with conservative therapy (pain medication and careful physiotherapy). However, if there is no improvement, paralysis or severe pain, microsurgical removal of the herniated piece of tissue should be performed. In 95% of all patients, surgical intervention brings immediate improvement.
Our experience at Inselspital
At the Back Center of Inselspital, specialists from all disciplines work closely together under one roof and coordinate with each other. Thanks to the cooperation of rheumatology, physiotherapy, neurology, neuroradiology, pain center and orthopedics on a daily basis, the optimal treatment strategy can be developed for our patients. Complicated cases are discussed in an interdisciplinary board and often operated on jointly by neurosurgeons and orthopedists. In this way, we create the conditions for the best possible treatment for each individual patient.
Minimally invasive intervertebral disc surgery for the quick and gentle relief of a compressed nerve is one of the most common interventions at our clinic and can also be performed on an outpatient basis if desired. The operation leads to a better result than on-going conservative treatment, which has not brought any improvement after 6–12 weeks. This was investigated by two independent American studies *, *.
Our nursing staff and physiotherapists know the treatment and aftercare following a herniated disc very well and pave the way for a speedy recovery. Because the right behavior is essential after a herniated disc, we have compiled useful information for our patients, especially on correct lifting and carrying, exercises for back training and a special video for the time after surgery.
Lumbar disc problems are common, but they rarely require surgery. More than 90% of disc protrusions or disc hernias with pain extending into the leg improve with rest, warmth, pain medication, relief positioning, physiotherapy and local infiltration. It is also important to distinguish a lumbar disc pain from lower back pain in lumbago. This is caused by irritation of the vertebral joints or ligamentous structures and there is no pain in the leg. Here, rest is even less indicated, as exercise is part of the therapy and leads to a faster recovery.
Whenever possible, we recommend 6–12 weeks of conservative therapy for herniated discs. We often observe that the symptoms only improve significantly in the second half of the treatment period. So it is worth persevering.
Who belongs to the risk group for a lumbar disc herniation?
Herniated discs occur more frequently in the fourth and fifth decades of life, but can occur at any age. 2–3% of the population will experience a lumbar disc herniation that causes symptoms in their lifetime. Studies have shown that the risk of a herniated disc is higher in smokers. Other causative factors are constant strain on the spine and a genetic predisposition.
Which are the most frequent symptoms?
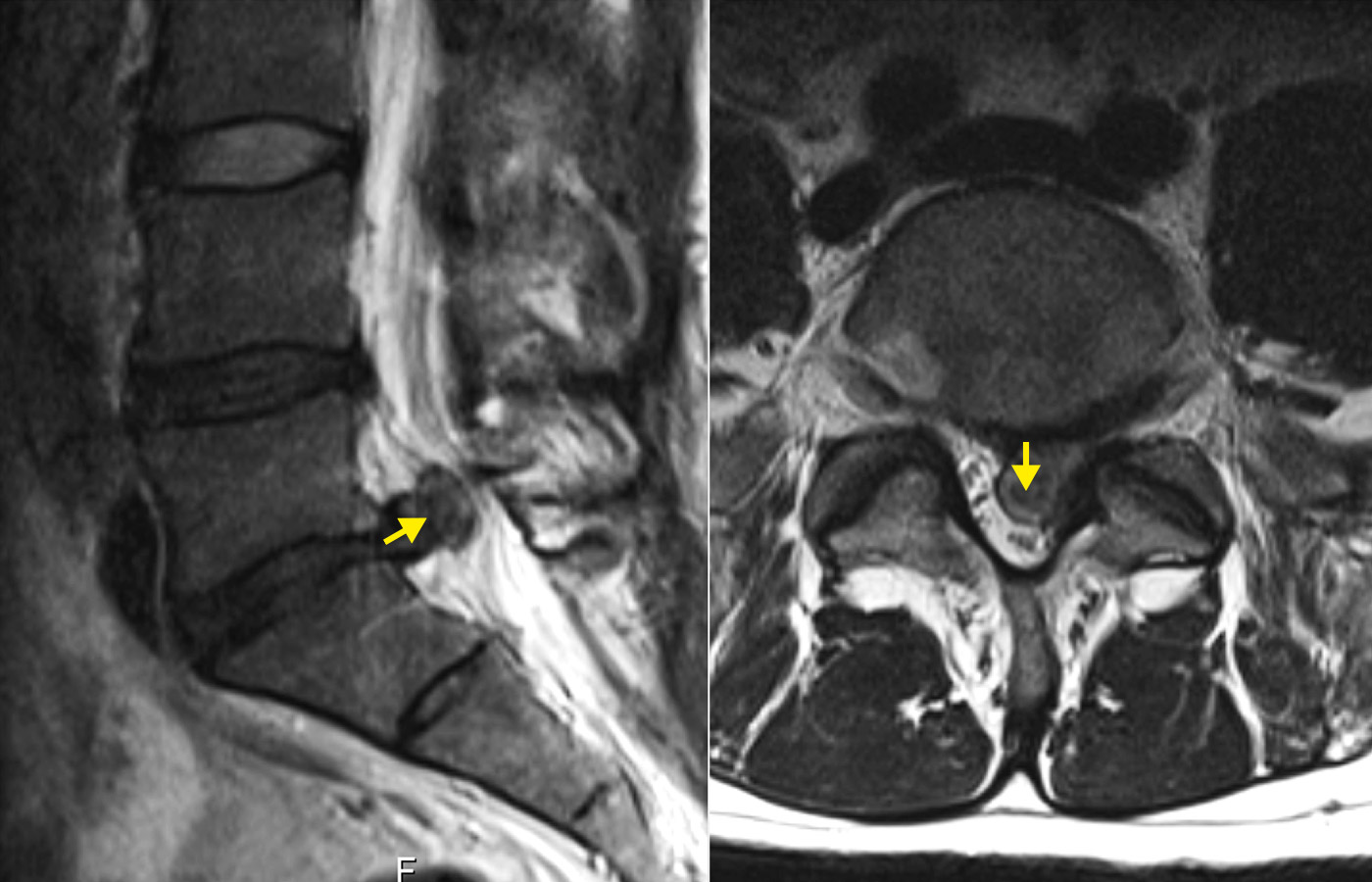
Disc hernias occur most frequently between the 4th and 5th lumbar vertebrae and between the 5th lumbar vertebrae and the coccyx. Depending on the direction of the prolapsing disc material, the superior (exiting) nerve or the inferior (traversing) nerve on the way to the neuroforamen can be affected. The pressure of the intervertebral disc on the nerves leads to corresponding irritations and signs of failure. Typical symptoms are radiating pain in the sensitive area of the skin (dermatome) of the respective nerve as well as paralysis or sensory disturbances like numbness. In addition, most patients complain of more or less severe back pain in the lumbar region (lumboischialgia).
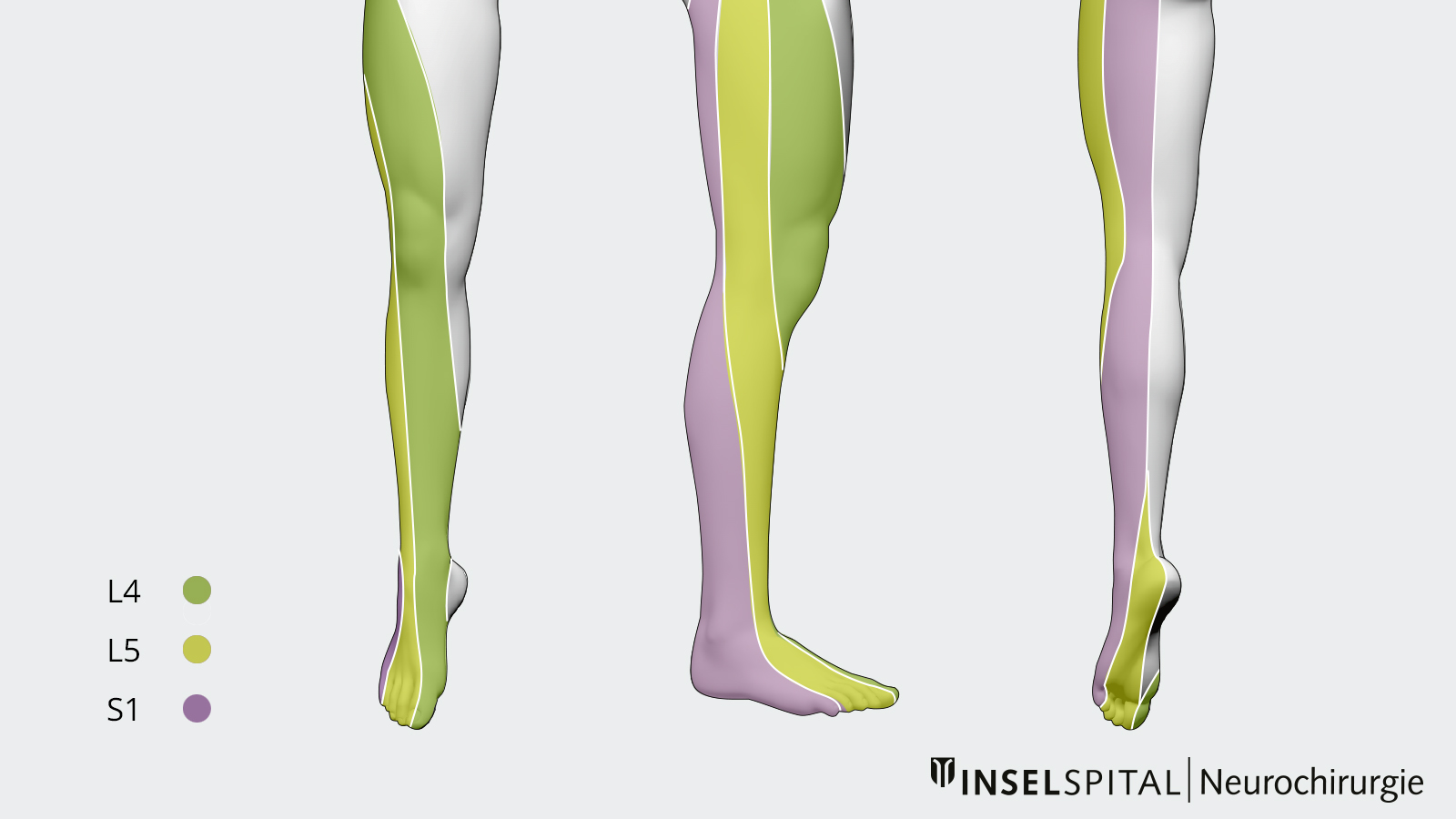
Because each nerve root exiting in the spinal column supplies a different characteristic dermatome (skin area) and myotome (muscle area), the disturbances that occur can ususally by used to determine exactly which nerve root is affected.
In the case of very large herniated discs, all the nerve roots running in the lumbar spinal canal can be affected. This so-called cauda equina syndrome is particularly threatening because it can cause disorders of the bladder and rectal and sexual functions. Cauda equina syndrome is always a neurosurgical emergency that must be operated on immediately after radiological confirmation. Otherwise, there is a risk of permanent nerve damage with corresponding loss of function.
Localization of the herniated disc based on symptoms
Typical findings for the nerve root are:
- L4: Pain in the thigh down to the knee, numbness in the front of the thigh and the inside of the lower leg, no strength when climbing stairs (knee extensor).
- L5: Pain in the buttocks and in the outer edge of the thigh down to the foot, numbness in the big toe of the foot, weakness of the foot lift, especially the big toe lift (heel stand).
- S1: Pain in the buttocks and in the back of the leg down to the foot, numbness in the outer edge of the foot and in the little toe, weakness of the foot drop (toe stand).
This list is not complete.
How is a lumbar disc herniation diagnosed?
A detailed anamnesis and careful clinical examination are decisive in the initial clarification of complaints in the area of the lumbar spine. If back pain in the lumbar spine is the only symptom, further radiological diagnostics can initially be dispensed with. In this case, conservative therapy may be considered, since in most cases the complaints disappear after a few weeks. Imaging is only required if the symptoms persist or if there are neurological deficits. Magnetic resonance imaging (MRI) is best suited for the diagnosis, as the intervertebral discs and nerve roots can be well visualized. Only in special cases does further clarification by means of electrophysiological examinations or CT myelography become necessary.
What is the surgical procedure?
If there is severe pain, a weakness in the muscles or failure of therapy, surgery should be performed. The procedure usually lasts 15–45 minutes and is performed with a 2–3 cm long skin incision. The intervertebral disc is usually accessed through a tube – this is called a tubular approach. After the operation, you will receive comprehensive care from our physiotherapists. You will also get a booklet with post-discharge instructions.
A 2–3 day inpatient stay in the hospital is usual, but the surgery can also be performed on an outpatient basis if desired.

Despite the high rate of spontaneous healing, surgery for a lumbar disc hernia is the most common surgical intervention on the lumbar spine. The field of neurosurgery has specialized in this condition for many years. The operation is routinely performed using a microscope. This surgical technique is known as microsurgery. The advantages of microsurgery for the patient are obvious: a smaller operation with a gentle approach, a more targeted exposure of the surgical site, less scarring and a greater degree of safety.
In 95% of the patients, the operation leads to an immediate improvement of the symptoms. However, recurrences can occur in 5–20% of patients, when pieces of the intervertebral disc escape into the spinal canal again. This usually depends on the size of the tear in the fibrous ring and less on whether the incident was treated with medication or surgery. When a recurrence happens, individual counseling and therapy is particularly important in order to achieve a good long-term result for the patient. The treatment options range from another minimally invasive microsurgical operation to immobilization and fusion of two vertebrae, especially after repeated discs herniations.
General information on the widespread disease of herniated discs can also be found under the keyword herniated disc.
Further reading
- Weinstein JN, Lurie JD, Tosteson TD et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT) observational cohort. JAMA. 2006;296:2451-2459.
- Vialle LR, Vialle EN, Suárez Henao JE, Giraldo G. LUMBAR DISC HERNIATION. Rev Bras Ortop. 2010;45:17-22.
- Heindel P, Tuchman A, Hsieh PC et al. Reoperation Rates After Single-level Lumbar Discectomy. Spine (Phila Pa 1976). 2017;42:E496-E501.
-
Lurie JD, Tosteson TD, Tosteson AN et al. Surgical versus nonoperative treatment for lumbar disc herniation: eight-year results for the spine patient outcomes research trial. Spine (Phila Pa 1976). 2014;39:3-16.
-
Bailey CS, Rasoulinejad P, Taylor D et al. Surgery versus Conservative Care for Persistent Sciatica Lasting 4 to 12 Months. N Engl J Med. 2020;382:1093-1102.