If the neurosurgeon knows precisely where the functional areas of the brain are located prior to brain surgery, he can plan the procedure safely and minimize the risk of possible consequential damage. Such brain mapping is possible with the help of navigated transcranial magnetic stimulation (nTMS). This is a non-invasive, neurophysiological technique that can be used to locate important functions in the brain with millimeter precision, as if on a map. For example, it shows exactly where the area of the brain responsible for motor function is located and how far it is from a tumor.
What is transcranial magnetic stimulation (TMS)?
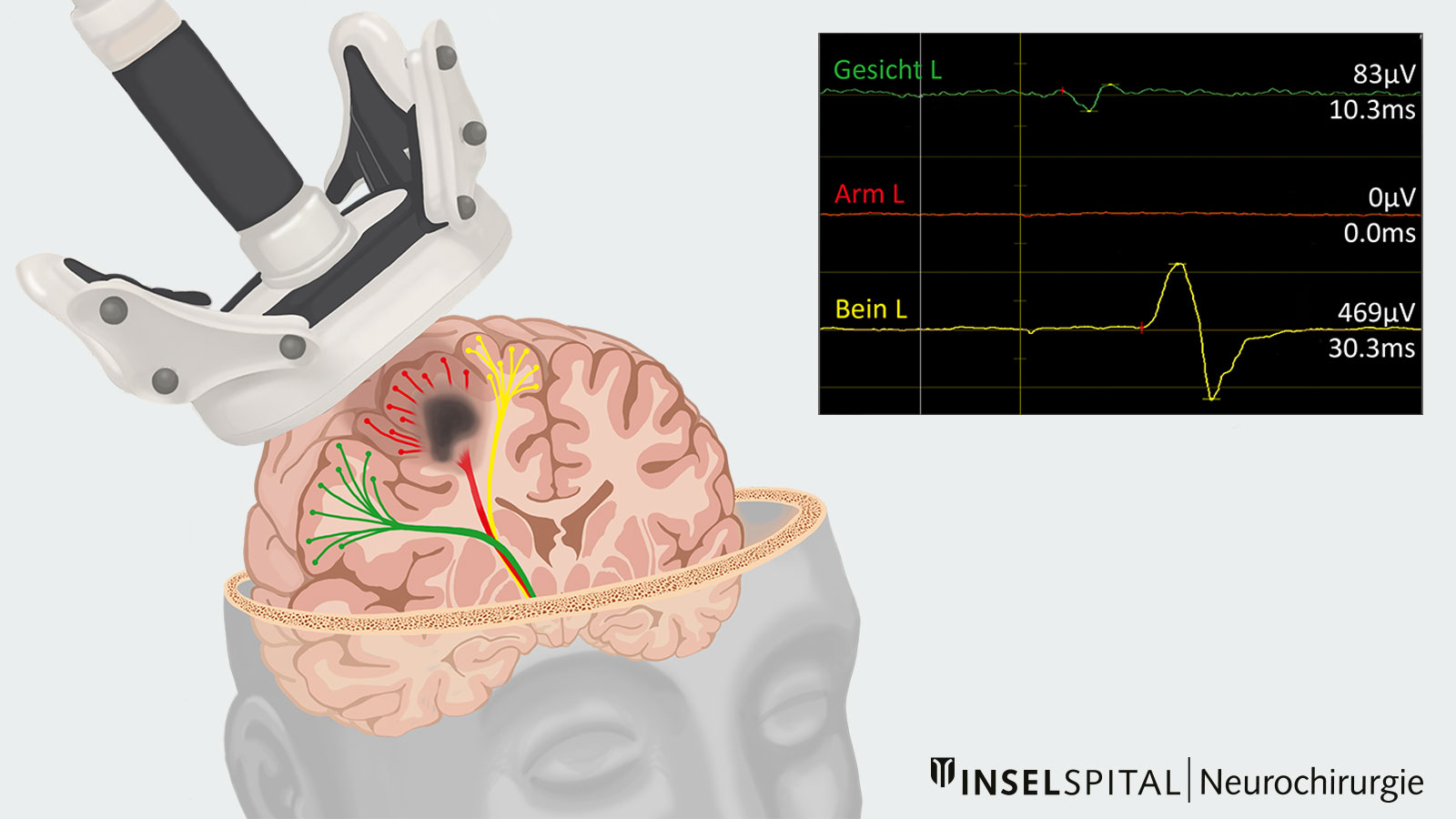
TMS is a non-invasive procedure in which nerve cells in the brain are stimulated from outside. A magnetic coil is placed on the patient's scalp. The coil generates rapidly changing magnetic fields that trigger a short electrical impulse in the brain. This impulse activates the connection between the motor cortex—the area of the brain that controls movement—and the corresponding muscles. The signal is transmitted in the form of an action potential via the muscle cells, causing the muscle to contract.
How does navigated TMS function?
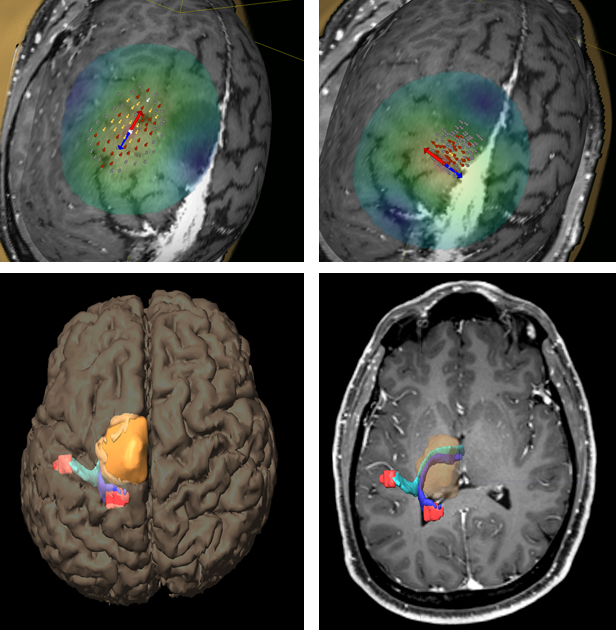
By registering the patient's head in three-dimensional space and integrating the data into neuronavigation, the exact location of the magnetic coil can be displayed on the patient's MRI image. This allows the area of the brain being stimulated to be shown precisely. For example, when the hand area of the motor cortex is stimulated, the fingers move. This not only allows the function of individual areas to be tested, but also reveals their spatial relationship to neighboring brain regions.
The motor-evoked potentials (MEPs) generated during stimulation can be measured, visualized, and analyzed. This information is particularly valuable for surgical planning, as it helps to spare functionally important areas.
By repeatedly stimulating different areas of the scalp and recording muscle responses, neurologists and neurosurgeons can accurately identify which areas of the brain are responsible for specific movements or functions.
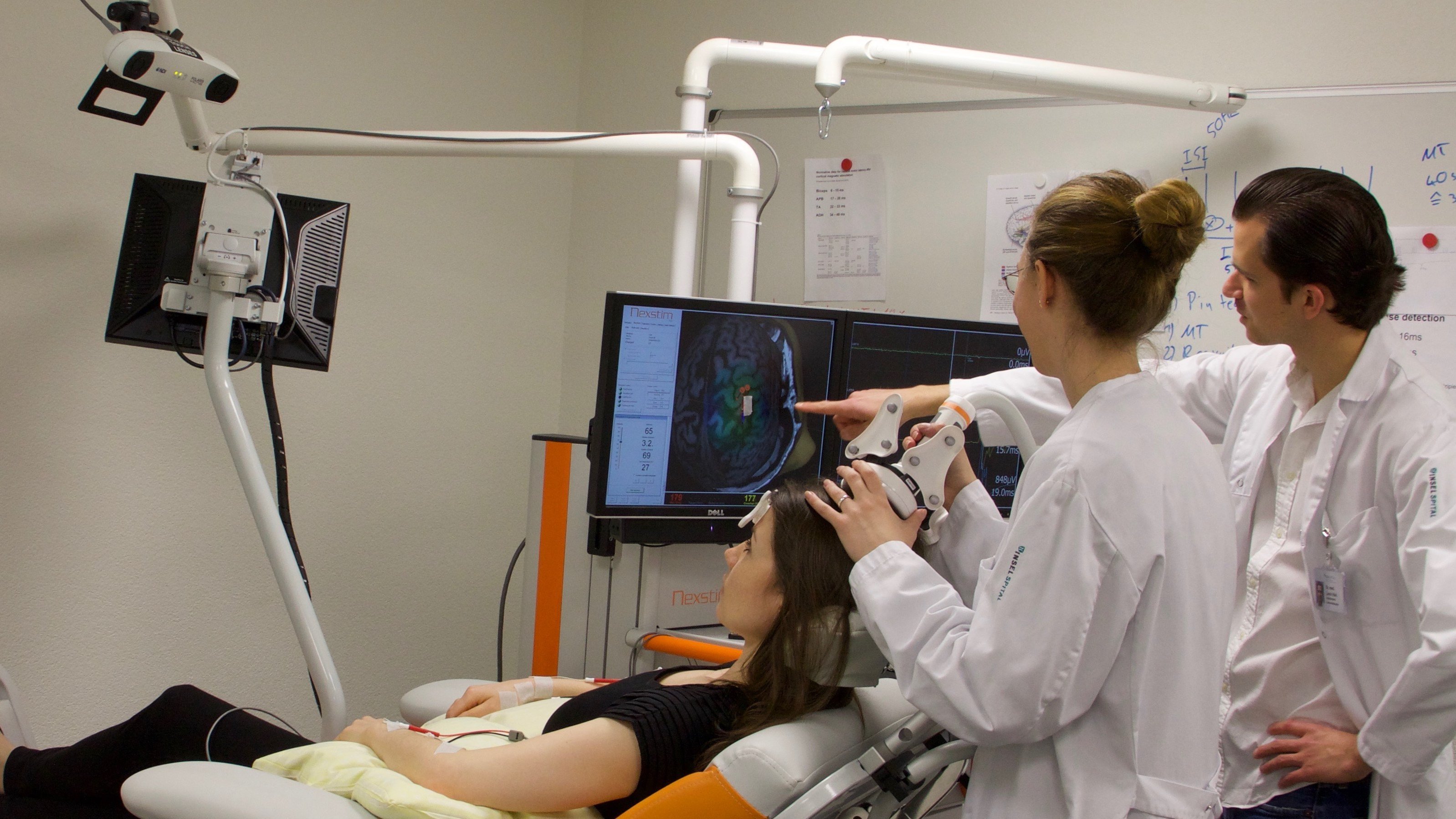
How is navigated TMS performed?
First, you are seated comfortably in a specialized chair. Your most recent brain MRI scan is loaded into the device. Three reference points are identified on your head and tracked using an infrared camera. This allows the stimulation to be precisely targeted with millimeter accuracy.
Depending on which motor center is being examined, adhesive electrodes are attached to the corresponding muscles. Through electromyography (EMG), the electrical activity of these muscles can be recorded and displayed. Your main role during the procedure is to stay relaxed.
Next, the magnetic coil is used to locate the motor area controlling the targeted muscles. A detailed functional map is created, showing exactly which areas of the brain control specific muscle movements. This map helps the neurosurgeon plan a safe and precise tumor removal.
The magnetic coil is then used to locate the motor center of the muscles to be examined, and a precise functional map is created. This map assists the neurosurgeon in planning safe and gentle tumor removal *.
Better predictions after surgery
In rare cases, surgery in the immediate vicinity of the motor center can lead to a loss of strength. In such cases, the same examination method can be used to predict how quickly recovery will take place. If the measurements show good responses in the arms and legs, a rapid recovery is likely *.
Our experience at Inselspital
At Inselspital, we are actively involved in the further development of innovative methods such as navigated transcranial magnetic stimulation. As part of international research projects and studies, we are continuously investigating new techniques to improve the precision and safety of neurosurgical procedures. In this way, we are helping to optimize surgical planning.
-
Krieg SM, Lioumis P, Makela JP, et al. Protocol for motor and language mapping by navigated TMS in patients and healthy volunteers; workshop report. Acta neurochirurgica. 2017;159:1187-1195.
-
Seidel K, Häni L, Lutz K, Zbinden C, Redmann A, Consuegra A, Raabe A, Schucht P. Postoperative navigated transcranial magnetic stimulation to predict motor recovery after surgery of tumors in motor eloquent areas. Clin Neurophysiol. 2019 Jun;130(6):952-959.
