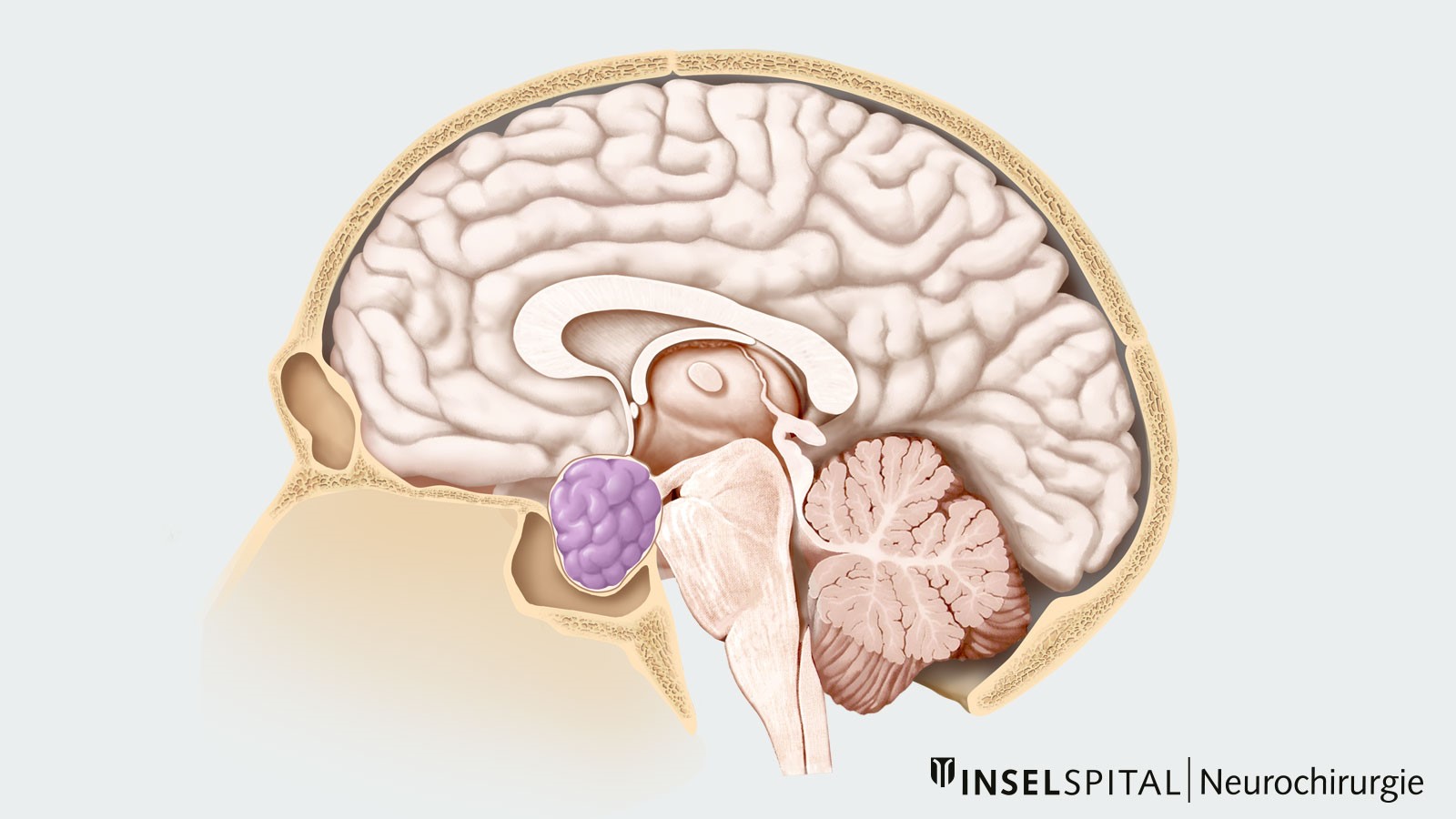
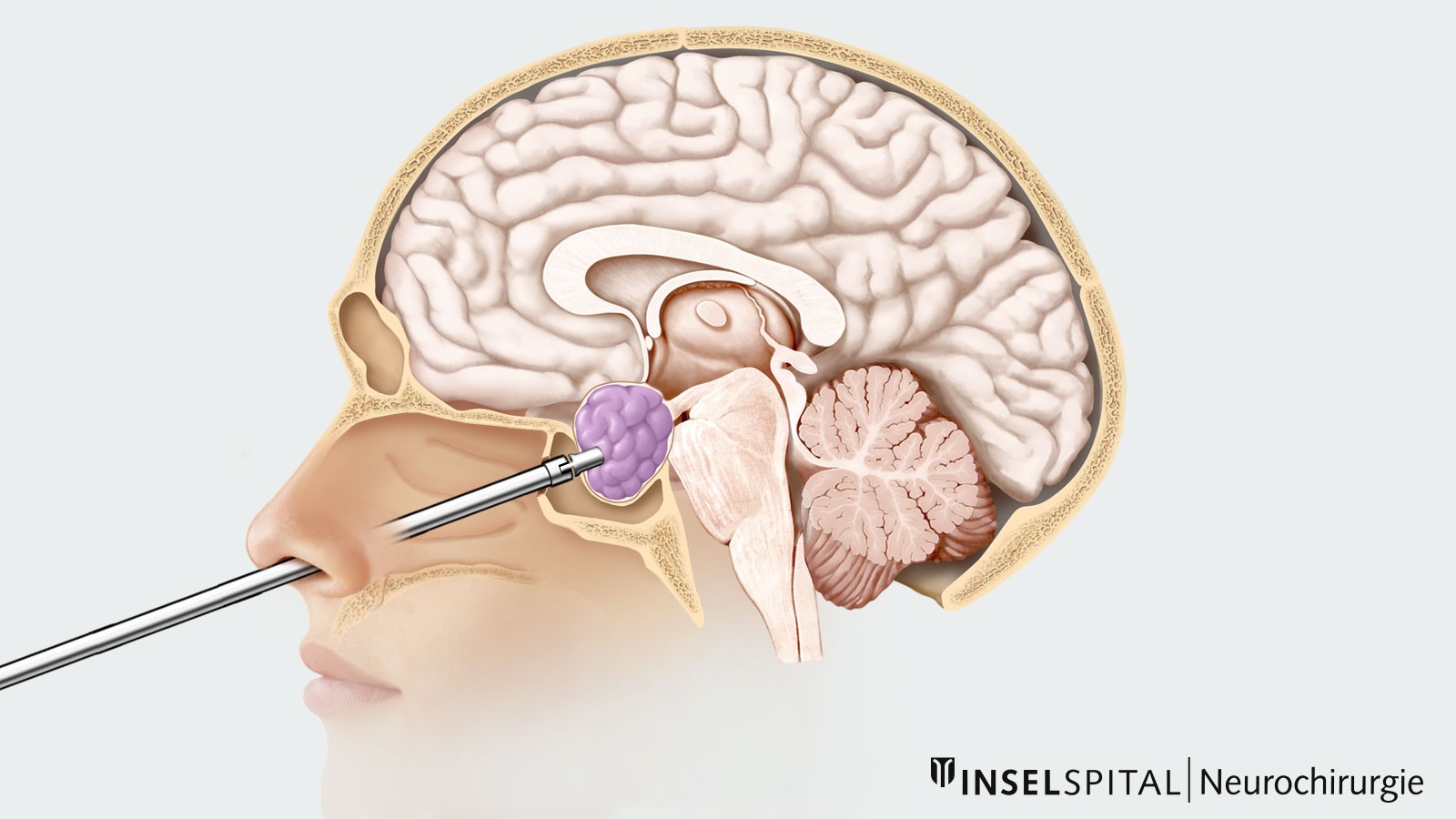
Pituitary adenomas are benign tumors of the pituitary gland, which is located in the anterior base of the skull. A distinction is made between hormone-active and hormone-inactive adenomas, as well as microadenomas (< than 1 cm) and macroadenomas (> than 1 cm). Pituitary adenomas cause hormonal disturbances. For prolactinomas, drug therapy is the first choice. For all other pituitary adenomas, surgical removal by minimally invasive surgery through the nose is indicated. This can be done either microsurgically or endoscopically.
How common is pituitary adenoma?
Pituitary adenomas account for about 10% of all brain tumors and occur most frequently between the ages of 30 and 40. Men and women are affected equally often.
What symptoms can a pituitary adenoma cause?
Smaller, hormone-inactive pituitary adenomas usually do not cause symptoms and are often discovered only incidentally when cerebral imaging is performed for other reasons. They are then referred to as incidental tumors.
A larger or hormonally active pituitary adenoma can cause quite different symptoms due to various underlying factors:
- hormonal disorders
- space-occupying effect on neighboring brain structures
- pituitary apoplexy, an acute hemorrhage in the pituitary gland
Hormonal disorders
Hormonal disorders are caused either by overproduction of hormones by the pituitary adenoma or by underproduction of hormones due to compression or infiltration of the pituitary gland.
| 65% | of adenomas actively secrete hormones: |
| 48% | prolactin |
| 10% | growth hormones |
| 6% | adrenocorticotropic hormone (ACTH) |
| 1% | thyrotropin (TSH), luteinizing hormone (LH), follicle stimulation hormone (FSH) |
Prolactin-producing tumors
Prolactin-producing tumors, so-called prolactinomas, can lead to functional disorders of the ovaries and testes, which can be manifested by
- menstrual disorders
- abnormal milk flow (galactorrhea) in women
- loss of libido in both sexes.
Growth-hormone-producing tumors
When tumors secrete growth hormones, possible symptoms include
- giant growth in chidren
- acromegaly in adults (in acromegaly, facial and cranial bones, hands and feet grow disproportionately)
- changes in the internal organs (e.g. heart muscle disease)
ACTH-producing tumors
Cushing's disease is a condition caused by a pituitary adenoma that produces ACTH. The resulting elevated cortisol levels can manifest in symptoms such as
- acne
- fat deposits on the abdomen
- full moon face
- bull neck
- stretch marks of the skin
- hypertension
- increased risk of thrombosis and embolism
TSH- and LH-/FSH-producing tumors
TSH- and LH-/FSH-producing tumors are less common.
Hormone-inactive tumors
In large hormone-inactive pituitary adenomas, compression of the pituitary gland and pituitary stalk may cause the following symptoms:
- deficiency of growth hormones and resulting growth or developmental disorders in children and deterioration of general condition and metabolic syndrome in adults
- deficiency of LH and FSH (hypogonadism) and resulting absence of menstruation in women and infertility and loss of libido in both sexes
- deficiency of TSH (hypothyroidism) and resulting cold intolerance, weight gain, fatigue, digestive disorders, skin changes, and memory impairment
- deficiency of ACTH (hypoadrenalism) and resulting low blood pressure on rising, increased fatigability and joint pain up to a life-threatening hormone deficiency (Addison's crisis)
Space-demanding effect on neighboring brain structures
A macroadenoma can press on and damage nearby brain structures and nerves. In addition to headaches, this can also cause other symptoms:
- a reduction in visual performance (visual loss) and/or visual field loss. Compression of the optic chiasm, the junction of the visual pathways, typically results in hemifacial blindness in both eyes with loss of one half of the visual field, called bitemporal hemianopsia
- double vision, facial pain, and drooping of the upper eyelids (ptosis) due to cranial nerve impairment with invasion of the cavernous sinus vein space
- headache, vomiting, impaired consciousness due to obstructive hydrocephalus. In obstructive hydrocephalus, the cerebrospinal fluid cannot drain properly due to a blockage, and the intracranial pressure increases.
Pituitary apoplexy
A pituitary apoplexy is an acute increase in size of a pituitary adenoma triggered by hemorrhage or dying tissue, called necrosis. The typical symptoms are:
- acute onset of severe headache
- acute loss of vision
- eye muscle paralysis
- possibly disturbances of consciousness
Pituitary apoplexy is a medical emergency.
How is a pituitary adenoma diagnosed?
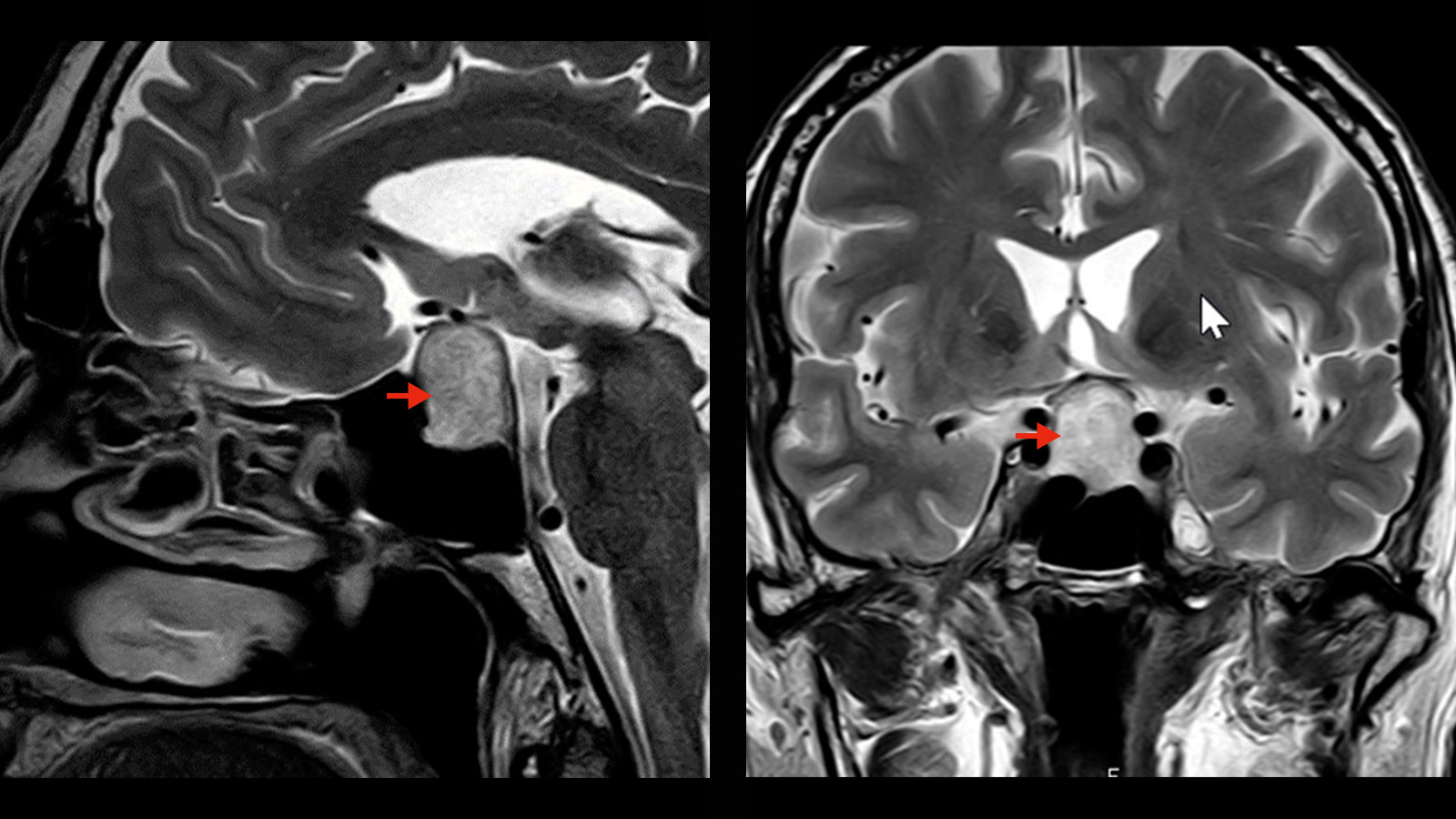
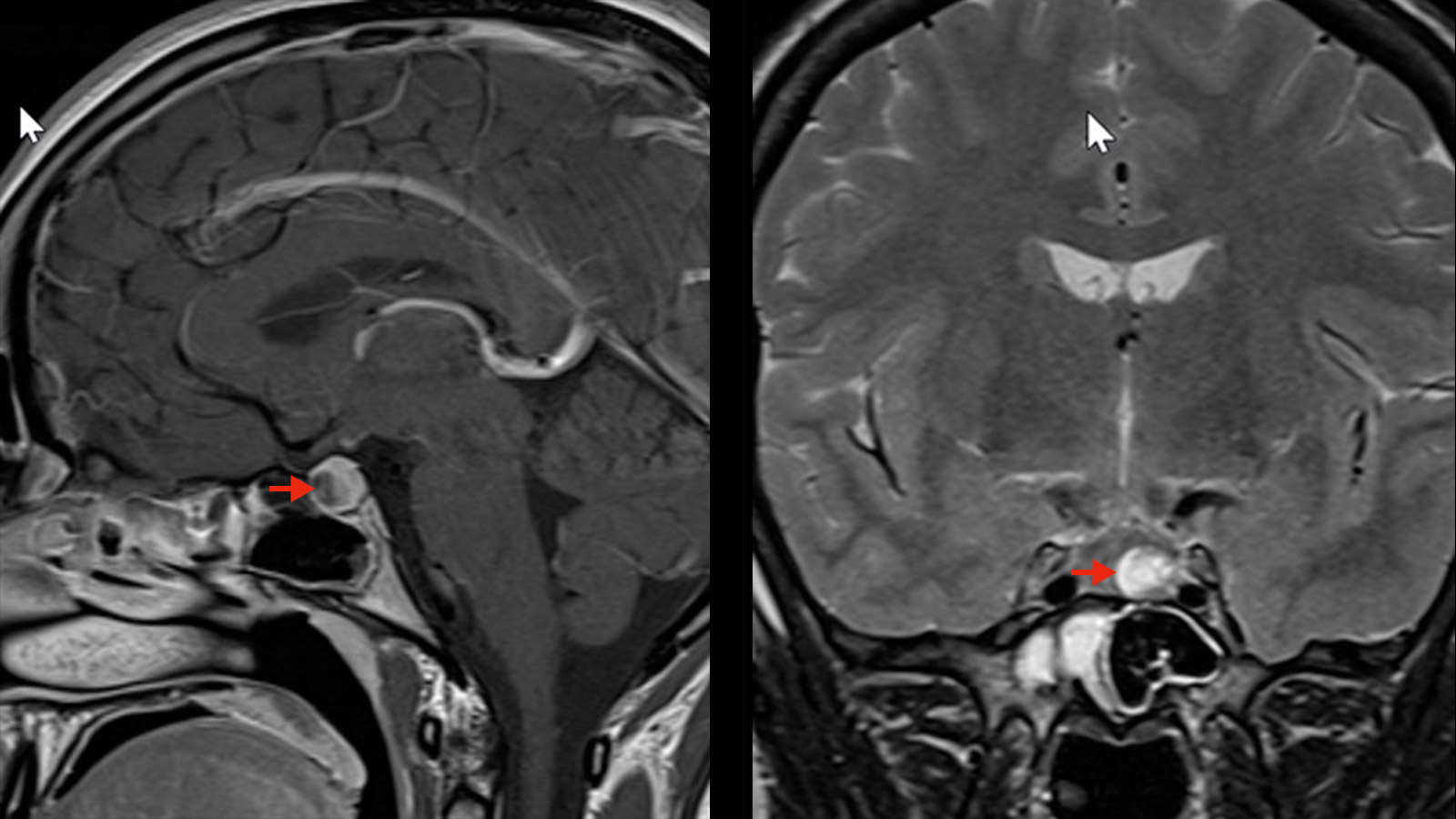
A TSH magnetic resonance imaging (MRI) with a contrast medium is the diagnostic procedure of first choice.
In all patients with pituitary adenomas, endocrinologic evaluation is indicated to diagnose and compensate for possible hormonal imbalances.
If the MRI image shows that the adenoma is in contact with the optic chiasm, the junction of the visual pathways, an additional ophthalmologic examination is necessary to clarify possible limitations of vision and visual field.
In the case of hypercortisolism (Cushing's disease), where an adenoma of the pituitary gland cannot be reliably determined by MRI examination, a special diagnostic procedure, sinus petrosal catheterization, must be used. This can be used to confirm the central cause of hypercortisolism and, if necessary, to determine a possible indication of laterality (right or left dominance of ACTH overproduction).
How is a pituitary adenoma treated?
In the case of hormone-inactive microadenomas that do not cause any symptoms, it is possible to wait and observe the adenoma in the course of regular follow-ups. In case of increase in size, surgical removal should be discussed.
For prolactinomas, drug therapy with dopamine agonists (e.g., cabergoline or bromocriptine) is the first-line therapy. In rare cases, prolactinomas can become so large and space-occupying that surgical removal is necessary to reduce the tumor mass.
For all other pituitary adenomas, surgical removal by minimally invasive surgery through the nose is indicated. This transnasal transsphenoidal surgery can be performed either microsurgically or endoscopically. Reoperation can also usually be performed for adenomas that regrow and form a recurrence.
For tumor remnants or recurrences that are difficult to access surgically, radiotherapeutic or radiosurgical treatment is a good alternative therapy.
Possible complications
Possible complications after resection of a pituitary adenoma are mainly disorders of electrolytesor hormonal balance. These disturbances may be temporary or permanent. In the postoperative phase, blood values and water balance are therefore monitored closely and hormones are substituted with medication if necessary.
If the pituitary adenoma has broken through the diaphragm sellae, in rare cases there may be leakage of cerebrospinal fluid from the nose after surgery, a condition known as rhinoliquorrhea. This occurs in about 3–5% of patients and necessitates a second operation to reseal the leak to prevent germs from entering the brain from the nose or sinuses.
Why you should seek treatment at Inselspital
Neurosurgery at Inselspital works closely with the departments of endocrinology, ophthalmology and radio-oncology. This is the only way to ensure comprehensive and high-quality care for each patient – before, during and after surgery. Each case is discussed by our interdisciplinary Pituitary Board, where an individual therapy plan is developed for each patient.
Our neurosurgery specialists have many years of surgical experience in the treatment of pituitary adenomas. Depending on the size of the adenoma, the microsurgical technique (endoscopically-assisted if necessary) or the full-endoscopic transnasal transsphenoidal technique are used. Both surgical procedures use the latest technological methods, such as 3D high-definition endoscopy and neuronavigation.
Further reading
- Benveniste, R., King, W., Walsh, J., Lee, J., Delman, B. und Post, K., 2005. Wiederholte transsphenoidale Operation zur Behandlung von rezidivierendem oder restlichem Hypophysenadenom. Journal of Neurosurgery, 102 (6), S. 1004-1012.
- Ciric I, Mikhael M., Stafford T., Lawson L., Garces R. Transsphenoidale Mikrochirurgie von Hypophysen-Makroadenomen mit Langzeit-Follow-up-Ergebnissen. Zeitschrift für Neurochirurgie. 1983; 59 (3): 395-401.
- Greenberg M. Handbuch der Neurochirurgie. 8. Aufl. Thieme 2016.
- Rotenberg, B., Tam, S., Ryu, W. und Duggal, N., 2010. Mikroskopische versus endoskopische Hypophysenchirurgie: Eine systematische Übersicht . The Laryngoscope, 120 (7), S. 1292-1297.
- Weerakkody, Y., 2020. Hypophysenadenom | Radiologie Referenzartikel | Radiopaedia.org. Verfügbar unter: https://radiopaedia.org/articles/pituitary-adenoma [Zugriff vom 8. Juni 2020].