Cluster headaches are among the most severely felt headaches of all. They bear their name because the headache attacks usually occur in clusters. In most cases, cluster headaches can be successfully treated with medication. If they occur chronically and medication does not work, there are functional neurosurgical treatment options such as occipital nerve stimulation (ONS) and deep brain stimulation (DBS).
What are chronic cluster headaches?
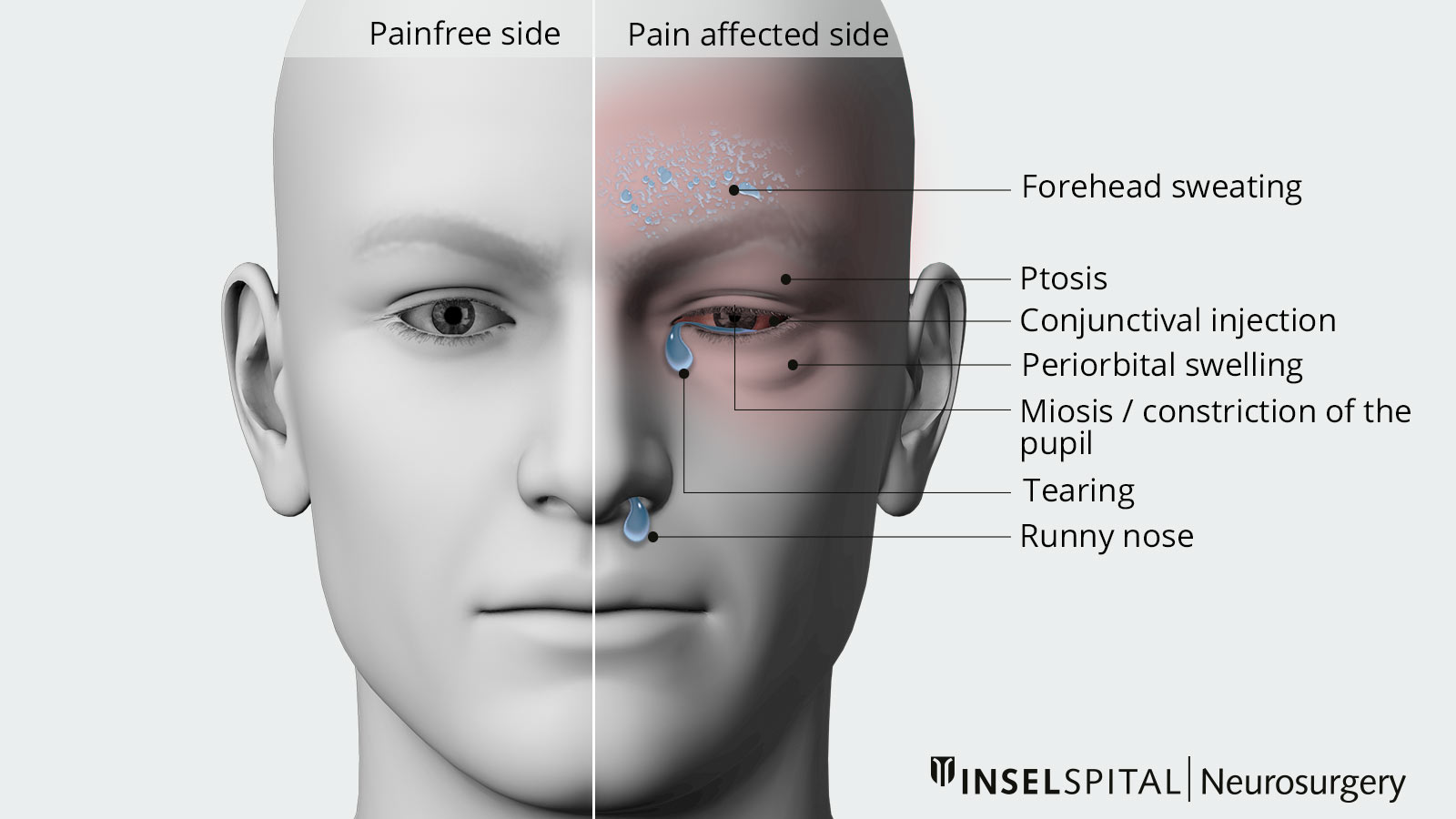
Cluster headaches are among the most severely experienced headaches. They manifest themselves as severe, one-sided, attack-like pain, usually in the area of the forehead, eyes and upper jaw. They often occur at night. The headache attacks occur in clusters, followed by symptom-free periods. The headaches themselves are accompanied by vegetative symptoms such as watery eyes, runny nose or swelling of the eye. If the pain occurs daily with no pain-free episodes, it is referred to as chronic cluster headaches *.
What are the treatment options?
Drug therapy
Drug therapy is the first choice for the treatment of cluster headaches. A distinction is made between drugs for acute attack treatment (triptans, oxygen inhalation) and drugs for relapse prophylaxis (verapamil, ergotamine, lithium, topiramate). Because of the potential side effects, medication should be administered and monitored by an experienced neurologist.
Neuromodulation
If cluster headaches occur chronically and respond inadequately to medication, a neuromodulatory procedure can be considered. Both occipital nerve stimulation (ONS) and deep brain stimulation
(DBS) are possible effective treatment alternatives for cluster headaches *.
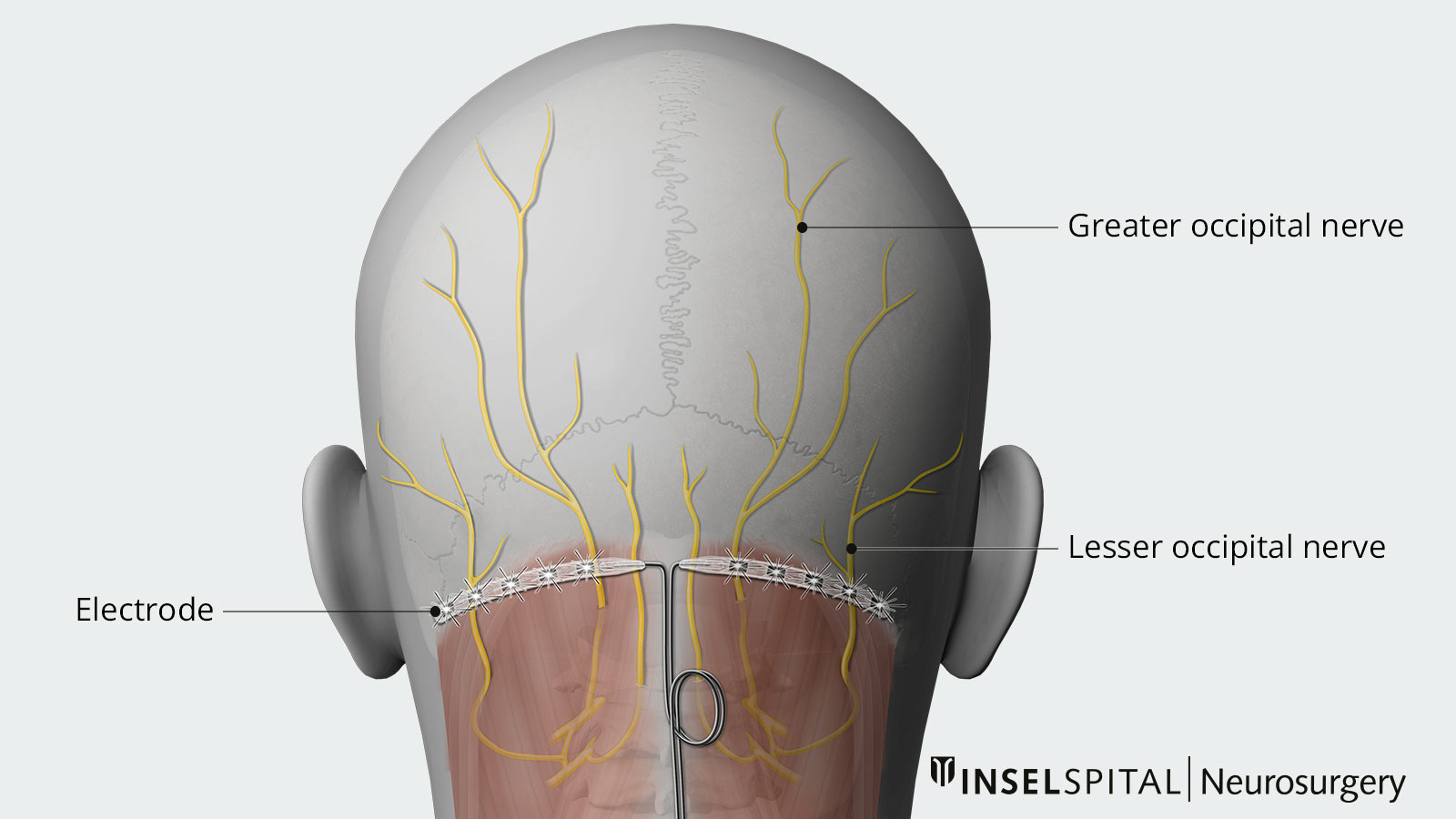
Occipital nerve stimulation
In ONS, electrodes are inserted under the skin in the suboccipital fatty tissue in the occipital region (see illustration). The aim is to stimulate the large and small occipital nerves. The electrodes are connected to a pacemaker, which is usually implanted below the collarbone.
Deep brain stimulation
Deep brain stimulation, or DBS for short, is the subject of intensive basic and clinical research. The number of diseases for which DBS is proving to be a potentially effective therapeutic measure is constantly growing. The continuous technical development of neurostimulators and stimulation electrodes as well as the improvement of imaging procedures in medicine also contribute to the immense development potential of this treatment method.
Status of studies
Occipital nerve stimulation (ONS)
A recently published large-scale prospective study from the Netherlands was able to prove the effectiveness of occipital nerve stimulation (ONS). The study examined 131 patients with chronic cluster headaches. A reduction in the frequency of headache attacks of around 45-55% was observed, depending on the level of stimulation, with significant inter-individual response rates. * These results correspond approximately to those of older studies. Several case series on ONS, each with 8–44 patients with chronic cluster headache, showed a response rate of approx. 64–77%. Patients with at least 50% headache reduction *, * were evaluated.
Deep brain stimulation (DBS)
Even smaller case series have been published on the treatment of chronic cluster headache with deep brain stimulation (DBS). The largest prospective case series to date of patients with chronic cluster headache from London showed results from 21 patients in whom all other treatment measures (including ONS in some cases) had failed *. Headache burden was reduced by an average of 68% in these patients, which is consistent with the results of smaller case series from other centers *, *, *.
A meta-analysis carried out by our research group confirms the high success rate of deep brain stimulation for chronic cluster headache. After evaluating the long-term results of a total of 40 patients who underwent surgery at four European centers, a response rate of 75% was found. This means that 75% of patients show at least a 50% reduction in headaches. The average number of headache attacks per week was reduced by an average of 77% in the long term. The results of this study were published in 2020 *.
The table shows the results of the meta-analysis in detail:
- The average frequency of headache attacks per week decreased from 36.8 to 12.6 after DBS over the total study observation period (average 44 months), a 77% reduction.
- Headache intensity improved from 8.2 to 4.4 at 12 months and even to 3.4 over the longer term (more than 50% reduction).
- The duration of headache attacks was also significantly reduced.
Overall, there was a 75% response rate, meaning 75% of all affected patients showed at least a 50% reduction in headache. The numbers in parentheses correspond to the control (so-called 95% confidence interval).
Results of DBS for chronic cluster headache (Nowacki et. al. 2020 *).
| Before surgery | 12 months after surgery | Long-term result | |
|---|---|---|---|
| Pain attacks (number/week) | 36.8 (31.2 –40.3) | 12.6 (6.5–18.6) | 12.6 (4.9–20.3) |
| Pain intensity (VAS pain scale with scores 0–10) | 8.2 (3.3–9.4) | 4.4 (3.3–5.5) | 3.4 (2.2–4.6) |
| Headache duration (min) | 57.69 (43.4– 0.0) | 25.7 (18.6–32.7) | 20.4 (12.7–28.1) |
| % Improvement | 77.0 (63.1–90.1) | 77.0 (68.0–87.0) | |
| Response rate (headache reduction > 50%) | 75% (60–86%) | 75% (60–86%) |
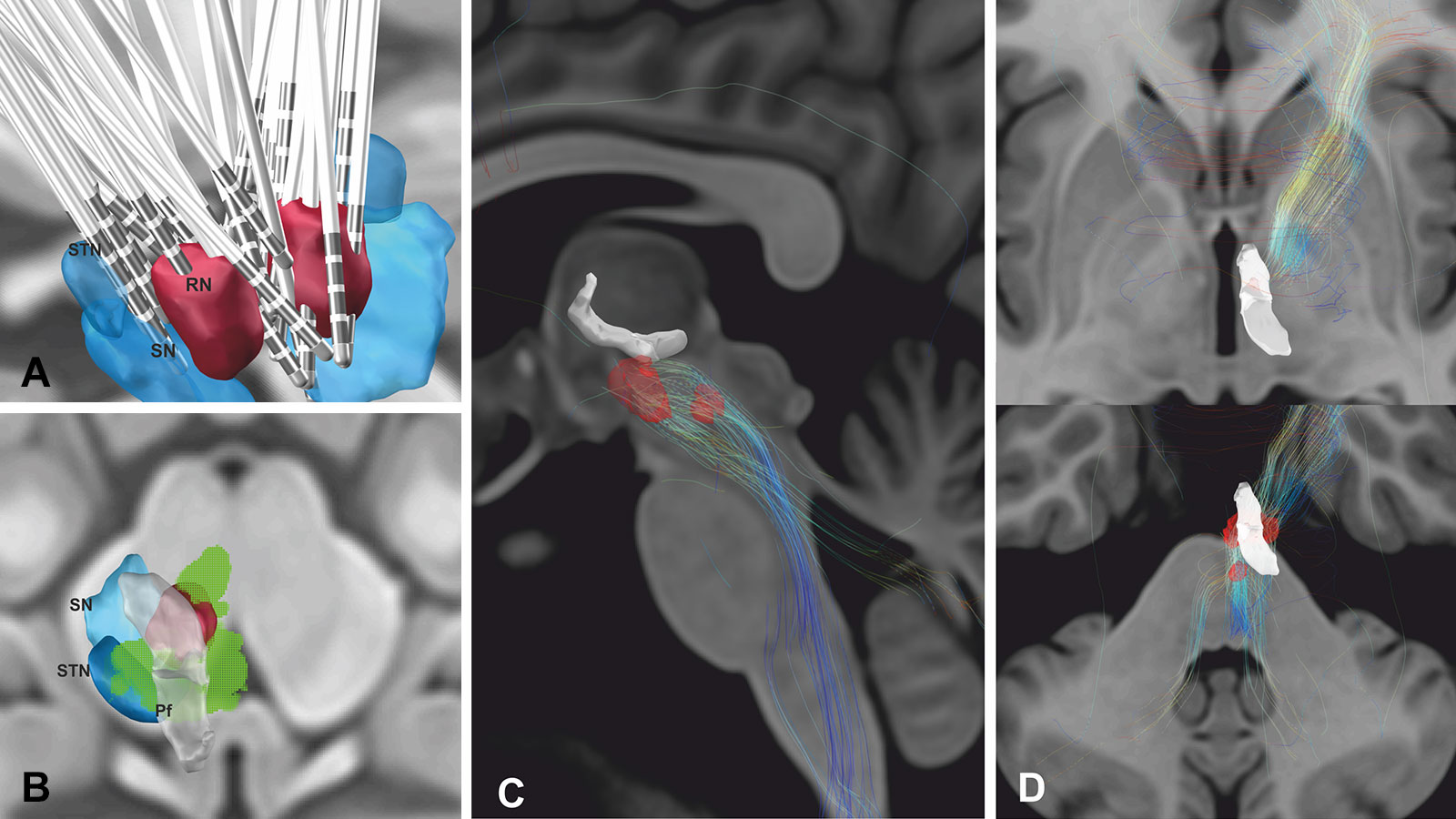
The imaging evaluation of the meta-analysis revealed interesting results. The thalamus and hypothalamus are known to be involved in pain processing. The trigeminal nerve, which also plays a role in the development of cluster headaches, emerges from the brain stem.
The electrode position and the effective electrical field of the stimulation in the patients analyzed activated the so-called ventral tegmental field in the midbrain area. It is known from anatomical studies that many nerve bundles run through this area, connecting the thalamus and hypothalamus with the brain stem. The modulation of precisely these nerve fibers therefore appears to account for the effect of deep brain stimulation on headache suppression.
-
May A. Cluster headache: pathogenesis, diagnosis, and management. Lancet. 2005;366:843-855.
-
May A, Leone M, Afra J et al. EFNS guidelines on the treatment of cluster headache and other trigeminal-autonomic cephalalgias. Eur J Neurol. 2006;13:1066-1077.
-
Fontaine D, Christophe Sol J, Raoul S et al. Treatment of refractory chronic cluster headache by chronic occipital nerve stimulation. Cephalalgia. 2011;31:1101-1105.
-
Leone M, Proietti Cecchini A, Messina G, Franzini A. Long-term occipital nerve stimulation for drug-resistant chronic cluster headache. Cephalalgia. 2017;37:756-763.
-
Akram H, Miller S, Lagrata S et al. Ventral tegmental area deep brain stimulation for refractory chronic cluster headache. Neurology. 2016;86:1676-1682.
-
Fontaine D, Lazorthes Y, Mertens P et al. Safety and efficacy of deep brain stimulation in refractory cluster headache: a randomized placebo-controlled double-blind trial followed by a 1-year open extension. J Headache Pain. 2010;11:23-31.
-
Nowacki A, Moir L, Owen SL, Fitzgerald JJ, Green AL, Aziz TZ. Deep brain stimulation of chronic cluster headaches: Posterior hypothalamus, ventral tegmentum and beyond. Cephalalgia. 2019;39:1111-1120.
-
Nowacki A, Schober M, Nader L, Saryyeva A, Nguyen TK, Green AL, Pollo C, Krauss JK, Fontaine D, Aziz TZ. Deep Brain Stimulation for Chronic Cluster Headache: Meta-Analysis of Individual Patient Data. Ann Neurol. 2020 Nov;88(5):956-969.
-
Wilbrink LA, de Coo IF, Doesborg PGG, Mulleners WM, Teernstra OPM, Bartels EC, Burger K, Wille F, van Dongen RTM, Kurt E, Spincemaille GH, Haan J, van Zwet EW, Huygen FJPM, Ferrari MD; ICON study group. Safety and efficacy of occipital nerve stimulation for attack prevention in medically intractable chronic cluster headache (ICON): a randomised, double-blind, multicentre, phase 3, electrical dose-controlled trial. Lancet Neurol. 2021 Jul;20(7):515-525.