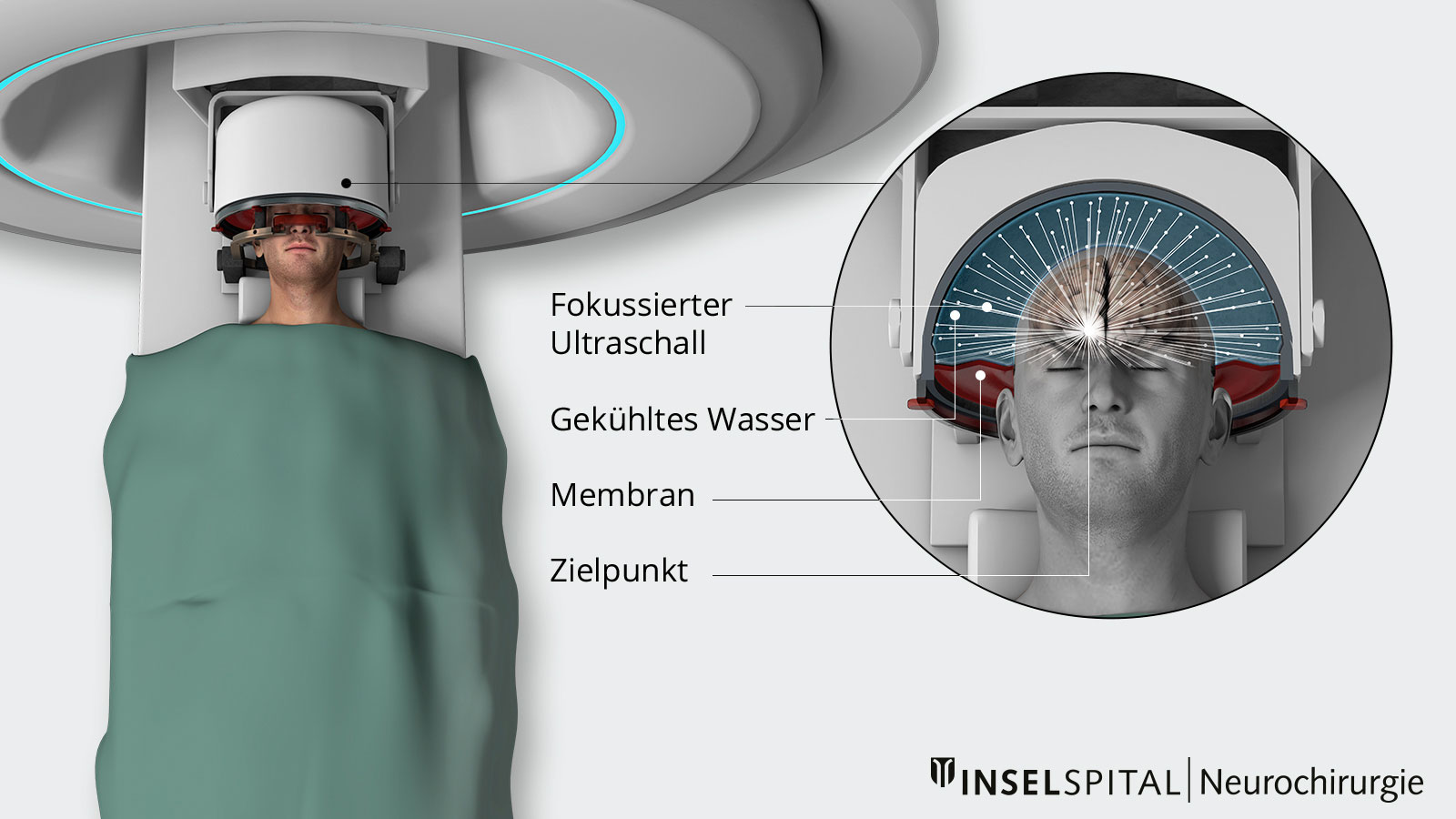
Magnetic resonance-guided focused ultrasound (MRgFUS or HIFU, short for high-intensity focused ultrasound) is a modern functional neurosurgical procedure for treating tremors, Parkinson's disease, and neuropathic pain that does not require any surgical incisions. Ultrasound waves are focused on a brain area measuring just a few millimeters, precisely bundled and converted into heat to selectively destroy nerve cells. Magnetic resonance imaging enables precise control and real-time monitoring. Patients benefit from rapid recovery.
How does MR-guided focused ultrasound work?
MR-guided focused ultrasound (MRgFUS) enables targeted modification of tissue deep within the brain—without any incisions in the skull. Bundled ultrasound waves are directed through the skull to a tiny point in the brain that is causing the symptoms of the disease. The ultrasound waves are harmless to the surrounding tissue because they only meet at a precisely defined target point in the brain, where they heat up the tissue. The procedure is extremely precise and capable of heating the small target area to around 55–60 °C with millimeter accuracy. At this temperature, the tissue is destroyed in a targeted manner. This process is called thermocoagulation or ablation.
Magnetic resonance imaging (MRI) enables precise control throughout the entire procedure: it shows the exact position of the ultrasound waves in real time and simultaneously measures the temperature in the target tissue. This ensures that only the desired area is treated, while the surrounding healthy brain tissue remains unaffected.
Which neurological disorders can be treated with MRgFUS?
MR-guided focused ultrasound is primarily used to treat movement disorders (essential tremor, tremor-dominant Parkinson's disease) or chronic pain conditions.
The most common indications include:
- Essential tremor: A common neurological disorder characterized by uncontrollable shaking of the hands or other parts of the body.
Tremor - Tremor-dominant Parkinson's disease: When the symptoms of the disease cannot be adequately controlled with medication and lead to a reduction in quality of life.
Parkinson's disease - Neuropathic pain: This is caused by damage to nerves or injuries to the spinal cord or brain, resulting in persistent, burning, or stabbing pain, often without any external injury. Neuropathic pain include
- Phantom pain after amputation
- Polyneuropathy (e.g., as part of diabetes)
- Plexus rupture
- Pain in paraplegia or tetraplegia
- Pain after a stroke
- Neuropathic trigeminal neuralgia
- Pain after herpes infection (e.g., shingles)
- Persistent pain after surgery for a herniated disc
Who is eligible for MRgFUS treatment?
Careful selection of suitable candidates is crucial for safety and treatment success. In cases of movement disorders, the indication is determined at the Interdisciplinary Center for Parkinson's Disease and Movement Disorders (ZfPB). In cases of neuropathic pain, the indication is also determined on an interdisciplinary basis following a pre-surgical assessment.
Important exclusion criteria are:
- intracranial vascular malformations
- blood thinning that cannot be paused for 2–3 days from an internal medicine perspective
- metal implants in the head area
- insufficient bone density of the skull bone or an excessively thick skull cap (upper part of the skull), as both can weaken the ultrasound waves
MRgFUS therapy: cooperation between Inselspital and Swiss Medical Network
MRgFUS therapy in the canton of Bern is offered exclusively by Swiss Medical Network and Inselspital, Bern University Hospital.
The actual treatment with MR-guided focused ultrasound (MRgFUS) is performed at the Medical Center Ostermundigen under the direction of PD Dr. Marc Gallay, an internationally recognized expert in this field. Inpatient care and follow-up treatment are provided in the neurosurgical/neurological ward of the Anna-Seiler-Haus at Inselspital, Bern University Hospital. Here, too, our patients receive interdisciplinary care from the team of doctors and nurses in the neurosurgery/neurology department at Inselspital and from PD Dr. med. Gallay.
This cooperation is an important addition to the range of treatments available for neurological movement disorders or pain conditions and guarantees our patients optimal therapy and care at the highest clinical and scientific level.
Preparation and assessment phase
The preparation and assessment phase prior to the procedure is similar to that for deep brain stimulation. A complete pre-surgical assessment is carried out.
The only additional examination required is a computed tomography (CT) scan of the skull. This is needed to assess the thickness of the skull bone. In rare cases, the skull is structured in such a way that treatment with focused ultrasound is not possible.
In addition, the head must be completely shaved before treatment.
During treatment
The actual treatment takes approximately two to four hours.
At the beginning, the head is fixed in a special stereotactic frame so that the ultrasound waves can be precisely aligned. This is done under local anesthesia.
An MRI is then performed to determine the exact target area inside the brain.
During the actual treatment, the patient remains awake and can talk to the doctors. Vital signs (heart rate, blood pressure, and oxygen levels in the blood) are monitored continuously throughout the treatment.
First, a test heating is performed, during which the temperature in the tissue is only slightly increased to approx. 41–43°C. If the result is satisfactory, the target area is further heated to 56–58°C, which finally deactivates a small area of about 2 mm in diameter.
The effect is immediate in cases of essential tremor, while symptom relief in neuropathic pain and Parkinson's disease develops gradually (progressively) over weeks to months.
Post-treatment care
After the procedure, our patients remain at the Inselspital for one to two nights for observation.
After discharge, follow-up checks are usually carried out after 1 month, 3 months, 1 year, and 3 years.
What are the risks?
Possible side effects of MRgFUS treatment are usually mild and often temporary. They also vary depending on the target area. These include:
General risks
- Mild headache or fatigue after treatment
- Swelling or tightness in the head due to the fixation (subsides within a few hours after removal of the frame)
- Nausea or dizziness during or shortly after treatment
- Post-treatment bleeding (very rare)
Specific risks associated with movement disorders
- Sensory disturbances (e.g., numbness or tingling in the hands or face) depending on the target site
- Mild unsteadiness or balance problems, which usually subside within a few days to weeks
- Temporary speech problems (very rare)
In very rare cases, permanent side effects may occur if surrounding tissue is affected.
MRgFUS for essential tremor
The average reduction in tremor is over 85% on the side operated on. *
There may be a temporary slight inhibition or delay in motor function on the operated side. This can be seen, for example, when walking, turning, and sometimes when speaking.
Specific risks associated with movement disorders
It is possible to treat both sides if this is necessary after a waiting period of at least one year.
MRgFUS in Parkinson's disease
Experience shows a reduction in tremors of over 80% in the first three months after the procedure *, *, *.
Rigor and bradykinesia, two main symptoms of Parkinson's disease, showed a reduction of 67% and 54% on the operated side in single-center studies involving unilateral treatment *, *, *. Data for bilateral treatment are also very promising, but further studies are needed to better demonstrate the risk-benefit ratio.
In addition, there were significant improvements in sleep quality and dyskinesia (involuntary, excessive movements) on the treated side of the body.
MRgFUS for neuropathic pain
Studies on the use of MRgFUS for neuropathic (neurogenic) pain have shown a significant reduction in pain, with an average relief of symptoms of around 42% in follow-up examinations (in some cases up to 55 months). Over 50% of those affected reported sustained pain relief of 50–100% in the last follow-up examination. *
In addition, studies show a reduced pain intensity and lower frequency of pain episodes. One year after treatment with focused ultrasound, the number of pain attacks was reduced by an average of 92%. *
Which therapy is suitable for whom?
Both MR-guided focused ultrasound and deep brain stimulation (DBS) are established procedures for treating essential tremor, Parkinson's tremor, and neuropathic pain.
For neuropathic pain, spinal cord stimulation and dorsal root ganglion stimulation are also available as treatment options.
The procedure used depends primarily on medical factors and the individual needs of the patient and is always discussed in detail by our interdisciplinary team of specialists.
-
Martínez-Fernández R, Natera-Villalba E, Rodríguez-Rojas R, Del Álamo M, Pineda-Pardo JA, Obeso I, Guida P, Jiménez-Castellanos T, Pérez-Bueno D, Duque A, Mañez-Miró JU, Gasca-Salas C, Matarazzo M, Alonso-Frech F, Obeso JA. Staged Bilateral MRI-Guided Focused Ultrasound Subthalamotomy for Parkinson Disease. JAMA Neurol. 2024 Jun 1;81(6):638-644. doi: 10.1001/jamaneurol.2024.1220.
-
Ahmed AK, Zhuo J, Gullapalli RP, Jiang L, Keaser ML, Greenspan JD, Chen C, Miller TR, Melhem ER, Sansur CA, Eisenberg HM, Gandhi D. Focused Ultrasound Central Lateral Thalamotomy for the Treatment of Refractory Neuropathic Pain: Phase I Trial. Neurosurgery. 2024 Apr 1;94(4):690-699. doi: 10.1227/neu.0000000000002752.
-
Martínez-Fernández R, Natera-Villalba E, Máñez Miró JU, Rodriguez-Rojas R, Marta Del Álamo M, Pineda-Pardo JÁ, Ammann C, Obeso I, Mata-Marín D, Hernández-Fernández F, Gasca-Salas C, Matarazzo M, Alonso-Frech F, Obeso JA. Prospective Long-term Follow-up of Focused Ultrasound Unilateral Subthalamotomy for Parkinson Disease. Neurology. 2023 Mar 28;100(13):e1395-e1405. doi: 10.1212/WNL.0000000000206771.
-
Krishna V, Fishman PS, Eisenberg HM, Kaplitt M, Baltuch G, Chang JW, Chang WC, Martinez Fernandez R, Del Alamo M, Halpern CH, Ghanouni P, Eleopra R, Cosgrove R, Guridi J, Gwinn R, Khemani P, Lozano AM, McDannold N, Fasano A, Constantinescu M, Schlesinger I, Dalvi A, Elias WJ. Trial of Globus Pallidus Focused Ultrasound Ablation in Parkinson's Disease. N Engl J Med. 2023 Feb 23;388(8):683-693. doi: 10.1056/NEJMoa2202721.
-
Gallay MN, Magara AE, Moser D, Kowalski M, Kaeser M, Jeanmonod D. Magnetic resonance-guided focused ultrasound central lateral thalamotomy against chronic and therapy-resistant neuropathic pain: retrospective long-term follow-up analysis of 63 interventions. J Neurosurg. 2023 Feb 24;139(3):615-624. doi: 10.3171/2023.1.JNS222879.
-
Cosgrove GR, Lipsman N, Lozano AM, Chang JW, Halpern C, Ghanouni P, Eisenberg H, Fishman P, Taira T, Schwartz ML, McDannold N, Hayes M, Ro S, Shah B, Gwinn R, Santini VE, Hynynen K, Elias WJ. Magnetic resonance imaging-guided focused ultrasound thalamotomy for essential tremor: 5-year follow-up results. J Neurosurg. 2022 Aug 5;138(4):1028-1033. doi: 10.3171/2022.6.JNS212483.
-
Stieglitz LH, Oertel MF, Accolla EA, Bally J, Bauer R, Baumann CR, Benninger D, Bohlhalter S, Büchele F, Hägele-Link S, Kägi G, Krack P, Krüger MT, Mahendran S, Möller JC, Mylius V, Piroth T, Werner B, Kaelin-Lang A. Consensus Statement on High-Intensity Focused Ultrasound for Functional Neurosurgery in Switzerland. Front Neurol. 2021 Sep 22;12:722762. doi: 10.3389/fneur.2021.722762.
-
Gallay MN, Moser D, Magara AE, Haufler F, Jeanmonod D. Bilateral MR-Guided Focused Ultrasound Pallidothalamic Tractotomy for Parkinson's Disease With 1-Year Follow-Up. Front Neurol. 2021 Feb 9;12:601153. doi: 10.3389/fneur.2021.601153.
-
Martínez-Fernández R, Máñez-Miró JU, Rodríguez-Rojas R, Del Álamo M, Shah BB, Hernández-Fernández F, Pineda-Pardo JA, Monje MHG, Fernández-Rodríguez B, Sperling SA, Mata-Marín D, Guida P, Alonso-Frech F, Obeso I, Gasca-Salas C, Vela-Desojo L, Elias WJ, Obeso JA. Randomized Trial of Focused Ultrasound Subthalamotomy for Parkinson's Disease. N Engl J Med. 2020 Dec 24;383(26):2501-2513. doi: 10.1056/NEJMoa2016311.
-
Eisenberg HM, Krishna V, Elias WJ, Cosgrove GR, Gandhi D, Aldrich CE, Fishman PS. MR-guided focused ultrasound pallidotomy for Parkinson's disease: safety and feasibility. J Neurosurg. 2020 Nov 27;135(3):792-798. doi: 10.3171/2020.6.JNS192773.
-
Gallay MN, Moser D, Jeanmonod D. MR-Guided Focused Ultrasound Central Lateral Thalamotomy for Trigeminal Neuralgia. Single Center Experience. Front Neurol. 2020 Apr 17;11:271. doi: 10.3389/fneur.2020.00271.
-
Gallay MN, Moser D, Jeanmonod D. MR-guided focused ultrasound cerebellothalamic tractotomy for chronic therapy-resistant essential tremor: anatomical target reappraisal and clinical results. J Neurosurg. 2020 Feb 7;134(2):376-385. doi: 10.3171/2019.12.JNS192219.
-
Gallay MN, Moser D, Rossi F, Magara AE, Strasser M, Bühler R, Kowalski M, Pourtehrani P, Dragalina C, Federau C, Jeanmonod D. MRgFUS Pallidothalamic Tractotomy for Chronic Therapy-Resistant Parkinson's Disease in 51 Consecutive Patients: Single Center Experience. Front Surg. 2020 Jan 14;6:76. doi: 10.3389/fsurg.2019.00076.
-
Schreglmann SR, Krauss JK, Chang JW, Bhatia KP, Kägi G. Functional lesional neurosurgery for tremor: a systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. 2018 Jul;89(7):717-726. doi: 10.1136/jnnp-2017-316302.
-
Schreglmann SR, Krauss JK, Chang JW, Martin E, Werner B, Bauer R, Hägele-Link S, Bhatia KP, Kägi G. Functional lesional neurosurgery for tremor: back to the future? J Neurol Neurosurg Psychiatry. 2018 Jul;89(7):727-735. doi: 10.1136/jnnp-2017-316301.
-
Gallay MN, Moser D, Jeanmonod D. Safety and accuracy of incisionless transcranial MR-guided focused ultrasound functional neurosurgery: single-center experience with 253 targets in 180 treatments. J Neurosurg. 2018 May 25;130(4):1234-1243. doi: 10.3171/2017.12.JNS172054.
-
Schreglmann SR, Bauer R, Hägele-Link S, Bhatia KP, Natchev P, Wegener N, Lebeda A, Werner B, Martin E, Kägi G. Unilateral cerebellothalamic tract ablation in essential tremor by MRI-guided focused ultrasound. Neurology. 2017 Apr 4;88(14):1329-1333. doi: 10.1212/WNL.0000000000003795.
-
Elias WJ, Lipsman N, Ondo WG, Ghanouni P, Kim YG, Lee W, Schwartz M, Hynynen K, Lozano AM, Shah BB, Huss D, Dallapiazza RF, Gwinn R, Witt J, Ro S, Eisenberg HM, Fishman PS, Gandhi D, Halpern CH, Chuang R, Butts Pauly K, Tierney TS, Hayes MT, Cosgrove GR, Yamaguchi T, Abe K, Taira T, Chang JW. A Randomized Trial of Focused Ultrasound Thalamotomy for Essential Tremor. N Engl J Med. 2016 Aug 25;375(8):730-9. doi: 10.1056/NEJMoa1600159.
-
Jeanmonod D. The Central Lateral Thalamotomy for Neuropathic Pain. In: Lozano, A.M., Gildenberg, P.L., Tasker, R.R. (Eds) Textbook of Stereotactic and Functional Neurosurgery. Springer, Berlin, Heidelberg.; 2009:2081-2096. doi:10.1007/978-3-540-69960-6_123