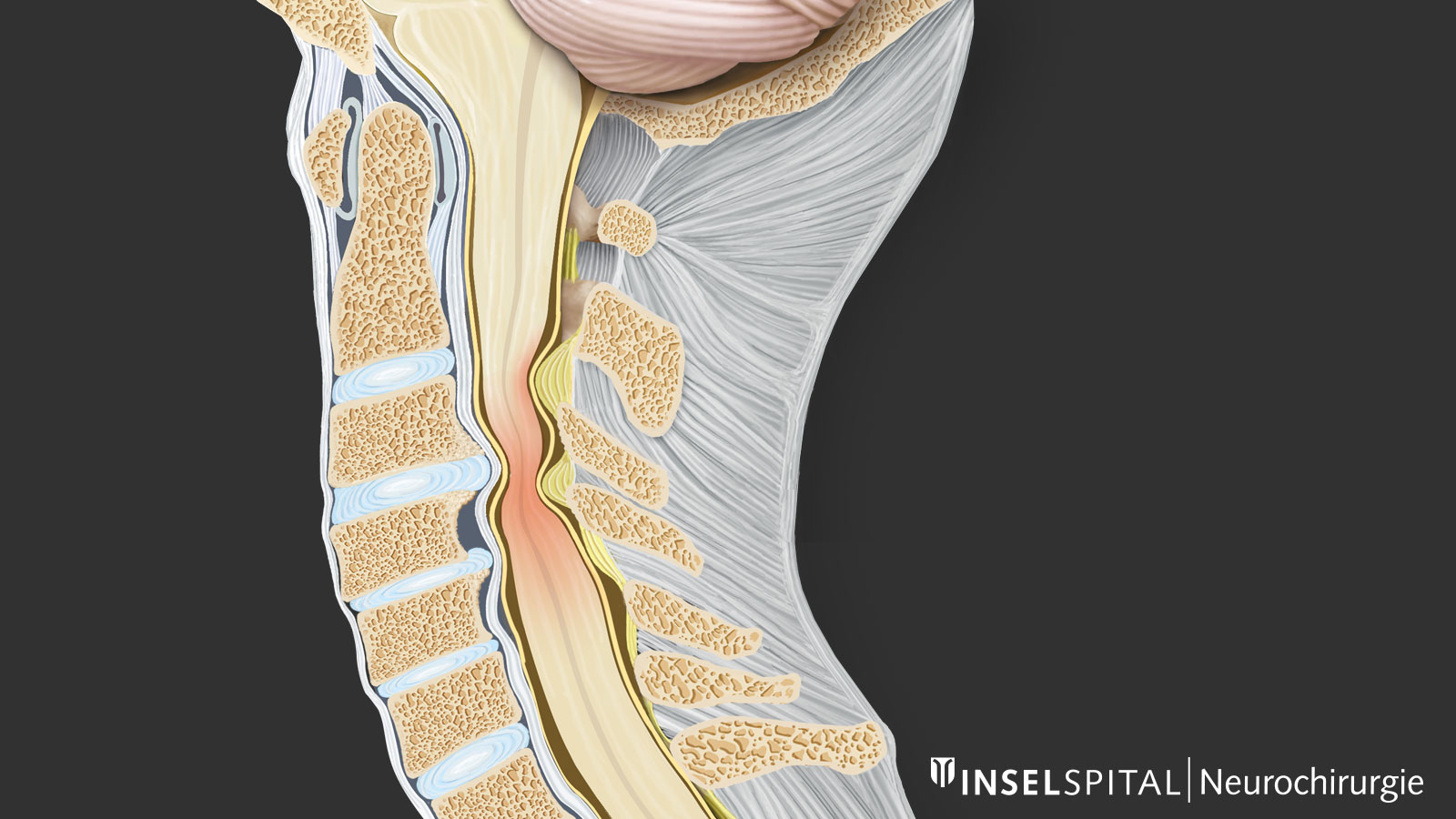
Cervical stenosis is a narrowing of the spinal canal in the neck area. It usually occurs due to the normal processes of aging. As with the lumbar spine, degenerative changes can lead to increased mobility between two vertebrae and excess formation of bone and connective tissue. Both are often linked. The body attempts to re-stabilize the spine by forming additional bone and ligamentous tissue and thickening joints. If the narrowing of the spinal canal results in damage to the spinal cord, this is called myelopathy.
What are the causes of a narrowing of the cervical spinal canal?
Narrowing of the spinal canal can be congenital. More common, however, is a secondary narrowing due to the degenerative changes of the spinal column. Cervical myelopathy therefore also has its age peak between the 50th and 70th year of life *.
Acquired or secondary narrowing of the spinal canal in the cervical region is referred to in medicine as cervical spinal stenosis. It can have two causes:
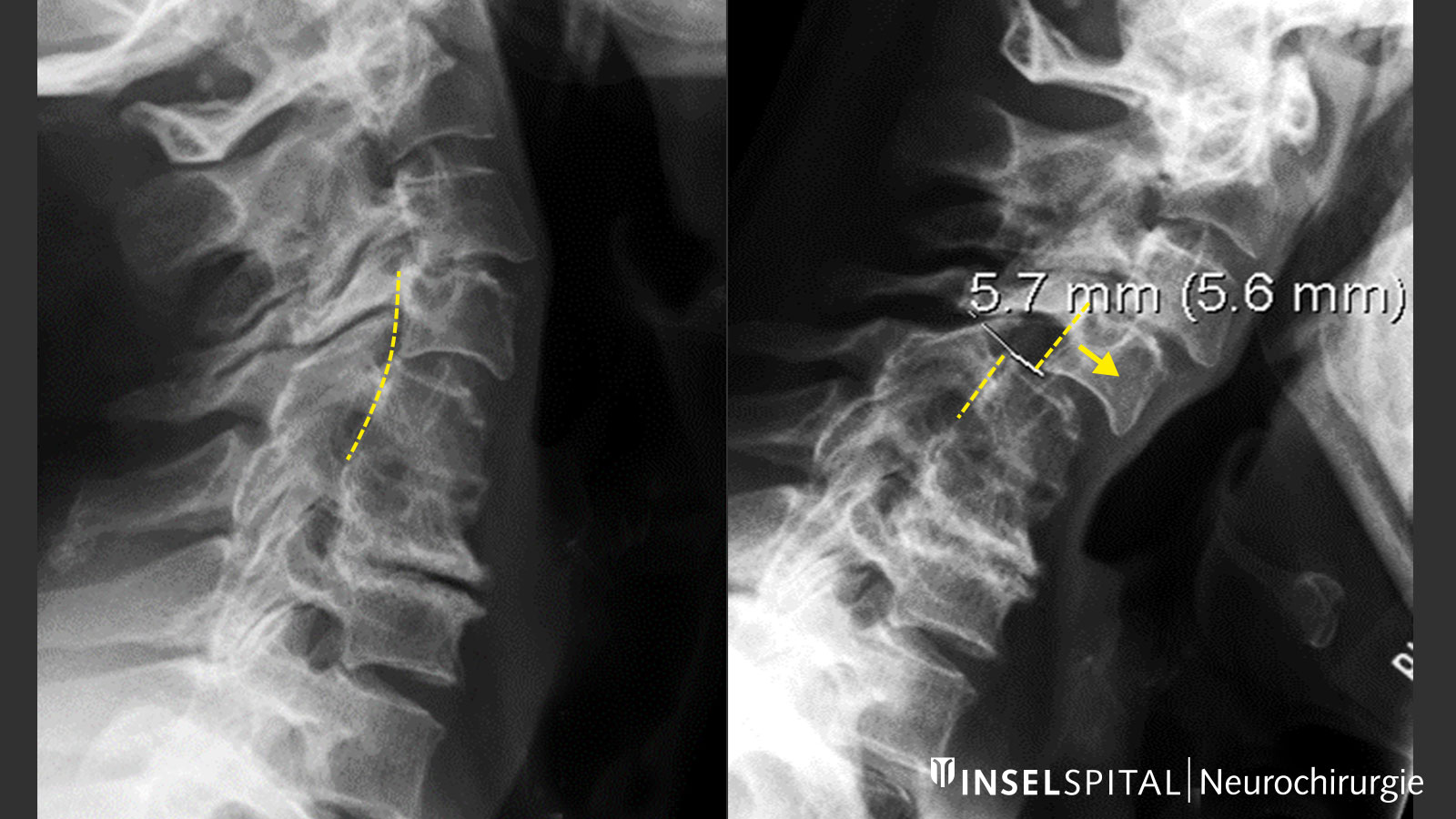
- Increased mobility and instability of the cervical vertebrae lead to a temporary, dynamic narrowing of the spinal canal during movements of the cervical spine.
- The spine forms new tissue due to aging and wear. Excess formation of bone or connective tissue increasingly narrows the spinal canal. This mechanism can be exacerbated by increased instability of the cervical vertebrae, as the body attempts to counteract instability through tissue formation and thickening.
What are the consequences of a stenosis of the spinal canal?
The spinal cord runs centrally in the spinal canal. Laterally, nerve roots emerge from the spinal column. A narrowing of the spinal canal can compress both the spinal cord and the nerve roots and lead to disorders. Nerve root compression is painful, but in contrast to spinal cord compression (cervical myelopathy), which is usually painless, it is less dangerous. However, both types of compression can permanently damage or even destroy tissue. This can occur directly via mechanical compression of the spinal cord or via vascular damage by stretching the spinal cord vessels or the feeding anterior spinal artery.
What are the symptoms of a cervical myelopathy?
The incidence of stenosis in the elderly population that does not cause symptoms is at least 25% *. The symptoms of spinal cord compression usually develop insidiously and non-specifically. In the case of pure spinal cord compressions, which are usually painless, years may pass from the first symptom until diagnosis.
Symptom progression
Initial signs include sensory disturbances in the hands or soles of the feet, clumsiness of the hands, and unsteadiness when walking in the dark. This is caused by a barely noticeable spastic or ataxic gait disorder and disturbances in depth sensitivity with reduction or loss of temperature and pain sensation as the first symptom.
Later, these symptoms intensify, and many patients complain of diffuse, patchy disturbances of sensation in the arms or legs.
Gait becomes increasingly stiff, wide-legged, jerky, and machine-like.
The disturbances of fine motor skills in the hands continue to increase, writing becomes angular and spidery, things can fall out of the hand. Buttoning clothes also becomes more difficult, and eating with cutlery is disturbed.
Vegetative disorders, such as urinary bladder emptying, may also occur.
Due to the different types of damage to the spinal cord, neurosurgeons and neurologists recognize typical syndromes *, *:
- Typical syndromes of damage to the spinal cord
- Posterior cord symptomatology: sensory disturbances, glove-like peripheral dysesthesias, disturbances of temperature and depth sensibility
- Motor syndrome: only weakness without sensory disturbances. Cause is damage to the pyramidal tract or anterior horn cells.
- Transverse syndrome: gait disturbances, spasticity and sensory disturbances
- Centromedullary syndrome: distal weakness of the upper extremities, the lower extremities are left out; possibly due to posterior horn lesions painful sensory disturbances of the hands. Damage to the central gray matter of the spinal cord
- Brown-Sequard syndrome: sign of unilateral spinal cord damage; ipsilateral hemiparesis due to involvement of the corticospinal tract and contralateral pain and temperature insensitivity below the lesion site
- Myeloradiculopathy as an expression of nerve and spinal cord dysfunction
The spontaneous course of the disease is very variable, with worsening more common than improvement. A worsening of the symptoms usually takes place over a longer period of time. However, it can also occur rapidly, and unfortunately the symptoms are then often no longer reversible. Neurological deterioration in episodes has been observed in 75% of patients *. Evidence suggests that approximately 5% of all patients with asymptomatic spinal cord compression become symptomatic each year *.
Acute courses are also known. These are usually patients with significant stenosis without symptoms who suffer acute damage to the spinal cord due to a minor injury. Under certain circumstances, this can lead to severe paralysis of the arms and legs *.
How is cervical stenosis diagnosed?
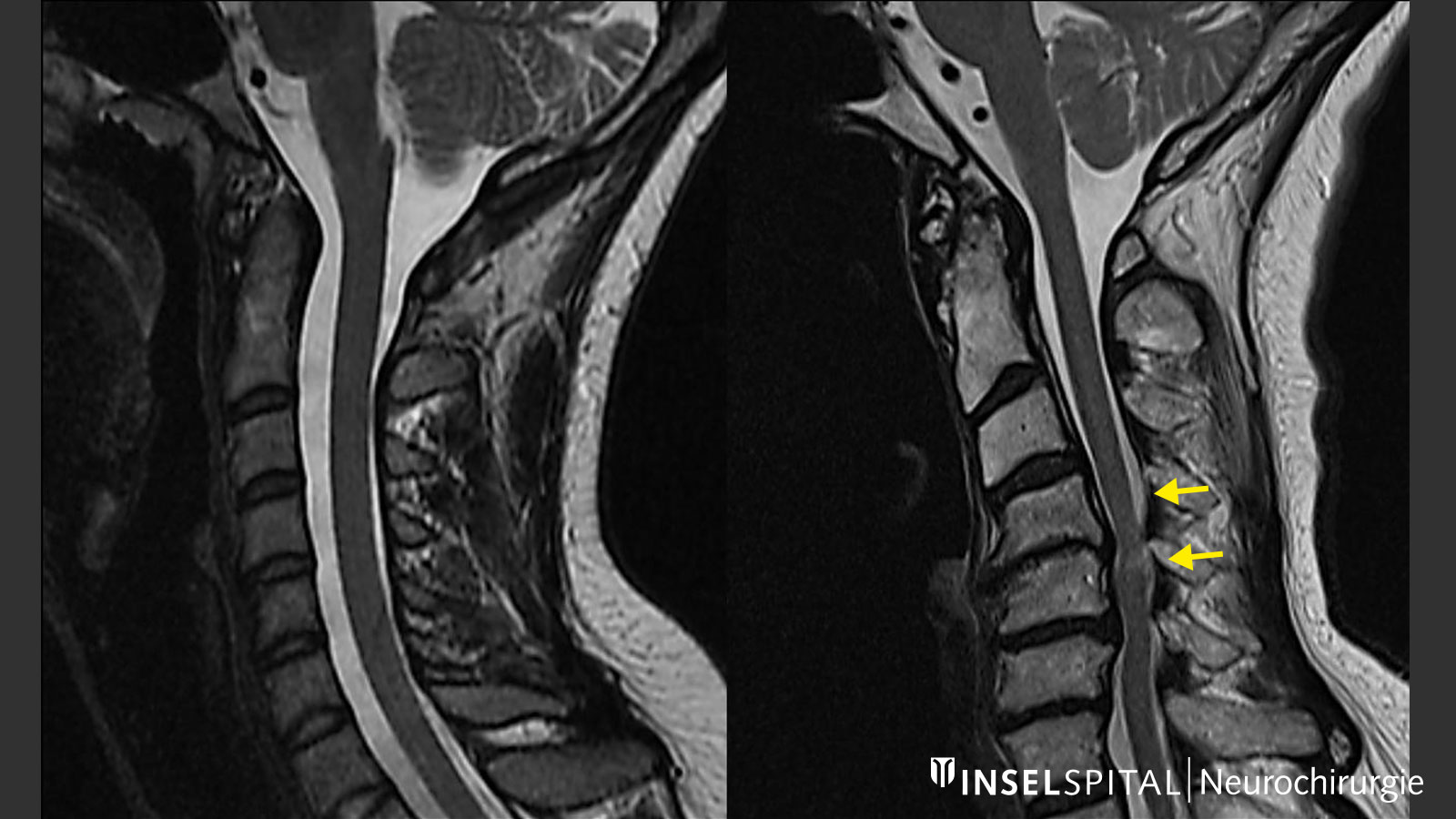
Spinal cord damage or cervical myelopathy is diagnosed when clinical symptoms are present or when the damage is detected by magnetic resonance imaging (MRI). The actual cause, namely the constriction or compression of the spinal cord, is usually also recognizable on the MRI images. In addition to a detailed neurological examination and MRI imaging, diagnostics also include X-rays of the cervical spine under movement to detect or rule out pathological mobility between the cervical vertebrae.
However: Since the symptoms caused by the constriction are initially gradual, varied and non-specific, the problem of the cervical spine is often only diagnosed at an advanced stage. It is not uncommon for patients to come to us in neurosurgery only after unsuccessful carpal tunnel surgery or after clarification of a suspected multiple sclerosis.
What are the treatment options?
In view of the increasing aging of the population and the expectation of an active lifestyle into old age, as well as the improved medical care and the low surgical risks, the question arises more and more frequently whether a stenosis should be operated on. Here, it should be taken into account that at least 25% of spinal stenoses in the elderly do not produce any symptoms. Therefore, clear criteria for an indication for surgery as well as a reasonable stepwise therapy are necessary.
The following rules apply:
- Pure wear and tear of the spine and compression of nerves can usually be treated with conservative therapy only.
- In the case of compressive myelopathy and clear symptoms, surgical decompression and immobilization should be performed. Space, and that is lacking in the compressed spinal cord, can only be gained by surgery.
What does conservative therapy look like?
In cases with wear and tear symptoms or mild nerve compression without myelopathy on MRI imaging, treatment with the following principles is often successful *:
- Short-term immobilization with a cervical spine brace and/or intermittent bed rest to relieve acute symptoms
- Drug therapy with non-steroidal anti-inflammatory drugs and muscle relaxants
- Local infiltration of a nerve with steroids and local anesthesia
- Physiotherapeutic traction treatment (longitudinal stretching of the cervical spine), loosening massages, acupuncture, low-level laser therapy
- Reconstruction and stabilization of the cervical spine through targeted strengthening of the
- neck muscles
- musculature of the upper quadrant
- shoulders
- Avoidance of activities that lead to heavy, permanent strain or to incorrect posture of the cervical spine
How is surgery performed for cervical stenosis and myelopathy?
In the combination of the different procedures, there are at least 6 different surgical methods, the use of which always depends on the individual findings of the patient.
If the stenosis is more anterior, relief is usually also from the front:
- Targeted removal of the narrowing, decompression of the spinal canal, implantation of a placeholder (cage) with or without plating
- Removal of the entire vertebra and insertion of an implant with plating
In case of stenosis more from the back or long-stretch ossification in the front (OPLL), the operation is performed from the back:
- Removal of the vertebral arches (laminectomy), usuallly with screw fixation for stabilization from behind
- Lifting of the vertebral arches to create space (laminoplasty)
What are the risks of surgery?
Non-medical professionals always dramatize the risk of spinal cord injury. However, in reality it is very low (< 1%). Rare is also the injury of a nerve during surgery or the occurrence of postoperative bleeding into the spinal canal (< 1-2%). Due to the access in the neck area, dysphagia or hoarseness may occur after surgery, which are usually temporary in nature (5%). Wound complications are also rare. In addition, in rare cases, the plastic implants can become loose or sink into the vertebrae. In most cases, however, this does not require treatment. Nevertheless, it must be kept in mind that despite the high level of safety of modern cervical spine surgery, there is a small risk of serious complications. For this reason, the indication for surgery should be made very carefully.
What happens after the operation?
Since this type of surgery can be performed more gently and quickly today, our patients are mobilized the day after the operation. During this process, the head and neck are supported by a soft tie for 1–2 weeks. Swallowing may be temporarily somewhat painful, as with a cold.
What improvement can patients expect after surgery?
About 70–80% of all patients improve. This is most pronounced when the disease is recognized with mild symptoms and surgery is performed early. With more severe symptoms, the improvement is less pronounced. This is because the spinal cord is part of the central nervous system and cannot regenerate as well as peripheral nerves. This shows how important early diagnosis is for the further course of the disease.
Is a relapse possible?
At the operated and immobilized level, this will very rarely be the case. However, the fusion of two vertebral bodies can increase the stress on the neighboring vertebrae. These connection degenerations are known and occur annually in about 3% of operated patients *. However, it is not possible to say with certainty whether they are due to the fusion or whether they would have occurred spontaneously. Connective degeneration can, however, be the cause of renewed pathological degeneration with instability or excess tissue formation and lead to a narrowing of the spinal canal again.
Can a cervical spinal stenosis be prevented?
To prevent the spinal cord from being damaged, it needs sufficient space in the spinal canal. Unfortunately, there are no patent remedies against the wear and tear of the spine and reactive narrowing. The most important preventive measure have proven to be strong and healthy neck muscles and a relaxed head posture. Working for long periods of time with a bent neck or in forced postures, such as jamming the phone between the head and shoulder, should be avoided. You should also look as straight ahead as possible when working at a computer screen. Likewise, working overhead for long periods of time or frequently carrying heavy loads on the head can accelerate wear and tear on the spine.
-
Teresi LM, Lufkin RB, Reicher MA et al. Asymptomatic degenerative disk disease and spondylosis of the cervical spine: MR imaging. Radiology. 1987;164:83-88.
-
Chiles III BW, Leonard MA, Choudhri HF, Cooper PR. Cervical spondylotic myelopathy: patterns of neurological deficit and recovery after anterior cervical decompression. Neurosurgery. 1999;44:762-769.
-
Crandall PH, Batzdorf U. Cervical spondylotic myelopathy. Journal of neurosurgery. 1966
-
Meyer F, Börm W, Thomé C. Degenerative cervical spinal stenosis: current strategies in diagnosis and treatment. Deutsches Ärzteblatt International. 2008;105:366.
-
Edwards II CC, Riew KD, Anderson PA, Hilibrand AS, Vaccaro AF. Cervical myelopathy: current diagnostic and treatment strategies. The spine journal. 2003;3:68-81.
-
Bednarik J, Kadanka Z, Dusek L et al. Presymptomatic spondylotic cervical cord compression. Spine. 2004;29:2260-2269.
-
Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. JBJS. 1999;81:519-528.

