Chordomas are rare, malignant tumors that occur along the entire spine and at the base of the skull causing damage to the bone. Depending on the location, patients most commonly experience double vision (for skull tumor) or decreased sensation and strength (for spine tumor) in addition to pain. The suspected diagnosis is made by an imaging examination, although only fine tissue examination provides a definitive diagnosis. The common treatment is surgical removal followed by radiation therapy.
What is a chordoma?
Chordomas are rare, malignant tumors that grow slowly, but are very destructive. They are classified as bone tumors and arise from the remnants of an embryonic structure, the chorda dorsalis, which is involved in the formation of the disc nuclei and vertebral bodies. Chordomas can occur along the entire spine, from the skull to the coccyx. About 50% of chordomas arise at the lower end of the spine (sacrum, coccyx), 30% at the base of the skull, and 20% along the rest of the spine at the neck level, chest, or sacrum.
As a result of their proximity to surrounding brain structures and cranial nerves, complete removal is usually very difficult. Local recurrences of the tumor are very common, at up to 85%. Around 30–40% of patients have metastases, the majority in the late phase of the disease. Metastases usually occur in the lungs, liver, bones, subcutaneous tissue and lymph nodes.
Who is most likely to develop a chordoma?
The average age at diagnosis is 60 years, although patients with chordomas of the skull base tend to be a younger age and children may also be affected. Chordomas are very rare, with an incidence of 0.5 cases/1 million people. Chordomas account for a total of 3% of all tumors of the spine and 1% of all tumors of the skull.
What are the symptoms of a chordoma?
The symptomatology depends on the localization of the tumor.
In intracranial chordomas, the symptoms are:
- Paralysis of the eye muscles
- Double vision
- Headache
In spinal chordomas, the symptoms are due to local compression of the spine:
- Pain
- Radicular symptoms (including loss of strength and sensation)
- Loss of bladder or rectal functions
How is a chordoma diagnosed?
The suspected diagnosis is made by means of imaging to clarify symptoms or also as an incidental finding in the context of other diagnostics.
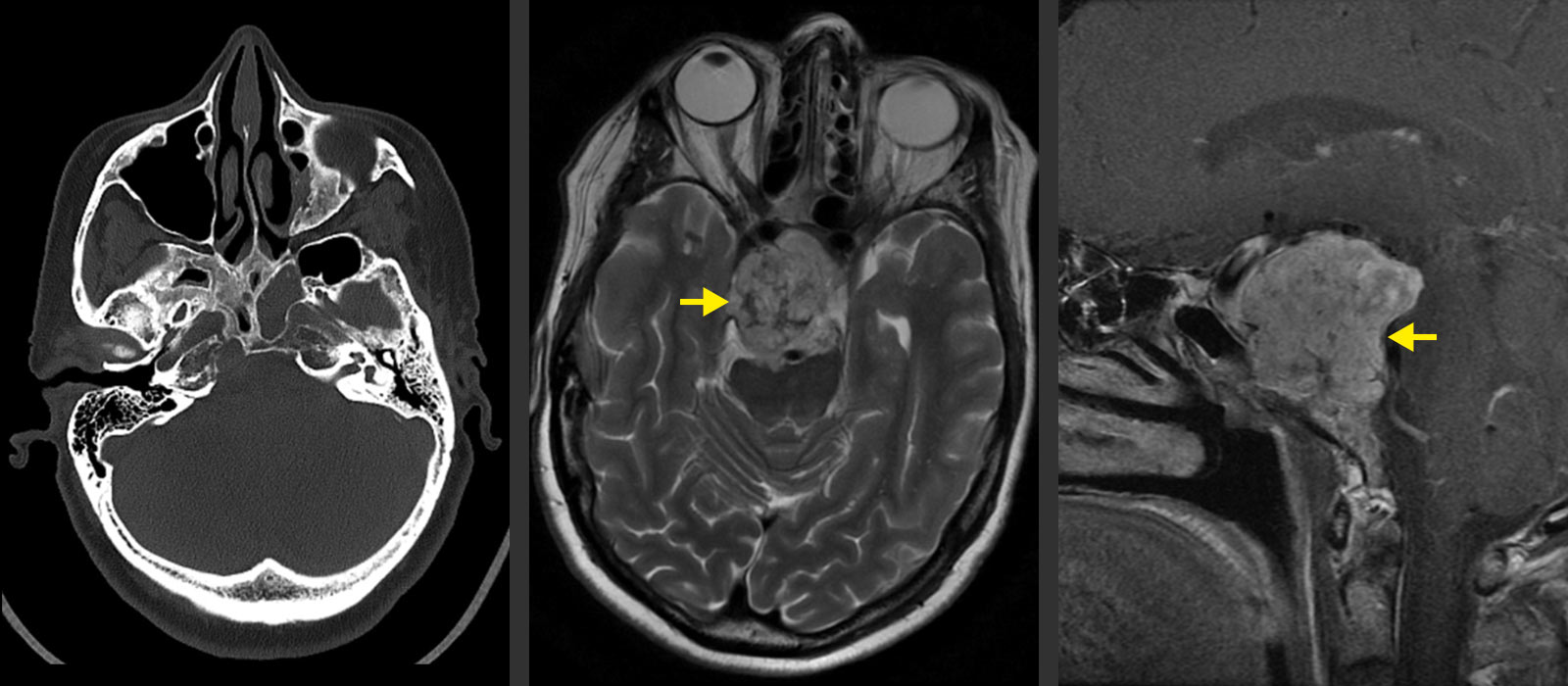
- Magnetic resonance imaging (MRI) is the leading method. In addition to the affected localization, an MRI of the entire spinal axis is always performed to exclude metastases located there.
- In addition, a computed tomography (CT) scan is performed to visualize the bone involvement in order to plan the surgical intervention.
- If intracranial vessel involvement is suspected, magnetic resonance angiography (MRA or MR angiography) or computed tomographic angiography (CTA or CT angiography) can complete the investigations.
However, a definitive diagnosis with assessment of benignity can only be made after tissue sampling and fine tissue microscopic examination by a neuropathologist.
What are the treatment options?
Surgery
The best therapy is a gentle and complete microsurgical or endoscopic removal of the tumor that is as complete as possible. However, this is not always possible due to infiltration of the surrounding area. Electrophysiological neuromonitoring is used during surgery to protect the surrounding nerve tissue. This procedure as well as the frequently used neuronavigation enable the neurosurgeon to work with maximum precision and safety under the operating microscope.
Radiotherapy
Neurosurgical tumor removal is almost always followed by radiotherapy (proton irradiation, radiotherapy or stereotactic radiosurgery). As an alternative to surgery followed by radiation, radiotherapy alone can also be performed.
Chemotherapy
According to the current results of studies, chemotherapy is only of minor importance in the treatment of chordomas.
Why you should seek treatment at Inselspital
At Inselspital, the best possible treatment strategy is determined individually for each patient. This is done in the certified neuro-oncological tumor center by an interdisciplinary team. This tumor board, which meets weekly, is composed of specialists from neurosurgery, neurology, neuro-oncology, nuclear medicine, radio-oncology and pathology. Here, each patient is discussed individually in order to determine the optimal treatment options for him or her.
For the operation itself, we use innovative technical procedures such as neuronavigation and intraoperative neuromonitoring. These new achievements are a guarantee for maximum precision during surgery and maximum safety for our patients.
