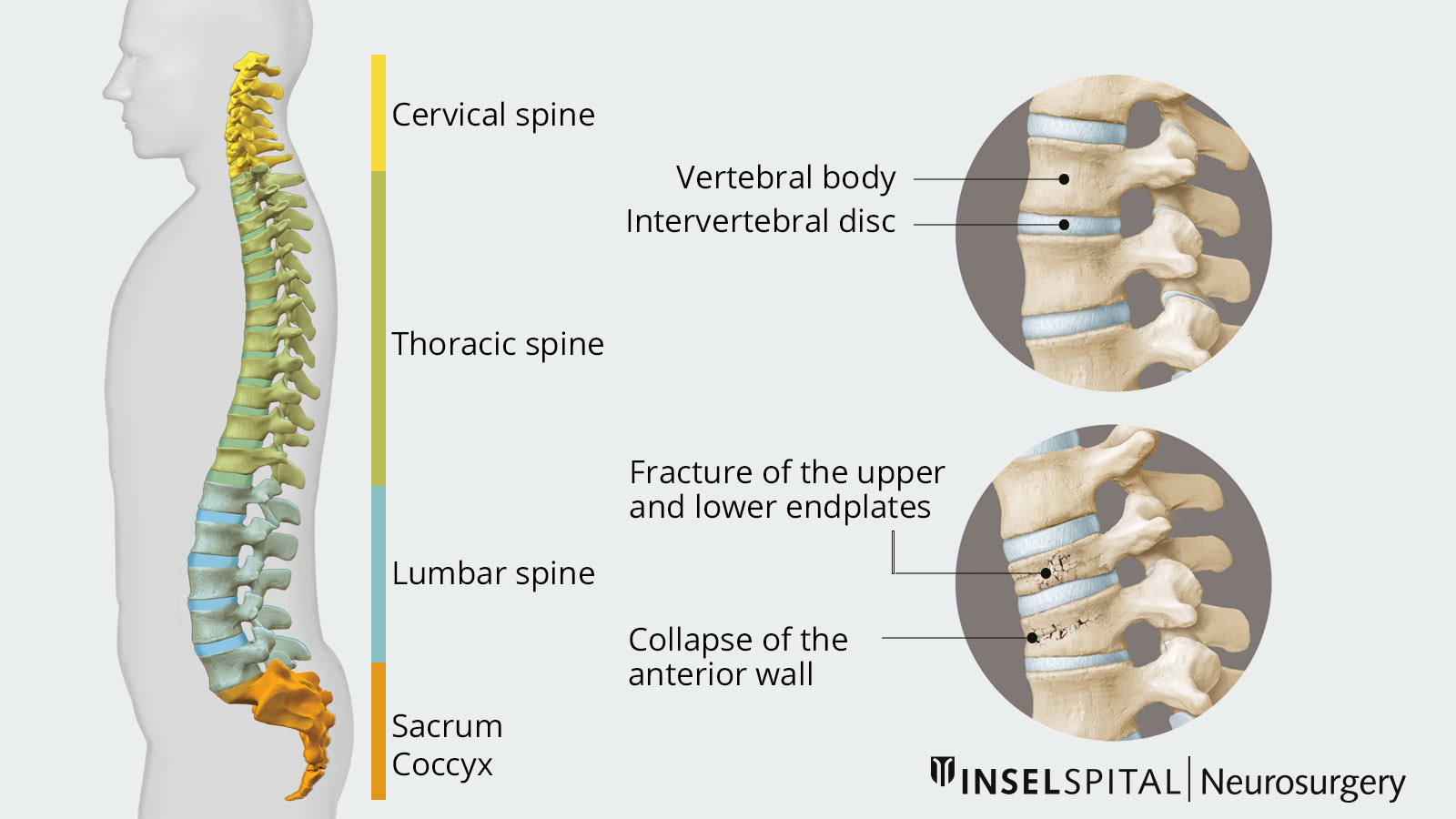
A vertebral fracture is a fracture of a vertebral body in the spine. The spine is composed of 24 free vertebrae, which are connected by intervertebral discs. In addition, some vertebrae are firmly fused together and form the sacrum and coccyx. A vertebral body fracture usually occurs due to an accident or fall or due to bone loss in old age, called osteoporosis.
What are the causes of a vertebral fracture?
An essential distinction is made between pathological fractures (due to osteoporosis or a tumor) and traumatic fractures (due to an accident or a fall). Osteoporosis is the most common cause of vertebral fractures, especially in old age and in connection with external forces. However, vertebral fractures can occur spontaneously in osteoporotic bones, even during everyday activities. Traumatic fractures are relatively rare and occur mainly in younger patients. In particular, falls from great heights or traffic accidents can cause injury to the spine.
With age, there is a general decrease in bone substance. If this is disproportionately large, it is called osteoporosis. In osteoporosis, the strength of the bone increasingly decreases. As a result, bone fractures occur easily. About 7% of men and 20% of women have osteoporosis after the age of 50. In addition, one-third of women and men over 50 suffer from osteopenia, a reduction in bone density that can be a precursor to osteoporosis.
The most common fractures in osteoporosis are vertebral fractures caused by minor traumas such as coughing or lifting heavy loads. The vertebrae of the thoracic or lumbar spine are most commonly affected. Here, the upper and lower endplates (fish vertebrae) or the anterior wall of the vertebral body (wedge vertebrae) collapse, resulting in various misalignments of the spine. These lead to incorrect loading and restricted movement. A typical feature is the increasingly stooped forward posture of the patient (kyphosis).
Fractures are divided into stable and unstable fractures. An unstable vertebral fracture also affects the posterior wall of the vertebral body and can compress the spinal cord or nerve roots with neurological deficits.
What are the symptoms of a vertebral fracture?
Often the only symptom of a vertebral fracture in old age is the sudden onset of back pain, radiating to the buttocks, flanks, or chest (thorax). These symptoms are often misinterpreted as "lumbago".
Only when there are several fractures andincreasing misalignment of the spinal column, does a visible hump formation or decrease in size occur. If the fracture also leads to a cpmpression of the spinal cord or nerves, radiating pain as well as neurological deficits may also occur.
How is a vertebral fracture diagnosed?
The first step in the assessment is to take a detailed history of the symptoms and, if applicable, the cause of the accident. In addition information on lifestyle habits and concomitant diseases as well as medication intake are important since some medications and many underlying diseases are associated with an increased risk of osteoporosis.
What stands out during the examination?
The physical examination focuses on the patient's basic posture, gait pattern, and general condition. In addition, physical examination reveals tenderness and sensitivity when palpating over the area of the fracture as well as an axial compression pain. If the vertebral fracture leads to a constriction of neural structures, there may be additional neurological deficits such as paralysis or sensory deficits.
What imaging techniques are used for diagnosis?
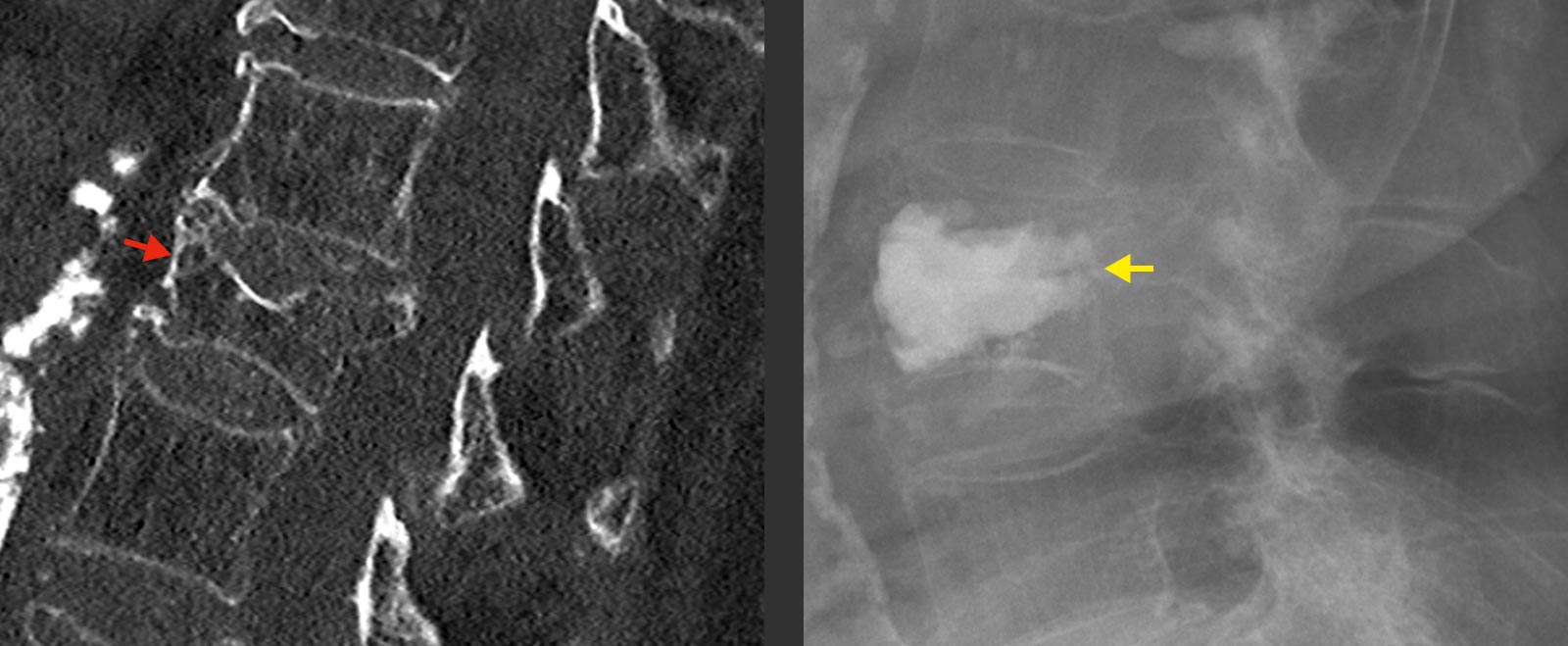
If a vertebral fracture is suspected in the history and clinical examination, it must be clarified further. For this purpose, an X-ray is taken in the standing position. In addition, computed tomography (CT) or magnetic resonance imaging (MRI) is very helpful to assess the condition and age of the fracture.
In all patients with suspected osteoporotic vertebral fractures, bone densitometry should also be performed. Dual X-ray absorptiometry (DXA) is the standard. Furthermore, daily calcium intake and other laboratory values should be checked. These are important prerequisites for the therapy and prevention of further fractures.
Conservative treatment
Most vertebral fractures in the elderly can be treated conservatively. Often the fractures are very painful and require good coverage with pain medication (analgesics). In addition, physical therapy and trunk orthoses can be used. Early mobilization is important to avoid concomitant complications. Vertebral fractures are often persistent and can cause pain for up to three months. This is mainly because complete immobilization of the spine, as with an arm in a cast, is impossible.
With all conservative treatments, regular X-ray checks of the spine should be performed while the fracture is healing so as not to miss further progression of the fracture and, in particular, pronounced malpositions of the affected spinal segment.
In addition, osteoporosis should be treated early and in a targeted manner. Appropriate osteoporosis medication can inhibit bone resorption and prevent further fractures. Furthermore, sufficient calcium intake should be ensured. This can usually be ensured by drug substitution. Physical activity also has a decisive influence on the development of osteoporosis. Exercise and sport maintain bone mass and reduce the risk of fractures.
Surgery
Surgical therapy of the vertebral fracture is advisable in some instances. In principle, there are two indications for surgical therapy:
- insufficient pain reduction by conservative therapy or
- unstable or progressive fractures associated with significant deformation of the spine
Surgical therapy must always be performed in addition to conservative therapy. For the surgical treatment of the vertebral fracture, cement augmentation is usually sufficient. This involves filling the fractured vertebral body with cement in order to stabilize it from the inside and prevent the fracture from progressing.
There are two methods for this, which have different areas of application:
- Vertebroplasty
In vertebroplasty, a hollow needle is inserted through the skin into the vertebral body under X-ray control. The vertebral body is then filled with bone cement via this needle. This results in a reduction of pain and prevents further collapse of the vertebral body. - Kyphoplasty
Kyphoplasty is a further development of vertebroplasty. Here, a balloon is first inserted into the vertebral body via the hollow needle and inflated in a controlled manner to straighten the fractured vertebral body. The resulting cavity is then filled with bone cement.
In the case of unstable fractures, cement augmentation alone is usually not sufficient. Here, additional stabilization of the vertebral body must often be performed with the aid of a screw and rod system. Access can often be minimally invasive and percutaneous (through the skin). Very rarely, surgical treatment of the fracture from the front or side is necessary.
If the vertebral fracture results in compression of the spinal cord or other neural structures, decompression is often required on an emergency basis to relieve pressure on the spinal cord and neurons in order to prevent neurologic deficits.
Why you should seek treatment at Inselspital
The Department of Neurosurgery at Inselspital maintains close interdisciplinary cooperation with the other conservative disciplines so that comprehensive diagnostics and targeted conservative therapy are possible. We have an experienced team of specialists for the treatment of vertebral fractures and also continue to monitor our patients closely.
If surgery is necessary, we draw on our microsurgical expertise and can usually help patients with minimally invasive procedures. Here we work closely with the Institute of Diagnostic and Interventional Neuroradiology. In our daily surgical routine at Inselspital, we use the latest intraoperative techniques such as intraoperative navigation und computed tomography to perform the gentlest possible effective surgery.
-
Blattert TR, Schnake KJ, Gonschorek O et al. Nonsurgical and Surgical Management of Osteoporotic Vertebral Body Fractures: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Global Spine J. 2018;8:50S-55S.
-
Schnake KJ, Blattert TR, Hahn P et al. Classification of Osteoporotic Thoracolumbar Spine Fractures: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Global Spine J. 2018;8:46S-49S.
-
Zwingenberg S et al. Klassifikation und Therapieempfehlung der osteoporotischen Wirbelkörperfraktur. Die Wirbelsäule 2019;3:217-235