Every surgical procedure requires imaging techniques. Which specific procedure is used depends on the type of surgery. For neurosurgical interventions, imaging must usually be supplemented by additional monitoring methods. In our clinic, intraoperative imaging is used as standard for all procedures.
Why is intraoperative imaging so important?
There are very different methods of intraoperative imaging, each with different objectives. What all these imaging procedures have in common, however, is that they are used while the patient is still asleep during an operation. The information obtained in this way can then be used immediately for further surgery.
The main advantage of intraoperative imaging is therefore that the surgeon can assess the surgical result still in the operating room and make any necessary corrections or adjustments while the operation is still in progress. Intraoperative imaging is therefore an important tool for the success of an operation:
- Brain tumors can be removed more comprehensively
- Surgical measures such as the elimination of vascular malformations or aneurysms can be checked directly
The intraoperative operation of imaging procedures requires a high level of expertise. In addition, the subsequent installation of intraoperative imaging requires structural changes in most clinics and therefore incurs high costs. The new construction of the high-precision operating theaters at the Inselspital has made it possible for our clinic to implement all of the imaging systems mentioned below.
Which intraoperative imaging procedures do we use?
The imaging procedures we use during an operation include
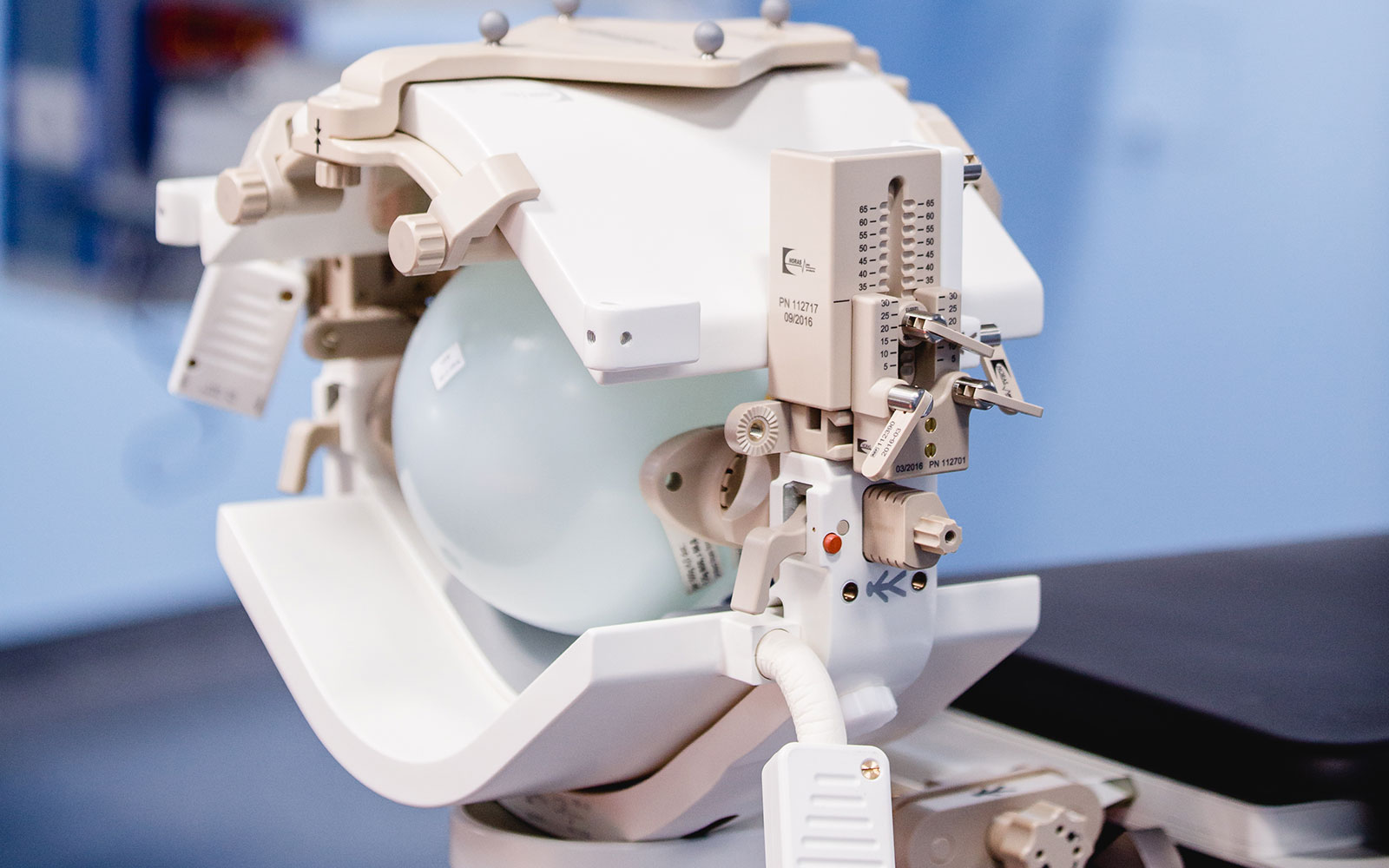
Intraoperative magnetic resonance imaging (iMRI)
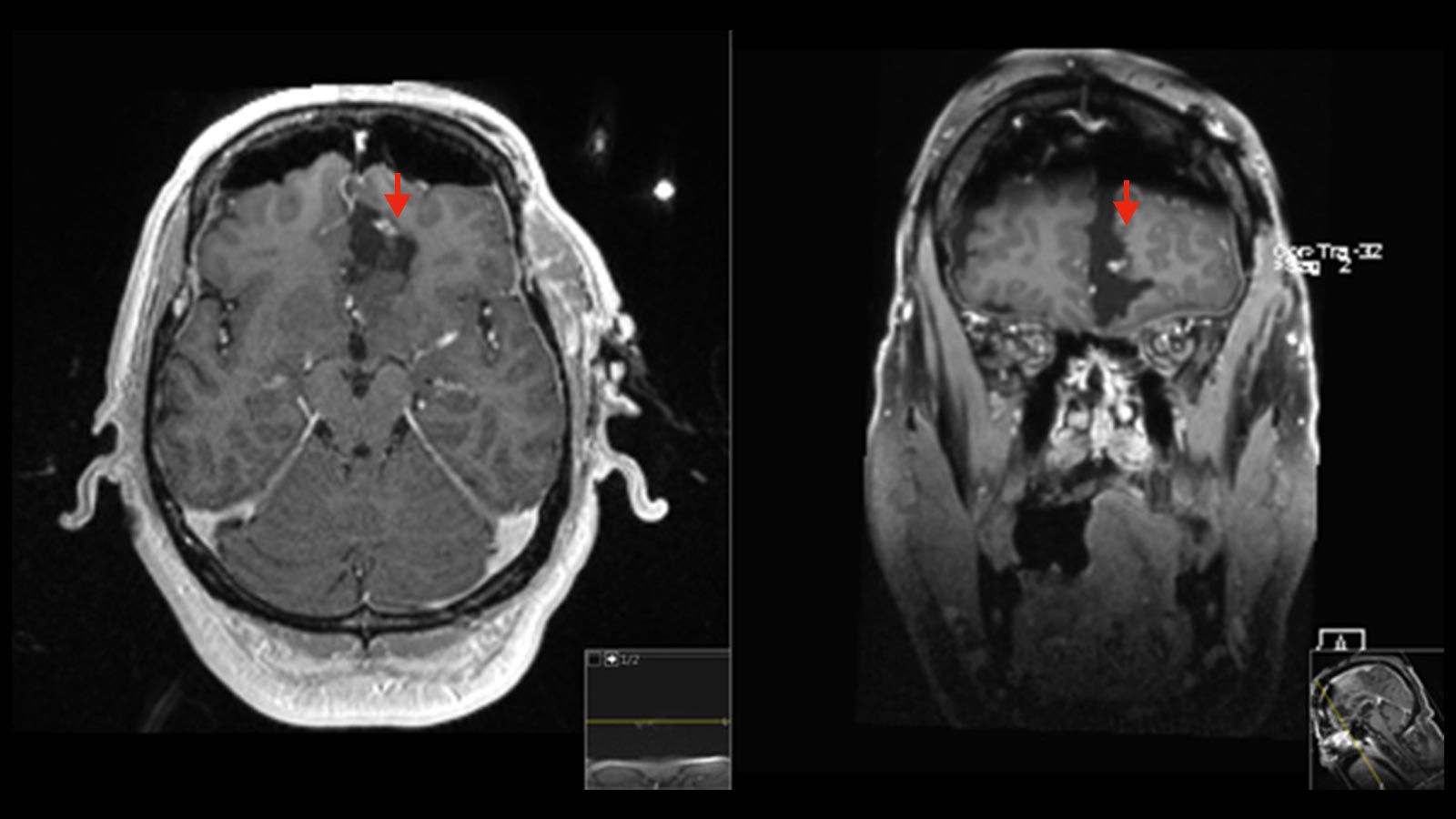
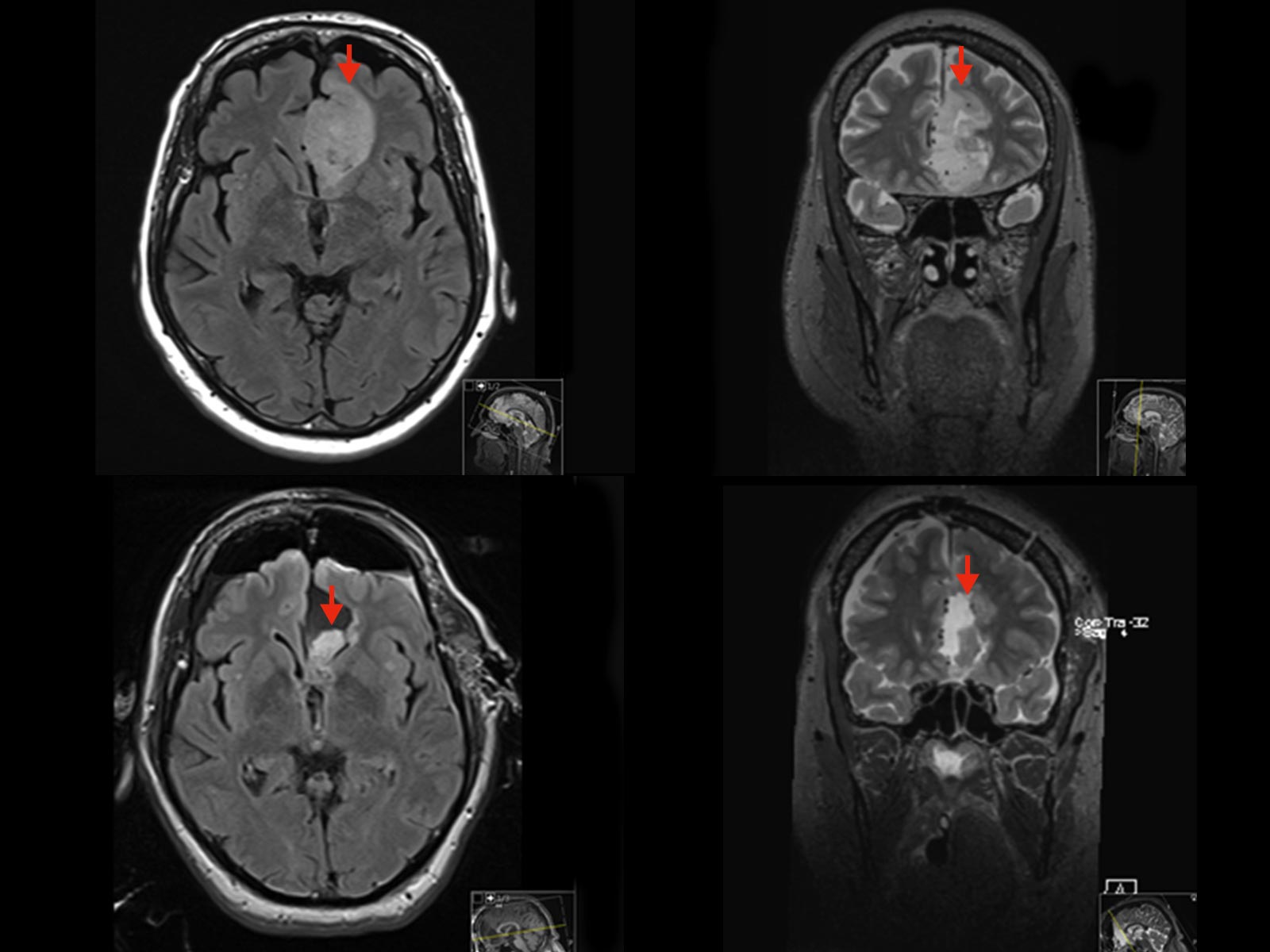
In the case of brain tumors, the extent of the tumor resection correlates with the patient's survival rate. The more of the tumor can be removed, the better the prognosis for the patient.
Our aim is to achieve a supramarginal resection for low-grade gliomas or metastases. In supramarginal resection, an additional safety margin of 1–2 cm is removed around the tumor in order to include tumor cells that extend beyond the visible margin. In highly malignant gliomas, complete resection of the tumor cells that absorb the contrast medium is the primary goal. Nevertheless, there are cases in the medical literature of tumors that were categorized as completely removed before surgery, but in about 40–70% of cases were not completely removed.
The iMRI should help us to reliably remove tumors as completely as possible. To protect neurological functions, this must be supported by other technologies such as neuromonitoring.
In functional neurosurgery, iMRI is used for deep brain stimulation (DBS). With the help of iMRI, the correct position of the electrodes can be checked immediately after the procedure and corrected if necessary.
Intraoperative computed tomography (iCT)
Intraoperative computed tomography (iCT) is frequently used in spinal surgery.
During spinal surgery, there is a high rate of suboptimally placed screws when implants are inserted to stabilize vertebrae. Recent study data show that intraoperative imaging reduces the rate of incorrectly inserted pedicle screws by 15–16% *. At the end of the surgical procedure, an intraoperative position check can be carried out using a final CT scan and, if necessary, an incorrect position of the screws can be detected and corrected. This significantly reduces the risk of a follow-up operation to reposition the screws.
Intraoperative digital subtraction angiography
In the endovascular treatment of vascular diseases and malformations such as aneurysms or arteriovenous malformations, intraoperative DSA enables better visualization of the anatomy of vessels and hidden structures. This subsequently leads to better surgical results.
Intraoperative ultrasound
Intraoperative ultrasound (iUS) is a versatile and cost-effective tool that provides surgeons with real-time support during surgery. iUS can be used to detect residual tumor tissue and compensate for brain shifts without significantly interrupting the surgical procedure. In combination with 3D or contrast-enhanced techniques, the benefits for patients could increase even further in the future.
Today, iUS is an integral part of modern glioma surgery or is used to guide the insertion of brain drains (e.g., insertion of VP shunts or external ventricular drainage).
Future intraoperative imaging
Positron emission tomography (PET) is a diagnostic imaging procedure in nuclear medicine that can be used to visualize metabolic activities in tissue. It is primarily used to detect tumors and metastases.
At the end of 2020, the world's fastest PET-CT scanner was put into operation at Inselspital's Department of Nuclear Medicine. This state-of-the-art scanner enables excellent examination quality with shorter examination times and reduced radiation exposure for our patients.
-
Fichtner J, Hofmann N, Rienmüller A, Buchmann N, Gempt J, Kirschke J et al. Revision Rate of Misplaced Pedicle Screws of the Thoracolumbar Spine–Comparison of Three-Dimensional Fluoroscopy Navigation with Freehand Placement: A Systematic Analysis and Review of the Literature. World Neurosurgery. 2018;109:e24-e32.
Further reading
Fahlbusch R, Golby A, Prada F, Zada G. Introduction: Utility of intraoperative imaging. Neurosurgical Focus. 2016;40(3):E1.
Giordano M, Samii A, Lawson McLean A, Bertalanffy H, Fahlbusch R, Samii M et al. Intraoperative magnetic resonance imaging in pediatric neurosurgery: safety and utility. Journal of Neurosurgery: Pediatrics. 2017;19(1):77-84.
Knauth M, Wirtz C, Tronnier V, Staubert A, Kunze S, Sartor K. Intraoperative MRI to control the extent of brain tumor surgery. Der Radiologe. 1998;38(3):218-224.
Raabe A, Fichtner J, Gralla J. Advanced intraoperative imaging. Clinical and Translational Neuroscience. 2017;1(1):2514183X1771831.