Herniated discs along the entire spine are usually the result of aging and wear and tear. However, a herniated disc in the thoracic spine, also known as thoracic disc herniation or thoracic disc hernia, is much rarer than a herniation in the cervical or lumbar spine, since the thoracic spine receives additional support from the ribs. Symptoms can start insidiously and be diffuse, which is why the diagnosis is sometimes delayed.
There are also often herniated discs without symptoms which are discovered by chance and do not require therapy. Surgery is only indicated when there are more severe symptoms and considerable compression on the spinal cord or nerves. Since the herniated discs of the thoracic spine are usually calcified, the operation is technically very demanding. It often has to be performed from the side through the thoracic cavity or transdurally, through the cerebrospinal canal, if the herniated disc is located directly behind the spinal cord and is not of soft consistency.
Why you should seek treatment at Inselspital
At Inselspital specialists from all disciplines work closely together under one roof and coordinate with each other through guidelines and internally defined standards, among other aspects. Thanks to the cooperation of neurosurgery with orthopedics, rheumatology, physiotherapy, neurology, neuroradiology and the pain center, the optimal treatment strategy can be developed for each patient on an interdisciplinary basis. Complicated cases are discussed in an interdisciplinary board and often operated on jointly by neurosurgeons and orthopedists. In this way, we create the conditions for the best possible treatment for each individual patient.
A specialized spine team of our neurosurgical department is responsible for an operation to decompress the nerve structures in the thoracic spine. In this type of surgery, our specialists perform the approach to the spinal cord through the thoracic cavity together with thoracic surgeons or orthopedic surgeons.
How common are thoracic disc hernias?
Less than 1% of all herniated discs are located in the thoracic spine. Middle-aged people (between 40–60 years) are most likely to develop a thoracic disc herniation. Men are affected slightly more often than women. All details on the causes can be found on the overview page Herniated disc.
What are the most common symptoms?
Symptoms caused by a herniated disc in the thoracic spine are often unspecific, which can make it difficult to make a correct diagnosis.
Common symptoms are:
- Local pain in the back
Sometimes the pain is also felt in the chest or abdomen. - Radiating nerve pain
If the descending spinal nerve is affected, there is classically a girdle-shaped pain in the chest area or sensory disturbances. - Myelopathy
If the spinal cord is compressed, damage to the spinal cord (myelopathy) can occur with neurological deficits below the lesion. These can range from mild sensory or coordination disorders of the legs to marked disorders such as urinary incontinence or, rarely, a high-grade paraplegic syndrome.
How is a thoracic disc herniation diagnosed?
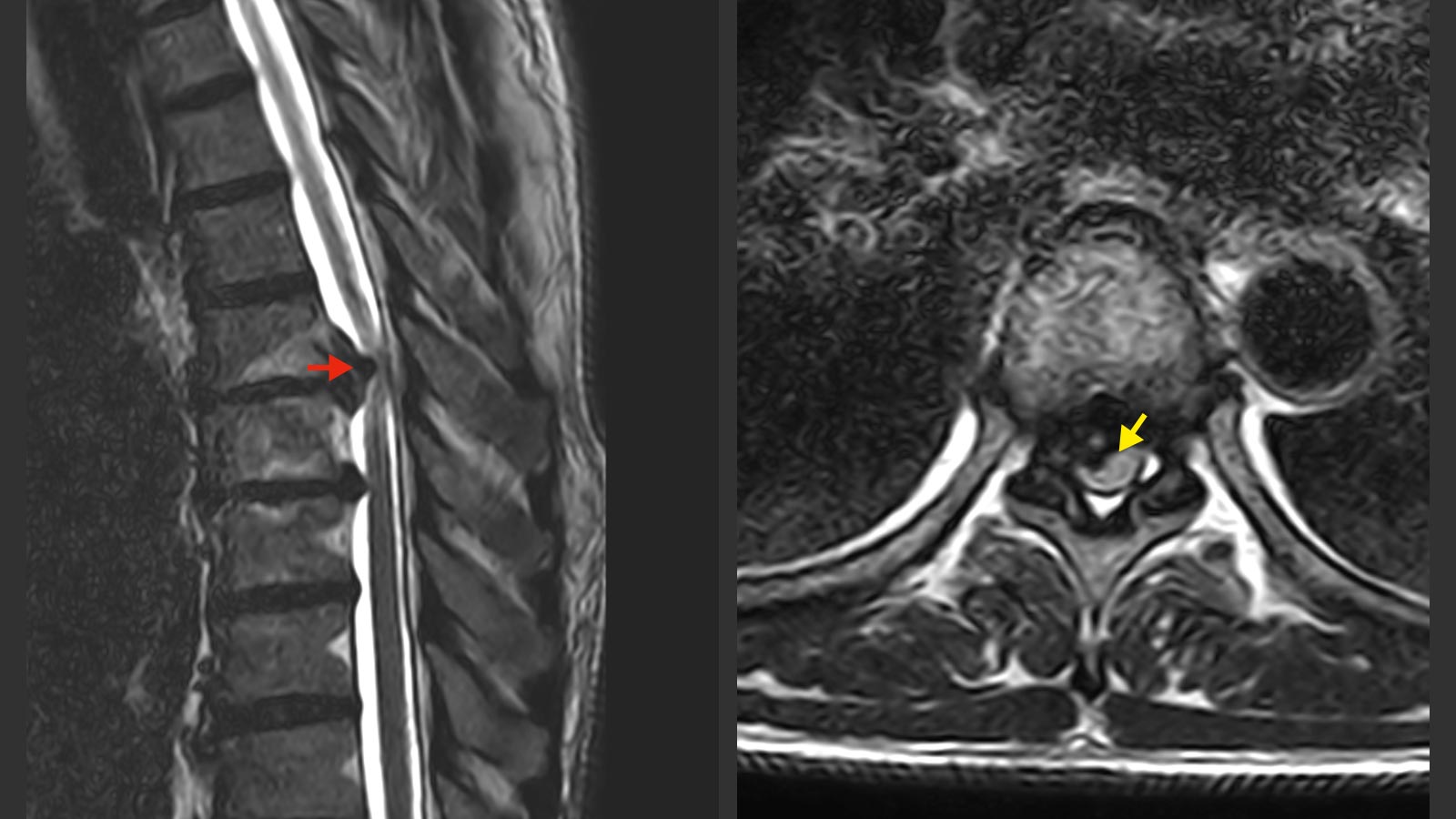
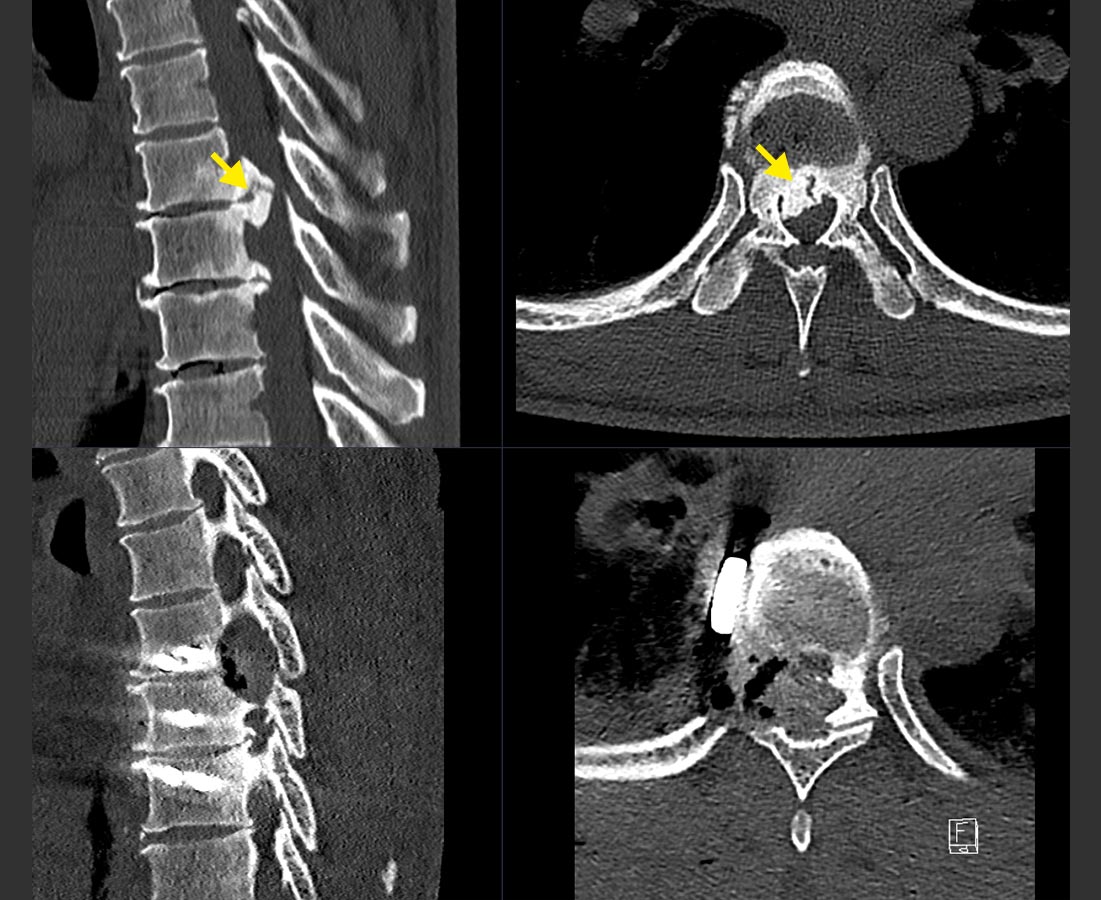
Every diagnosis is preceded by a detailed interview and focused neurological examination. The clinical suspicion must then be confirmed with imaging. The imaging of choice is magnetic resonance imaging (MRI). This is the best way to visualize nerves, the spinal cord and the herniated disc. A large number of disc hernias in the thoracic spine are calcified. Therefore, it is important for surgical planning to also perform a computed tomography (CT).
Rarely, additional examinations such as an electrophysiological measurement of the nerve function (evoked potentials) are necessary to make a therapy decision regarding surgery or further conservative treatment.
What are the treatment options?
If the compression of the nerve only causes pain and no other symptoms, a thoracic disc herniation is treated conservatively with pain medication and physiotherapy. If the patient's pain does not improve or paralysis persists, surgery should be considered.
If neurological disorders have developed as a result of the nerve compression, surgery is unavoidable. In the case of a thoracic disc herniation, a diagnosed myelopathy is often the reason for surgery. The aim of the operation is to stop the spinal cord damage from progressing. In many cases there is also a neurological improvement after the operation, but the extent of the recovery is often incomplete despite the operation and depends on the severity of the previous damage.
Surgical procedures for thoracic disc herniation
Surgery for thoracic disc herniation is challenging for two reasons.
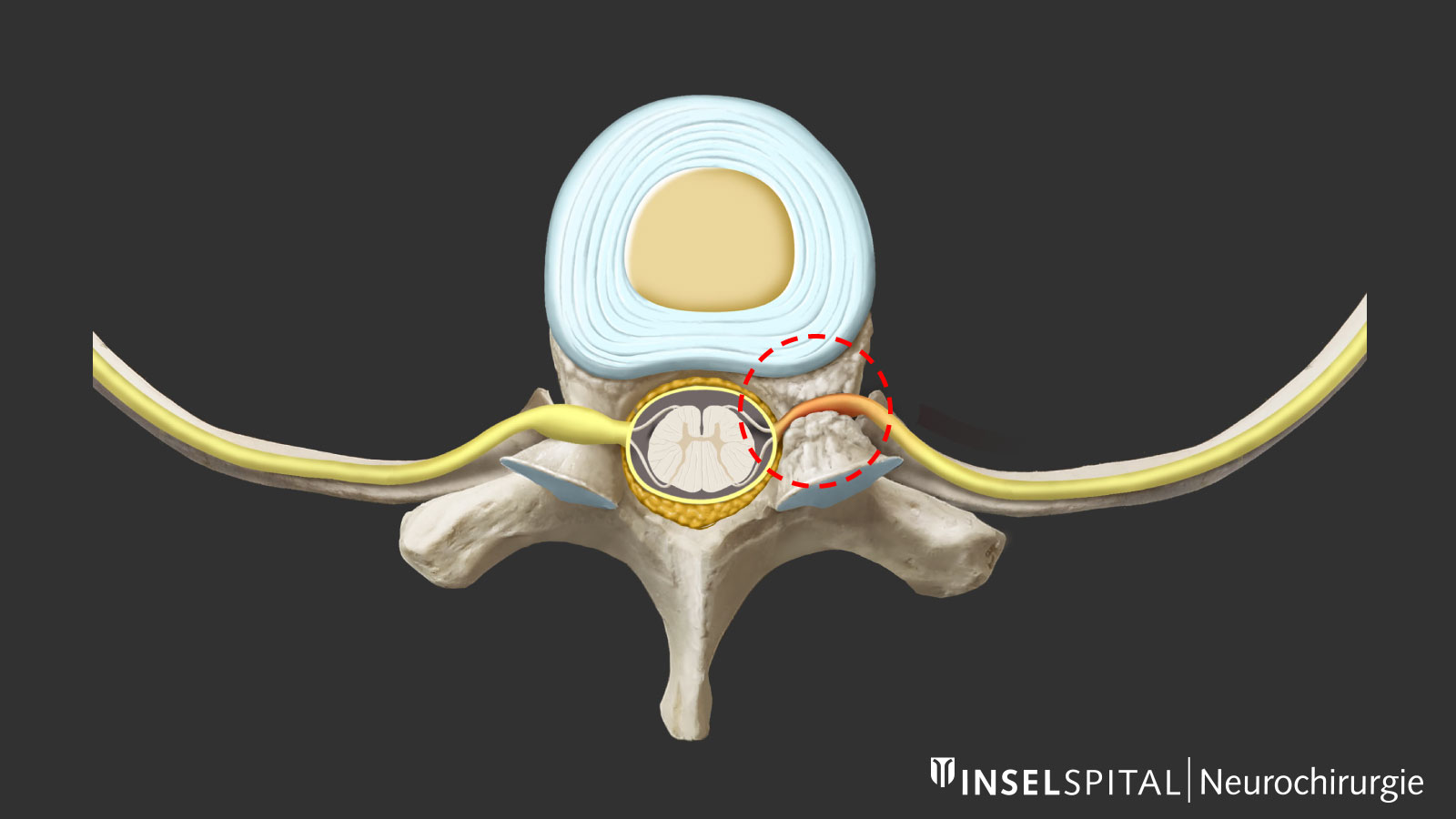
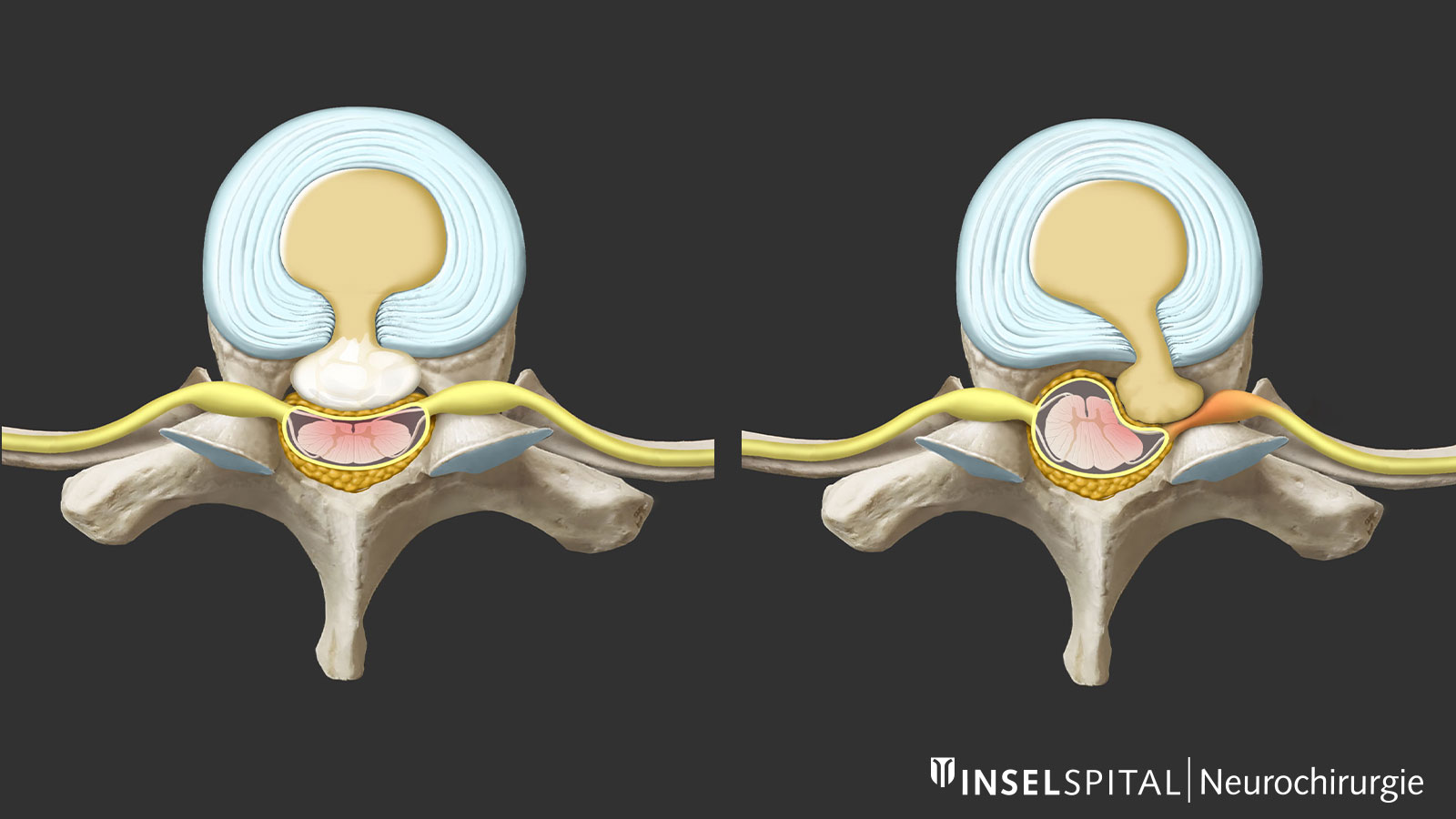
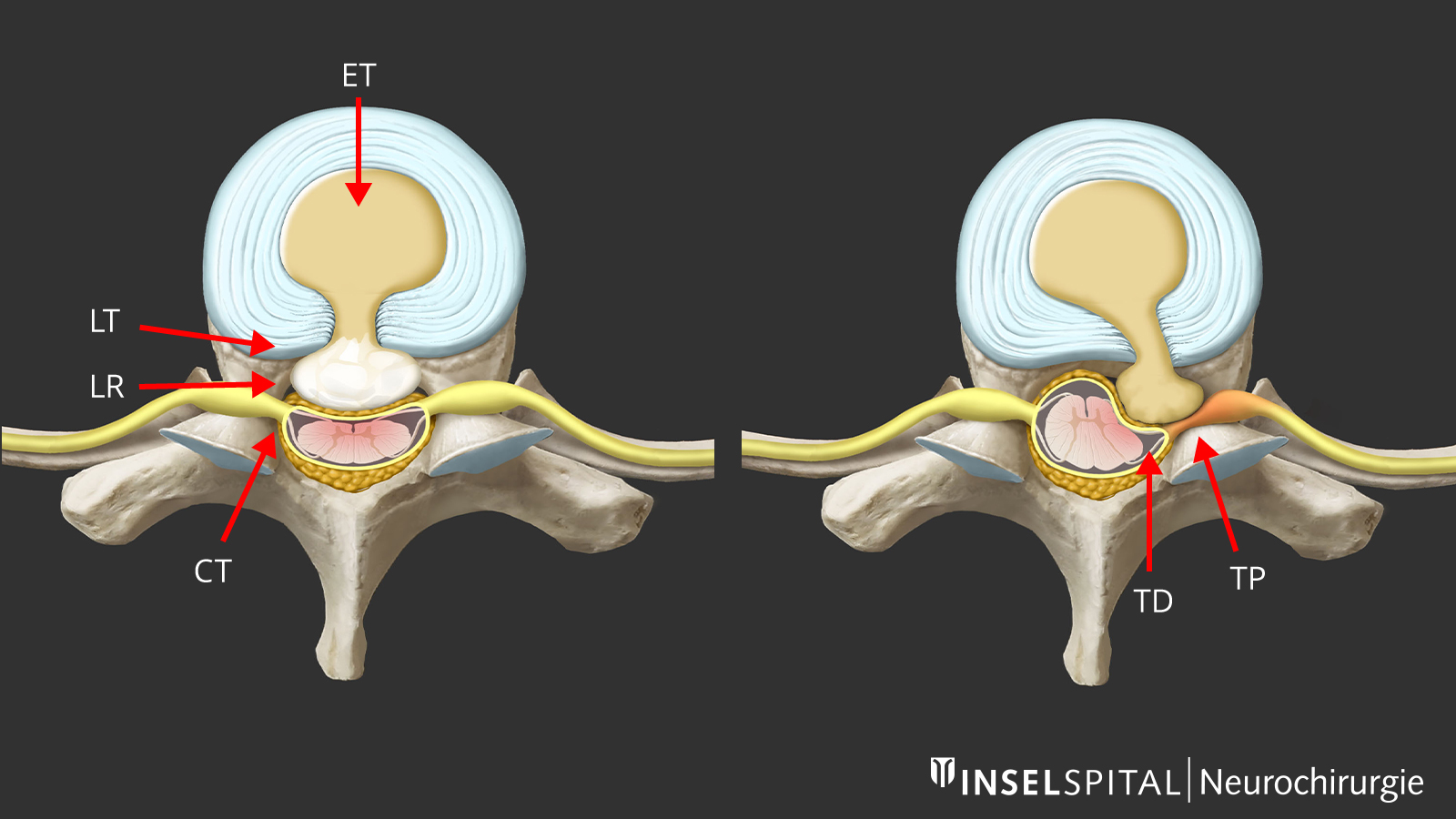
- Anatomical situation
The spinal cord (myelon) blocks the path to the herniated disc. It is therefore particularly important to plan the approach precisely in order to affect the myelon as little as possible. The classic approach is the transpedicular approach with unilateral removal of the vertebral arch root or the costotransversectomy with resection of the rib attachment. In this case, one passes the spinal cord diagonally and can remove a soft disc herniation. In the case of an ossified herniated disc, one often has to operate strictly from the side by spreading two ribs. This reduces the mobilization of the spinal cord. Because the working channel is very deep and the operation is nevertheless performed via a minimally invasive approach, this technique is very demanding. - Calcifications
Due to deposits and calcifications, the consistency of the thoracic disc hernia is often very hard. Manipulation immediately adjacent to the spinal cord is therefore riskier than for other disc hernias. Due to the proximity to the spinal cord, the risk of neurological deterioration is greater than in cervical spine surgery and, in our view, always requires intraoperative neuromonitoring of motor evoked potentials and D-wave.
Treatment of foraminal stenosis of the thoracic spine
Local narrowing of the nerve exit hole (foramen) can cause isolated compression of the intercostal nerve. This narrowing manifests itself in stabbing, pulling or burning pain radiating from the spine along a rib. Therapy consists of local minimally invasive decompression of the nerve via a direct approach to the back.