Episodic pains in the region of the ear, tongue, throat, and tonsils are characteristic of this rare neuralgia. These pain attacks are triggered by irritation of the glossopharyngeal nerve, also known as the pharyngeal nerve. This can occur, for example, through chewing, swallowing, speaking, or other forms of pressure application. In cases where medications provide no relief, neurosurgery offers a promising treatment option. A specific minimally invasive operation has proven effective and long-lasting in relieving pain in more than 85% of our patients.
How common is glossopharyngeal neuralgia?
Glossopharyngeal neuralgia is a rare condition compared to other forms of facial and head pain. It is very uncommon, with a prevalence of 0.2–1.3% among all facial pain syndromes, and it tends to affect older individuals more frequently. However, it can potentially occur at any age.
What are the symptoms of glossopharyngeal neuralgia?
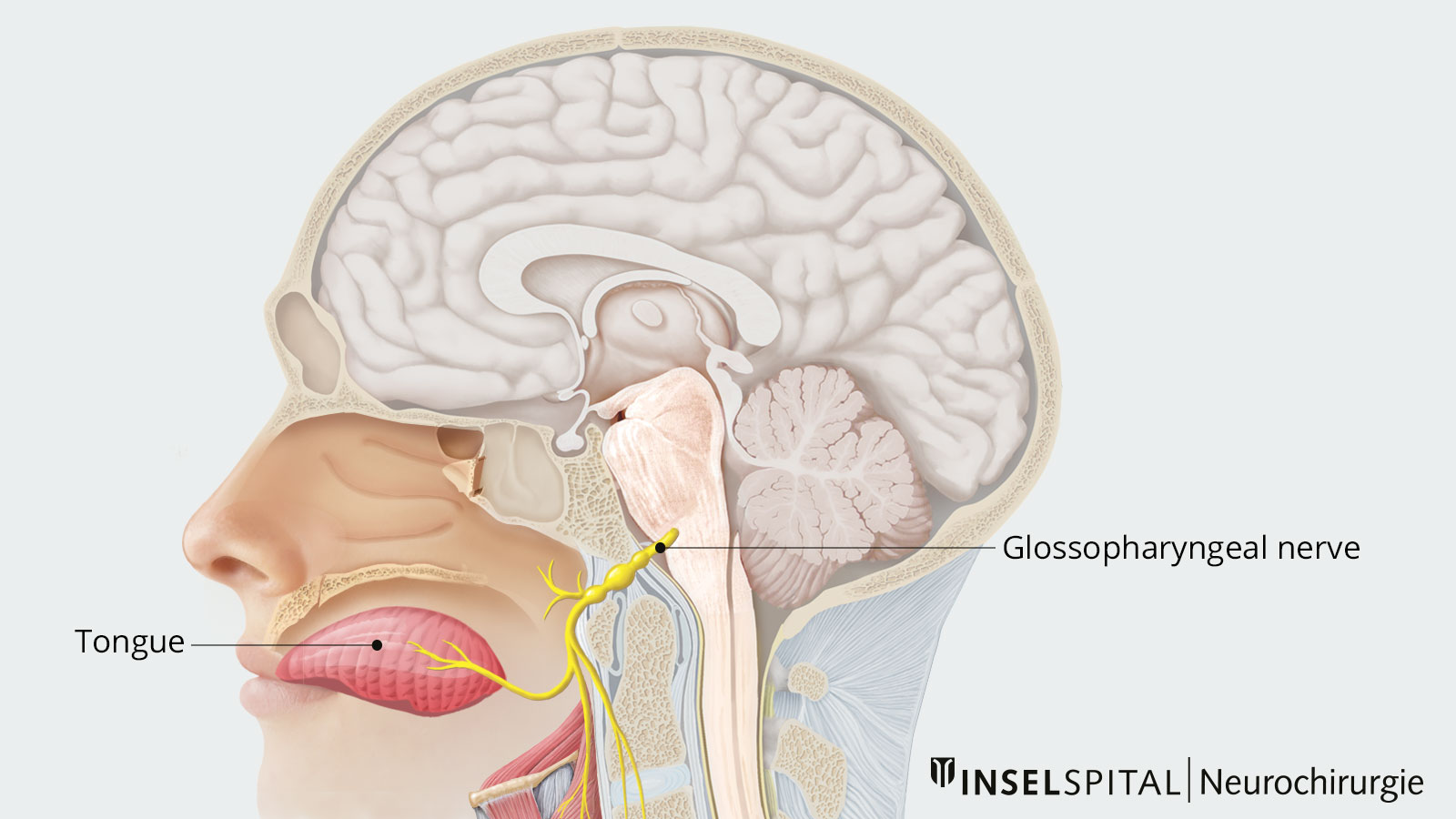
The glossopharyngeal nerve is a sensorimotor nerve, meaning it contributes to the movement of the pharyngeal muscles and transmits information from the pharynx, tonsils and tongue to the brain. The Greek name of this IX cranial nerve describes its area of supply. It includes, together with the vagus nerve, the pharynx sensory and motor, but also secretory the parotid gland and the glands of the base of the tongue, and with its taste fibers the posterior third of the tongue.
Accordingly, glossopharyngeal neuralgia is characterized by severe, shooting, usually unilateral and left-sided pain that often begins in the equilateral pharyngeal, cervical, tonsillar, lingual, and auricular regions and usually lasts only for a few seconds. The episodes of pain are typically triggered by swallowing, chewing, coughing, yawning, talking or touching. Affected patients often begin eating less out of fear of the pain and rapidly lose weight.
Spontaneous improvement of glossopharyngeal neuralgia within 6 months is not uncommon. However, if pain persists, a symptomatic cause must be ruled out and further treatment options considered.
What causes glossopharyngeal neuralgia?
In rare cases, glossopharyngeal neuralgia can be an expression of a specific pathological change, for example, a tumor, a vascular abnormality, an inflammation or an adhesion near the nerve. Much more common, however, are the classic idiopathic cases with no identifiable cause.
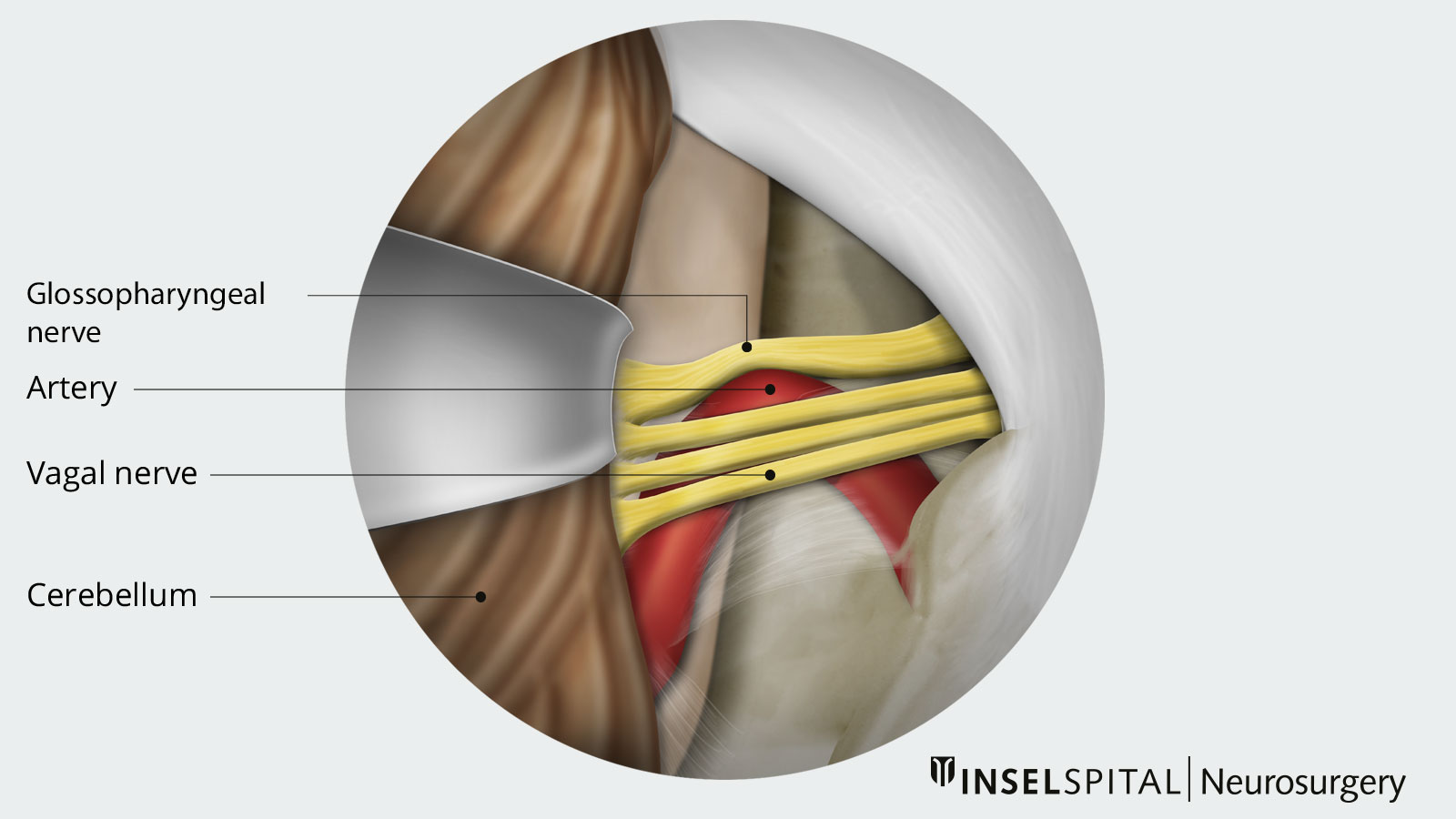
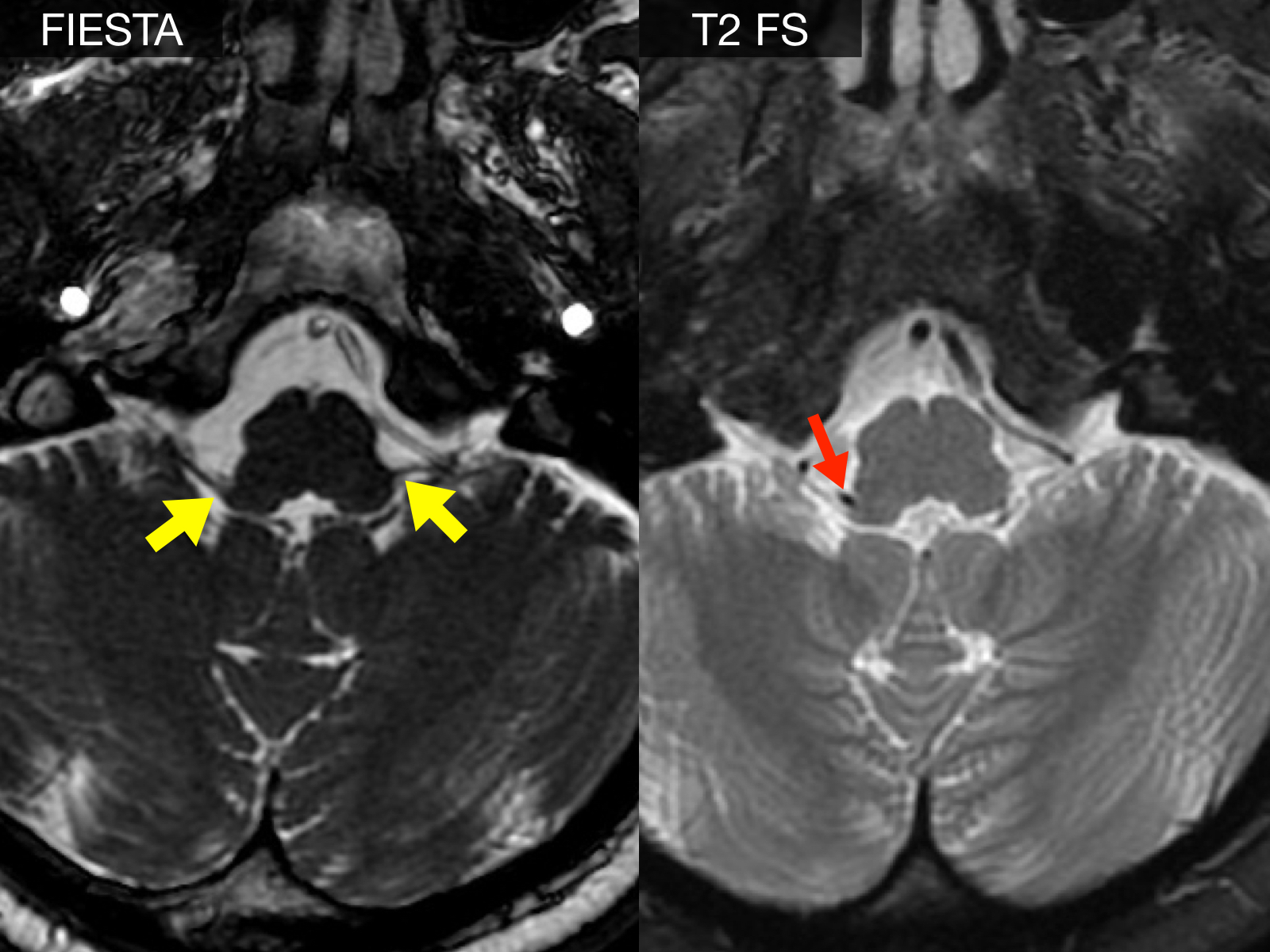
Pathophysiologically, it appears that electrical impulses may jump to pain fibers due to damage to the nerve sheaths in response to tactile stimuli. The lesions in the nerve sheaths may be attributed to natural mechanical wear and tear due to the aging process or could result from chronic exposure to nearby pulsating blood vessels (see also neurovascular conflict under "What causes trigeminal neuralgia?").
How is the diagnosis made?
For evaluation and to rule out space-occupying lesions, it is advisable to undergo a Magnetic Resonance Imaging (MRI) of the skull. This can help diagnose a potential neurovascular conflict or a tapered petrous apex of the skull base.
What are the treatment options?
In rare symptomatic forms of glossopharyngeal neuralgia, the underlying cause is treated when possible.
Conservative treatment
In more common cases of idiopathic glossopharyngeal neuralgia, where a cause cannot be diagnosed, drug treatment, usually with carbamazepine, is used initially. This involves increasing the dose of medication until the pain episodes stop.
Surgical treatment
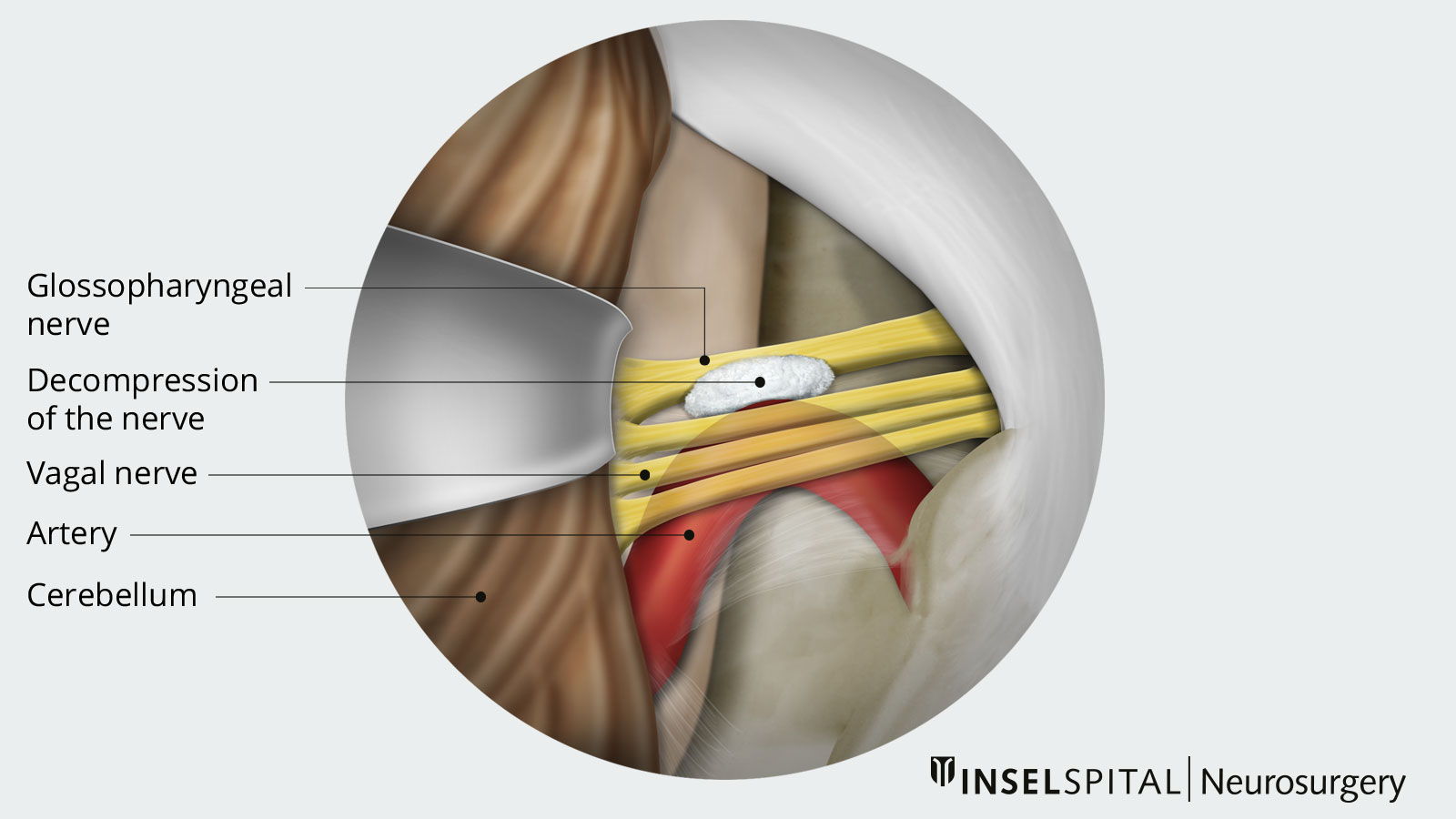
If conservative therapy fails despite adequate dosing or if significant medication side effects occur, consideration should be given to neurosurgical intervention. Currently, worldwide, non-destructive microsurgical neurovascular decompression according to Janetta is the procedure of choice.
In our clinic, we use minimally invasive techniques and a surgical microscope to examine the course of the glossopharyngeal nerve and free it from pulsating vascular loops that cause nerve irritation.The troublesome vessel is kept away from the nerve with the help of a Teflon mesh. Throughout the entire procedure, our neurophysiological monitoring is performed to ensure the safety of our patients.
Why you should seek treatment at Inselspital
For our specialists at Inselspital, microvascular decompression is a standard procedure for glossopharyngeal neuralgia. While it is more commonly used for trigeminal neuralgia, the technique is identical. The long-term results of this operation are extremely positive, with over 85% of patients experiencing a significant and lasting improvement in their pain following the procedure.