Radiosurgery is a specialized form of radiotherapy and an important component of modern neurosurgery. It involves high-precision radiation, allowing for the millimeter-accurate and highly intensive irradiation of a specific target point in the brain without invasive intervention. Radiosurgery maximizes the therapeutic effect of radiation on diseased tissue without damaging healthy brain tissue.
For which diseases do we use radiosurgery?
Surgeries in specific brain regions carry a high level of risk. They can be entirely or partially avoided by opting for radiosurgical treatment instead.
Radiotherapy is used for:
- Various benign or malignant brain tumors
- Vascular malformations
- Functional disorders (such as trigeminal neuralgia, focal epilepsy, or tremor)
Radiosurgery can be used alone or in combination with microsurgical or endovascular techniques.
To achieve the best possible treatment for each individual patient, at Inselspital, every patient case is individually evaluated and discussed by an interdisciplinary team of physicians. Together, the patients for whom radiosurgery is indicated are determined.
How does radiosurgery treatment work in our clinic?
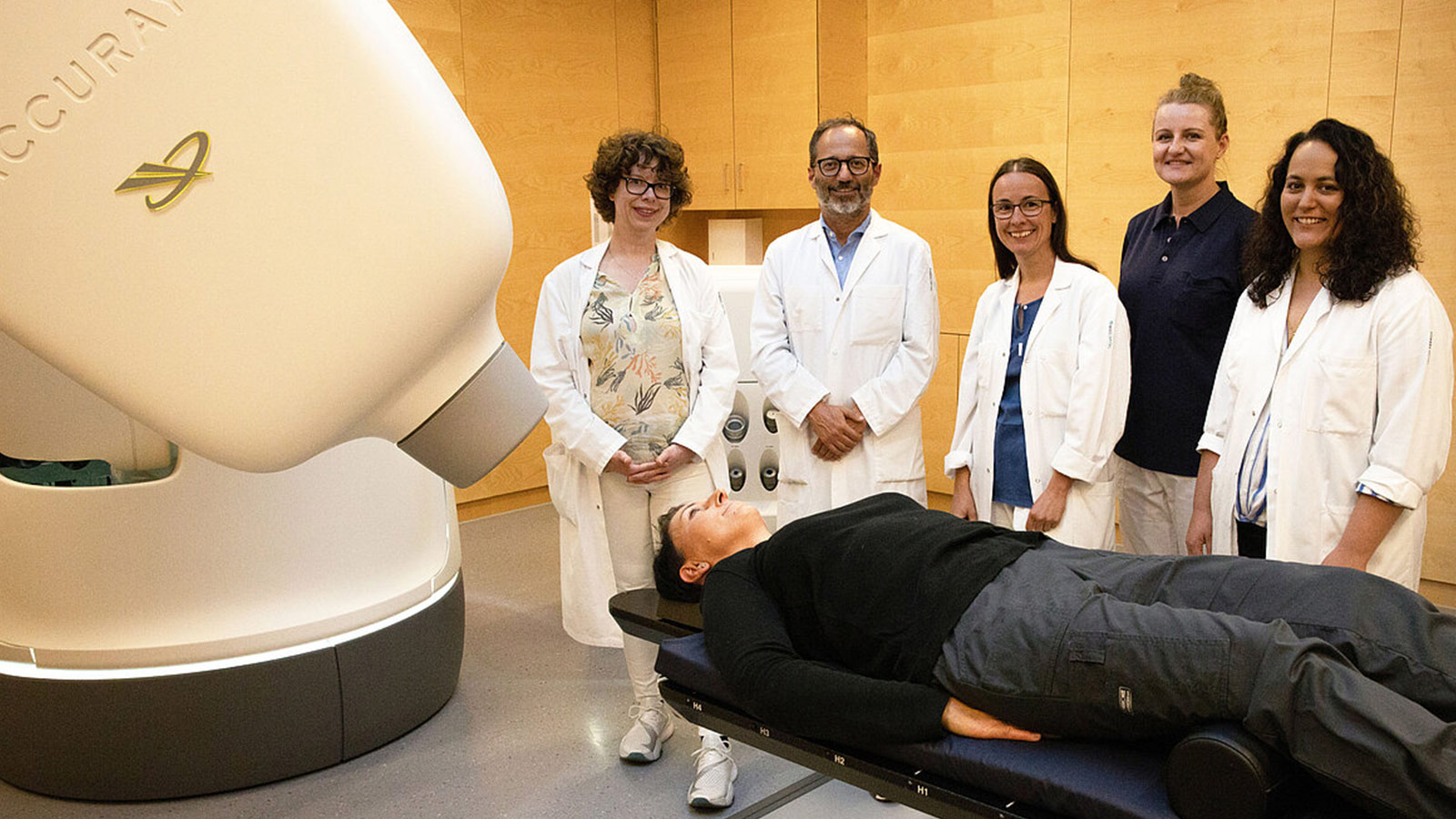
During the preparation and execution of the radiation, neurosurgeons, radiation oncologists, physicists, and medical-technical radiology assistants (MTRA) work closely together. For precise radiotherapy, good pre-planning using imaging techniques such as computed tomography (CT) and magnetic resonance imaging (MRI) is very important.
Step 1: Initial consultation
During the first outpatient consultation, the doctor will inform you about the procedure, results, risks, and possible side effects of the treatment (headaches, fatigue, dizziness). If radiation is considered, you will be notified in writing of your radiation appointment.
Step 2: Mask
For the treatment, the production of a mask is necessary in advance. The radiation mask consists of four layers, each softened in warm water to precisely conform to your head and facial shape. Similar to the stereotactic frame, a plexiglass box is attached to the mask, representing a three-dimensional coordinate system for CT imaging. This allows for the accurate determination of the volume of the lesion or region to be treated and the boundaries of the radiation area.
The production of the mask requires one or more outpatient appointments.
Step 3: Imaging
In addition to the radiation appointment, you will be scheduled for MRI and CT examinations.
Blood may be drawn from you to determine kidney function blood values. This is necessary if a contrast agent needs to be injected during the imaging examination.
In the case of an angiography, it will be performed directly on the day of treatment with the frame setup (stereotactic angiography).
Step 4: Radiation treatment plan
Physicists, radiation oncologists, and neurosurgeons plan the radiation based on the CT images, MRI images, and other examinations. They determine the radiation parameters – including the size, shape, and arrangement of the radiation fields. This very complex process takes several hours. The complete radiation plan is finalized by the time of the initial irradiation.
Step 5: Radiosurgical treatment
One of the most advanced devices for radiosurgical treatment, the so-called CyberKnife®, is used at our clinic. The CyberKnife is programmed with the position of the tumor based on CT and MRI images. Using an integrated X-ray system, the programmed data is continuously compared with real-time images during irradiation, and tumor movements (deviations) are immediately corrected.
A stereotactic CT can be performed with a mask. If an angiogram is required, it will be performed separately. On the treatment table of the radiation device, you will be positioned precisely in the radiation mask, exactly as in the previous CT scan. A stereotactic frame is applied under local anesthesia and removed immediately after irradiation.
The treatment is closely monitored by the attending physicians and technical personnel. They are in constant contact with the patient via video and voice transmission. You will not feel anything during the irradiation itself. The duration of the irradiation depends on the complexity of the irradiation plan and can range from 20 minutes to 1.5 hours.
Step 6: End of treatment
Following the irradiation, the mask is removed, and you can go home. However, due to possible side effects, we ask that you do not drive yourself home but instead come accompanied. In certain cases, you may need to stay at Inselspital for one day for monitoring.
What is CyberKnife technology?
At our clinic, one of the most modern devices for radiosurgical treatment, called CyberKnife®, is utilized. This advanced system combines various cutting-edge technologies, including:
- a highly precise, computer-controlled robotic arm with integrated imaging
- a high-resolution multileaf collimator (MLC) for the precise irradiation of larger tumors
- an image-guided tumor localization system
- an advanced patient positioning system
The CyberKnife® is the only non-invasive, robotically controlled radiosurgical system for the highly complex and millimeter-accurate irradiation of tumors at any location in the body. The interplay of these technologies allows irradiation from over a thousand different angles. This enables tumors or metastases in sensitive body areas such as the brain to be safely irradiated while maximizing the preservation of surrounding healthy tissue.
Unlike the widely used Gamma Knife, the radiation is not generated by a radioactive substance (Cobalt-60) but by a linear accelerator. This ensures that the emitted radiation dose is precisely known and does not decrease with the age of the radiation source.

What is the difference between radiosurgery and normal radiotherapy?
Sensitivity of cells to ionizing radiation
The sensitivity of cells to ionizing radiation varies greatly among different body tissues and depends largely on how quickly a tissue regenerates or grows.
In every tissue, including tumors, there are cells that are very insensitive to radiation because they are in a resting phase. This means that their genetic material, DNA, is highly compacted, and repair mechanisms effectively counteract the DNA damage caused by radiation.
In rapidly dividing tissues, a large proportion of cells are in the phase of cell division at any given time. During the cell division phase, the genetic material is particularly sensitive to radiation.
Conventional radiation therapy
In conventional (fractionated) radiation therapy, the aim is to increase the proportion of destroyed tumor cells by irradiating for several consecutive days. A largely selective damage to the tumor is achieved by allowing healthy tissue to recover between treatments with the administration of the total radiation dose in small portions (1–2 Gray per session), while tissues from radiation-sensitive and rapidly dividing tumors may recover less effectively. However, this requires sensitivity of the tissue being treated to radioactive radiation.
Radiosurgical therapy
In contrast, radiosurgery utilizes the particular technique of radiation focusing. This means that, due to the millimeter-precise precision of this technique, physicians can administer a very high radiation dose without damaging surrounding radiation-sensitive tissue. This allows even cells in resting phases to be sufficiently damaged. Radiosurgical treatment is usually a one-time irradiation, administered in a single treatment session.
Our experience at Inselspital
At Inselspital, every indication and planning of radiosurgical treatments are carried out by an interdisciplinary team of experts consisting of specialists in radiation oncology, neuroradiology, neurosurgery, neurology, and oncology. This allows for the best possible treatment to be achieved for each individual patient.
The advantages of radiosurgical treatment include:
- Short treatment duration (1–5 days)
- No surgical opening of the skull
- Mostly outpatient treatment (admission and discharge on the same day)
- Short treatment time (between 20 minutes and 1.5 hours – depending on the size and number of lesions to be treated)
- Short sick leave (1–2 days)
- Treatment covered by health insurance without prior cost approval.
