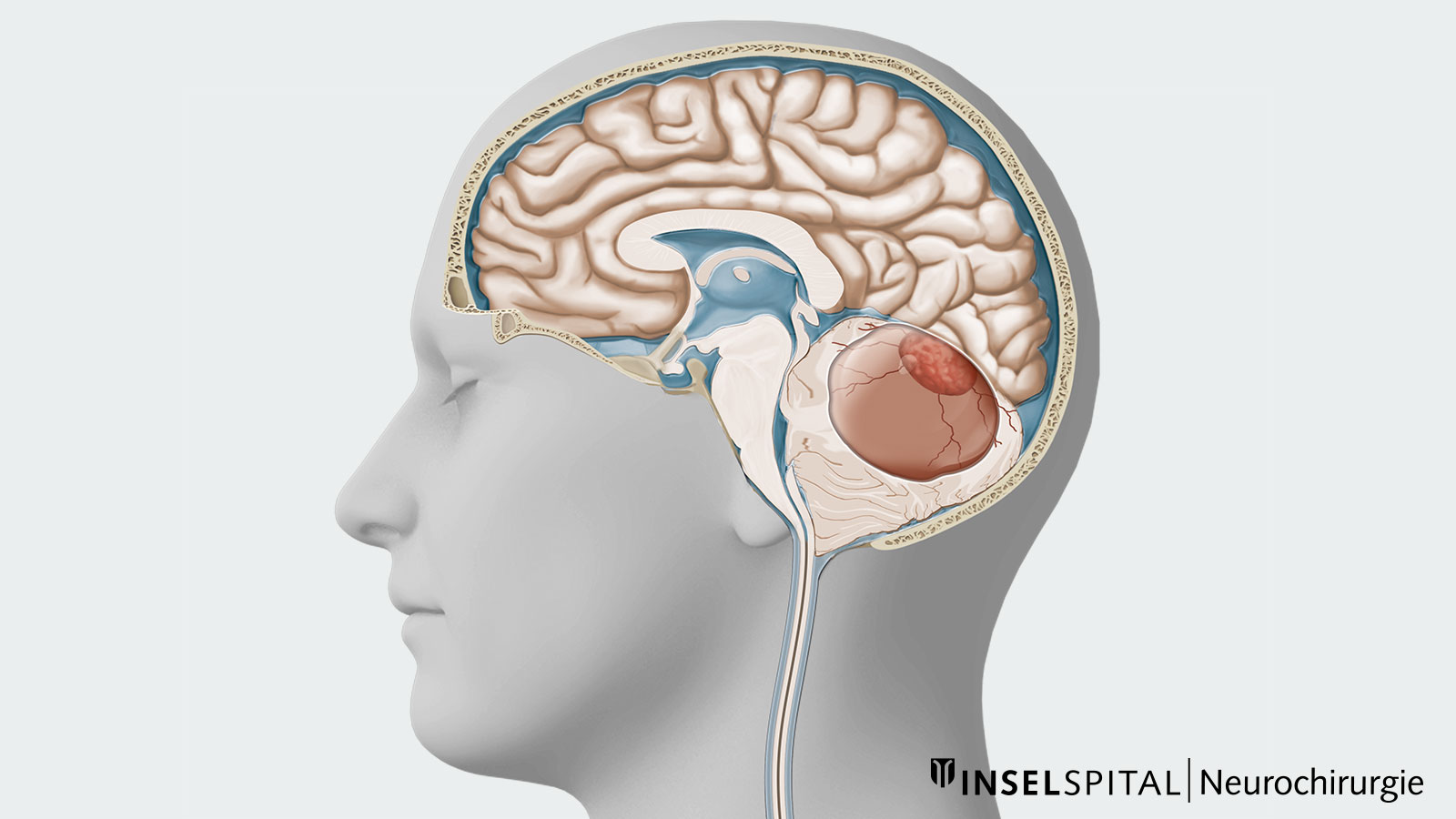
A hemangioblastoma is a rare, benign and extremely vascular tumor of the central nervous system. In addition to a solid nodule, hemangioblastomas often have cystic parts. Hemangioblastomas are usually localized in the cerebellum, brain stem or spinal cord. Microsurgical removal is the treatment of first choice. The difficulty of the operation depends on the size, location and nature of the tumor. In patients with multiple hemangioblastomas or in patients with Von Hippel-Lindau disease, surgery is performed only on those tumors that are causing symptoms or growing.
Who is affected by hemangioblastomas?
Hemangioblastomas are rare tumors of the central nervous system. They often occur sporadically, but can also be due to Von Hippel-Lindau syndrome (VHL). For this reason, further clarification should be performed for every newly diagnosed hemangioblastoma. *
Hemangioblastomas represent about 2% of all primary brain tumors. 85% of them are localized in the cerebellum. * Rarely, hemangioblastomas grow in other locations:
- in the area of the cervical spinal cord (< 10%)
- in the brain stem (< 5%)
- in the cerebrum (< 2%)
80% of all hemangioblastomas are sporadic and typically occur in the 4th decade of life. * The manifestation of VHL-associated hemangioblastomas is earlier. Most patients develop the disease between the ages of 20 and 40. *, *
While sporadic hemangioblastomas are usually single tumors, they are often multiple in Von Hippel-Lindau syndrome. Up to 84% of patients with VHL develop a hemangioblastoma. *
Von Hippel-Lindau syndrome (VHL)
Von Hippel-Lindau syndrome was first described at the beginning of the 20th century by the German ophthalmologist Eugen von Hippel and the Swedish pathologist Arvid Lindau. The disease is inherited in an autosomal dominant manner and is based on a mutation of the tumor suppressor gene VHL. The mutation leads to the appearance of a variety of benign and malignant tumors:
- hemangioblastomas of the central nervous system
- hemangiomas of the retina
- clear cell renal cell carcinomas and renal cysts
- pheochromocytomas
- serous cystadenomas
- neuroendocrine tumors of the pancreas
- endolymphatic tumors of the middle ear
- papillary cystadenomas of the testis
For the diagnosis of VHL, one or more tumors must be present, depending on family history. Genetic tests are also available. In general, genetic counseling involving the entire family is very important for this hereditary disease. *
What symptoms does a hemangioblastoma cause?
When a hemangioblastoma grows and compresses the brain tissue locally, it can cause symptoms. Acute bleeding is rather rare. Rather, hemangioblastomas cause symptoms typical of cerebellar impairment. Patients report symptoms such as headaches, nausea, vomiting, disturbances in gait and balance, double vision and disturbances in fine motor skills. These deficits are partly due to direct damage to the cerebellar tissue, partly also caused by pressure on the brain stem or increased intracranial pressure due to congestion of cerebrospinal fluid. *
Less common hemangioblastomas in the spinal cord or brain stem cause similar neurological deficits. Hemangioblastomas in the area of the spinal cord can additionally lead to sensory disturbances in the extremities.
How is a hemangioblastoma diagnosed?
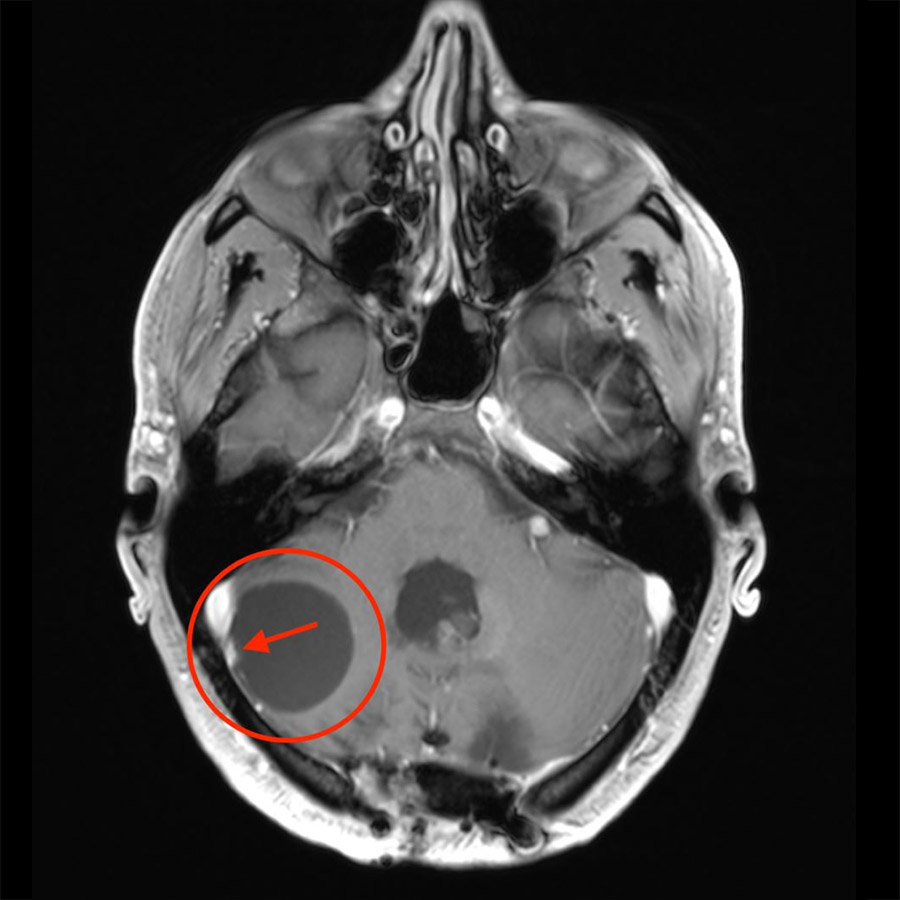
In the case of neurological complaints, a radiological examination is carried out using computer tomography (CT) or magnetic resonance imaging (MRI). MRI is the better method because of its higher resolution and more detailed soft tissue imaging. The imaging often shows a cystic mass and, after administration of contrast medium, only a small solid tumor nodule. However, the size of the solid and cystic parts can vary greatly in hemangioblastomas.
In addition to CT or MRI, digital subtraction angiography (DSA) can also be performed. In this procedure, a thin catheter is inserted into the artery in the groin and advanced to the brain. There, the cerebral vessels are then visualized via contrast medium injections. DSA may be necessary to detect the smallest solid parts of the tumor that cannot be visualized on CT or MRI, or to visualize the vascularization of the hemangioblastoma. However, for a definitive diagnosis fine tissue examination of the tissue samples after surgery is required.
What are the treatment options?
Microsurgery
Gentle microsurgical removal of hemangioblastoma is the treatment of choice. During the operation, the solid tumor nodule is removed and the cyst is relieved. Removal of the cyst wall is not necessary. In the case of individual hemangioblastomas, surgery is a curative therapy, i.e. no further therapies such as radiation or chemotherapy are necessary after surgery. 82‒98% of patients show an improvement in symptoms after surgical removal of the hemangioblastoma.
VHLS-associated haemangioblastomas recur more frequently and often occur in multiples. For this reason, they are only surgically removed if they cause symptoms, grow strongly or threaten important brain structures through their growth *
Radiosurgery
Stereotactic radiosurgery or fractionated radiation are used for inoperable tumors or for multiple tumors in different locations in order to avoid multiple surgical interventions. *
-
Kuharic M, Jankovic D, Splavski B, Boop F, Arnautovic K. Hemangioblastomas of the Posterior Cranial Fossa in Adults: Demographics, Clinical, Morphologic, Pathologic, Surgical Features, and Outcomes. A Systematic Review. World Neurosurgery. 2018;110:e1049-e1062.
-
Lonser R, Glenn G, Walther M, Chew E, Libutti S, Linehan W et al. von Hippel-Lindau disease. The Lancet. 2003;361(9374):2059-2067.
-
Bamps S, Calenbergh F, Vleeschouwer S, Loon J, Sciot R, Legius E et al. What the neurosurgeon should know about hemangioblastoma, both sporadic and in Von Hippel-Lindau disease: A literature review. Surgical Neurology International. 2013;4(1):145.
-
Wanebo J, Lonser R, Glenn G, Oldfield E. The natural history of hemangioblastomas of the central nervous system in patients with von Hippel—Lindau disease. Journal of Neurosurgery. 2003;98(1):82-94.
-
Bridges K, Jaboin J, Kubicky C, Than K. Stereotactic radiosurgery versus surgical resection for spinal hemangioblastoma: A systematic review. Clinical Neurology and Neurosurgery. 2017;154:59-66.
-
Vaganovs P, Bokums K, Miklaševics E, Plonis J, Zarina L, Geldners I et al. Von Hippel-Lindau Syndrome: Diagnosis and Management of Hemangioblastoma and Pheochromocytoma. Case Reports in Urology. 2013;2013:1-5.