Dural arteriovenous fistulas (dAVFs) are acquired vascular malformations in which there is a pathological connection between arterial vessels of the meninges and venous vessels of the brain or spinal cord. Dural AVFs are usually curable, but are often overlooked in standard examinations and imaging. The symptoms are often non-specific, which can delay diagnosis. It is therefore important to think of this clinical picture when complaints such as gait disturbances, headaches or neurological symptoms occur for which no cause can initially be found.
Who is affected by dural arteriovenous fistulas?
Dural arteriovenous fistulas account for about 10-15% of all arteriovenous malformations and are therefore quite rare. They occur more frequently in the 5th decade of life and are extremely rare in childhood. * *
What are the symptoms of a dural arteriovenous fistula?
Through the pathological connection of arteries and veins, the blood flows into the venous system at high arterial pressure. This leads to venous congestion and edema in the surrounding tissue, which can cause neurological deficits but also epileptic seizures.
Depending on the location of the fistula, pulse-synchronous ringing in the ears due to the perception of the flow noise or a visual impairment can occur. A dural arteriovenous fistula in the area of the spinal cord usually leads to a slowly progressing gait disorder, which can culminate in a paraplegic syndrome. High-grade dural AVFs can also hemorrhage and cause permanent neurological deficits. *
How is a dural arteriovenous fistula diagnosed?
Diagnosis of a dural arteriovenous fistula in the brain or spinal cord requires magnetic resonance imaging (MRI) as well as diagnostic subtraction angiography for selective visualization of the vessels.
What is the risk of intracerebral hemorrhage?
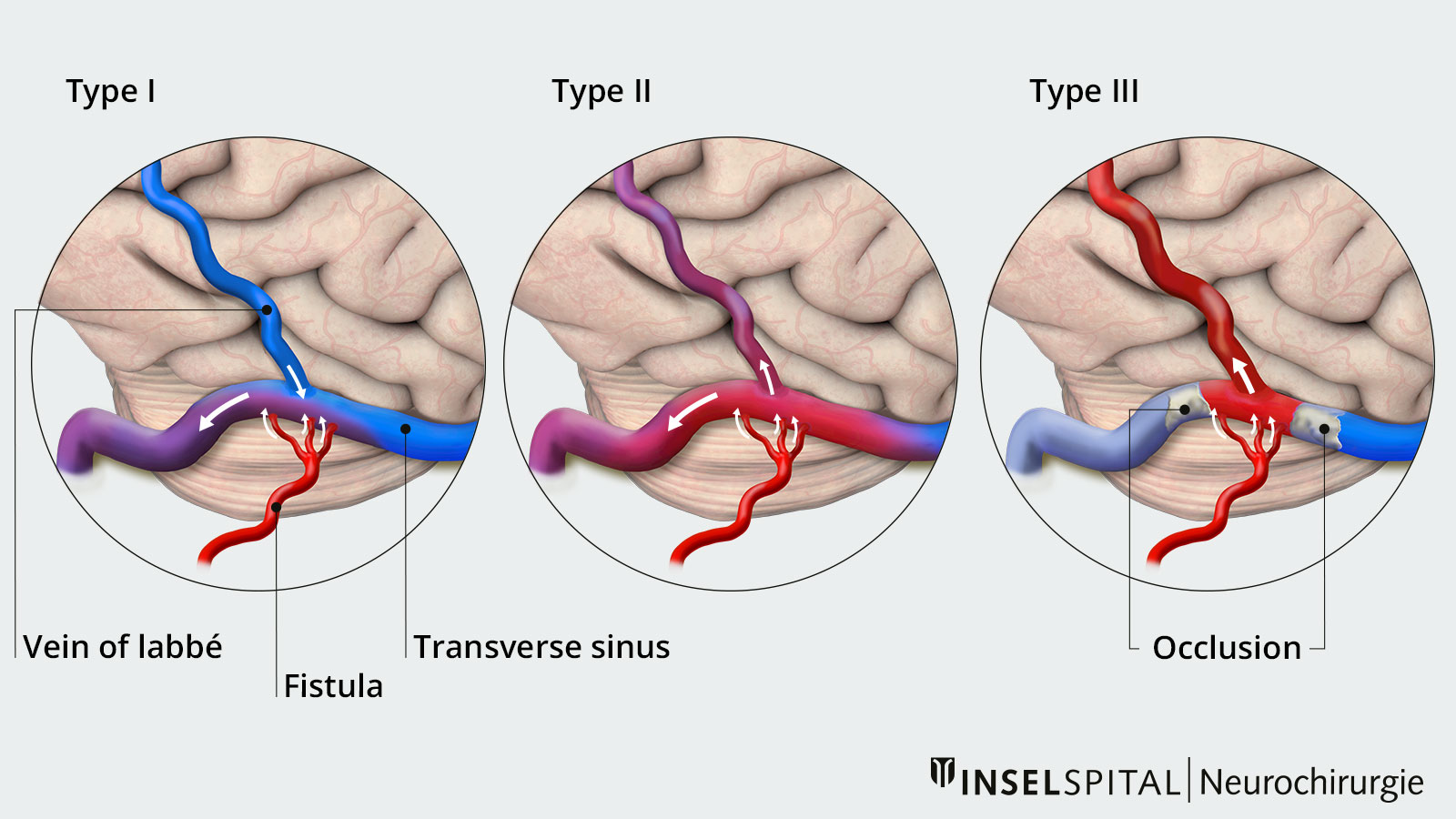
Intracranial dural arteriovenous fistulas can be divided into different groups, which also correspond to their dangerousness.
Borden type I – without cortical venous drainage
Blood from the fistula can drain freely into a large venous blood vessel. Dural ateriovenous fistulas without cortical venous drainage (Borden type I) have a very low risk of rupture of less than 0.6% per year. 13% of patients with a dAVF of Borden type ) heal spontaneaously. *
The risk of a dAVF without cortical venous drainage changing to a dAVF with cortical venous drainage is approximately 1.4% per year. *
Borden-Typ II and III – with cortical venous drainage
Blood from the fistula backs up into the brain via a venous blood vessel or a direct connection to a smaller vein.
Dural arteriovenous fistulas with cortical venous drainage (Borden type II and III) have a significantly higher risk of rupture, and in addition, increased morbidity due to neurological deficits. The annual risk of rupture is highly dependent on the type of symptoms patients have at diagnosis:
- Asymptomatic patients or patients with tinnitus or visual impairment have a rupture sirk of approx. 2% per year.
- Patients with symptoms of venous congestion have a risk of rupture of approx. 10% per year.
- Patients with cerebral hemorrhage have a risk of approx. 46% of further hemorrhage within the next year. *
What are the treatment options?
Treatment recommendations vary for dAVFs in the brain and spinal cord. Basically, the following options are available:
- a microsurgical operation
- endovascular procedure
- radiotherapy
The choice of therapy is always an individual decision and depends on the type and location of the dural arteriovenous fistula, the symptoms and the patient's previous illnesses.
Intracranial dural arteriovenous fistulas without cortical venous drainage
Patients with an incidentally discovered dural fistula without symptoms do not require therapy. However, it is important that regular imaging checks are carried out in order to detect and treat a change to a higher-grade dural arteriovenous fistula (risk approx. 1.4% per year) in good time. In patients with symptoms such as a pulse-synchronous ringing in the ears, treatment can be offered. The primary goal is to reduce flow through the fistula to relieve symptoms, not necessarily to close the fistula. Such treatment is usually endovascular. *
Intracranial dural arteriovenous fistulas with cortical venous drainage
This type of dAVF has a high risk of rupture and subsequent neurological problems. Therefore, the goal of treatment here is to repair the abnormal connection between the artery and the vein. In most cases, microsurgical disconnection of the fistula at the origin of the draining vein is the treatment of choice for this group of patients. *
Spinal dural arteriovenous fistulas
Spinal dural arteriovenous fistulas usually cause venous blood stasis in the spinal cord, which can lead to slowly progressive damage to the spinal cord with symptoms ranging from gait disturbance and weakness in the legs to paraplegia. The treatment of choice for simple fistulas is therefore disconnection by microsurgery. For more complex spinal dural fistulas, surgical and endovascular procedures are combined. In very complex and high-grade fistulas, the risk of treatment may be higher than the risks of natural history, so no therapy is recommended. * *
Why you should seek treatment at Inselspital
The examination results, treatment steps and follow-up planning for patients with dAVFs are jointly reviewed and discussed at Inselspital by a multidisciplinary team of neurosurgeons and neuroradiologists. Should surgical treatment be necessary, our state-of-the-art vascular neuronavigation system enables precise targeting to the fistula point and thus minimally invasive optimization of the procedure. The use of the latest surgical technologies such as indocyanine green angiography or electrophysiological monitoring helps us to achieve optimum surgical results for our patients.
-
Arnautovic KI, Krisht AF. Transverse-sigmoid sinus dural arteriovenous malformations. Contemp Neurosurg, 1999;21(15):1-6.
-
Gross BA, Du R. The natural history of cerebral dural arteriovenous fistulae. Neurosurgery. 2012;71:594-602; discussion 602.
-
Barrow DL, Awad IA. Spinal Vascular Malformations. The American Association of Neurological Surgeons, Park Ridge, Illinois. 1999;
-
Reynolds MR, Lanzino G, Zipfel GJ. Intracranial Dural Arteriovenous Fistulae. Stroke. 2017;48:1424-1431.
-
Spetzler RF, Detwiler PW, Riina HA, Porter RW. Modified classification of spinal cord vascular lesions. J Neurosurg. 2002;96:145-156.