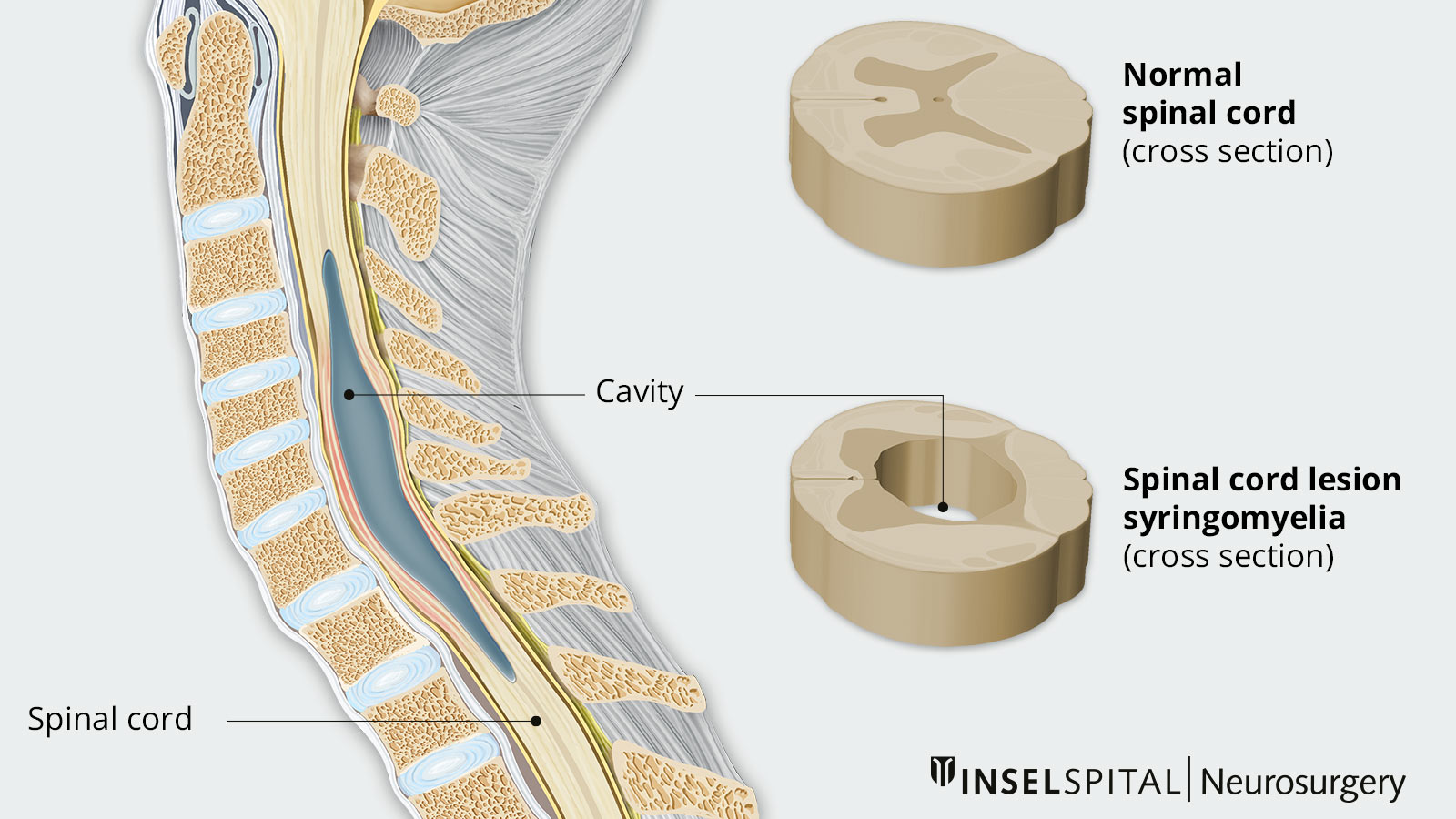
Syringomyelia or syrinx is relatively rare. It is an elongated, fluid-filled cavity in the spinal cord, which is mainly observed in the cervical spine. As it progresses, the syrinx can increase in size, length, and width and cause increasing damage to the spinal cord. Several triggering factors may be responsible. The operation of syringomyelia should be performed by an experienced neurosurgeon, as it is surgically demanding and the risk for further neurological deficits is high.
How common is syringomyelia?
Overall, syringomyelia is a very rare condition. Every year, 1–2 out of 1,000,000 people are affected – men about twice as often as women. Symptoms usually begin between the ages of 20 and 40. Although there is a familial accumulation, genetic causes have not yet been found.
What are the causes of syringomyelia?
Syringomyelia is always caused by a cerebrospinal fluid circulation disorder, i.e., an impairment of cerebrospinal fluid flow. It is assumed that a blockage of the CSF passage between the spinal cord membranes or also disturbances of the mobility of the spinal cord due to scars or other malformations are the triggering factors. As a result, cavities form in the spinal cord, predominantly in the cervical spine. The causes for the disturbed outflow can be congenital or acquired:
Congenital syringomyelia
Congenital syringomyelia is usually due to a Chiari malformation. In this developmental disorder, the cerebellum is displaced into the foramen magnum, the exit canal of the spinal cord from the base of the skull. As a result, the cerebrospinal fluid circulation in the craniocervical region is disturbed. Due to continuous transmission of the natural flow to the nerve tissue, which can no longer escape, damage occurs in the cervical region of the spinal cord. This phenomenon was called the "water hammer effect" by Gardner in 1950.
Acquired syringomyelia
Acquired or secondary syringomyelia occurs as a result of:
- Trauma. In this case, clinically progressive neurological deficits above the level of spinal cord damage become apparent several months to years after the causative trauma.
- Inflammation. Chronic inflammation can occur after meningitis, hemorrhage, or surgery within the meninges, also with arachnoiditis, an inflammation of the arachnoid membrane (arachnoid mater) surrounding the brain.
- Tumors and other constrictions in the spinal canal. Extramedullary tumors, osteophytes, or chronic large disc hernias cause compression of the CSF drainage pathways.
Differential diagnosis
A prominent central canal (canalis centralis), the so-called hydromyelia, must be distinguished from the finding of syringomyelia. The CSF flows through this canal within the spinal cord. In adults, the canalis centralis is not usually seen on magnetic resonance imaging (MRI). However, a slight widening of the canal may sometimes be seen in the image. Syringomyelia does not always have to be present as a pathologic finding. Suspicious diagnoses tend to increase due to improved MRI imaging.
What symptoms are caused by syringomyelia?
The symptoms of syringomyelia usually develop slowly and depend more on whether the cavity is in the cervical or thoracic spine and less on its size. There is no typical symptomatology. The symptoms most often correspond to those of central spinal cord injury.
- The leading symptom is a dissociated sensory disturbance. In this case, pain and temperature sensations are disturbed on one side or at least asymmetrically at the affected level of the spinal cord or are completely abolished while touch is still perceived. As a result, superficial injuries such as burns may not be noticed by the patient.
- Deep sensitivity, i.e., the perception of certain stimuli from inside the body, is also sometimes impaired.
- Furthermore, constant drilling pain may occur due to a disturbance of the sympathetic conduction.
- In addition, a lesion of the central sympathetic fibers can lead to Horner's syndrome or disorders of sweat production with absent or reduced sweat secretion.
- At the motor level, damage to motor neurons results in muscle weakness and incomplete paralysis (paresis) of the upper extremities at the level of syringomyelia. In the lower extremities, incomplete bilateral paralysis (para paresis) may occur, usually manifested only in the form of increased reflex readiness (hyperreflexia) and pathological reflexes. Spasticity or even paralysis are rarer.
- If syringomyelia also extends into the upper cervical medulla or brain stem, this is manifested by disturbances in breathing patterns (especially nocturnal apnea), eye movements (nystagmus), and lower cranial nerves (e.g., difficulty swallowing).
The symptoms of syringomyelia develop chronically and usually progress over several years. The progression may temporarily accelerate or slow down. Spontaneous regression is to be expected only in very few cases. The secondary forms of syringomyelia, especially arachnoids and tumors, show a less favorable course with gradual progression.
How is syringomyelia diagnosed?
If syringomyelia is suspected, magnetic resonance imaging (MRI) should be performed. Special MRI sequences, which can be used to visualize CSF flow, or myelography with contrast medium can be used to find and localize disturbed CSF passages. In any case, an MRI with intravenous contrast should be done to see a possible underlying tumor. Neurophysiological examinations can assess the extent of neurological damage.
What is the therapy for syringomyelia?
First and foremost, the underlying cause of syringomyelia must be treated. In the case of a Chiari malformation, decompression is obtained via bony relief and possibly dura expansion surgery (duraplasty) in the craniocervical area. The necessity of duraplasty has not been clearly established. Therefore, the individual situation should always be discussed with the patient to minimize unnecessary risk from surgery.
If the cause is a spinal tumor, it is usually located in the spinal cord. Surgical tumor removal is challenging and can lead to further neurological deficits. Therefore, an experienced neurosurgeon must decide whether surgery is advisable based on the tumor's exact location in the spinal cord and clinical symptoms. If surgery is performed, the goal is to achieve the maximum possible resection without creating new neurological deficits.
If the syringomyelia is not due to a definite cause, the spinal cord is decompressed and freed from any membranes that impede CSF flow and cause the syrinx. In order for CSF circulation to occur unimpeded, duraplasty is performed in some patients.
Before surgery, we perform an extended risk assessment on our patients. During the operation itself, the sensitive spinal cord functions are monitored with the help of our innovative intraoperative neuromonotoring (IOM). The insertion of silicone tubes and the like is now only performed in exceptional cases due to various problems.
Supportive pain therapy or physiotherapy may also be given.
Why you should seek treatment at Inselspital
When operating for syringomyelia, it is important to note that recurrences may occur depending on the underlying pathology, requiring multiple surgeries. Therefore, it is important to choose the right time for surgery. This can have a positive impact on the patient's quality of life.
The operation itself should be performed by an experienced neurosurgeon, as it is surgically demanding and the risk for further neurological deficits is high. At Inselspital, we use our innovative intraoperative neuromonitoring (IOM) for the safety of our patients during the procedure. This procedure is a focus of our clinic. We are among the leading international clinics in this field, especially in terms of technological equipment, intraoperative methods, experience based on patient numbers, and scientific publications.
-
GARDNER WJ, GOODALL RJ. The surgical treatment of Arnold-Chiari malformation in adults; an explanation of its mechanism and importance of encephalography in diagnosis. J Neurosurg. 1950;7:199-206.
-
Greitz D, Ericson K, Flodmark O. Pathogenesis and mechanics of spinal cord cysts: A new hypothesis based on magnetic resonance studies of cerebrospinal fluid dynamics. Int J Neuroradiol 1999;5:61–78.
-
Josephson A, Greitz D, Klason T, Olson L, Spenger C. A spinal thecal sac constriction model supports the theory that induced pressure gradients in the cord cause edema and cyst formation. Neurosurgery. 2001;48:636-45; discussion 645.
-
Milhorat TH, Capocelli AL, Kotzen RM, Bolognese P, Heger IM, Cottrell JE. Intramedullary pressure in syringomyelia: clinical and pathophysiological correlates of syrinx distension. Neurosurgery. 1997;41:1102-1110.
-
Rusbridge C, Greitz D, Iskandar BJ. Syringomyelia: current concepts in pathogenesis, diagnosis, and treatment. J Vet Intern Med. 2006;20:469-479.
-
Vandertop WP. Syringomyelia. Neuropediatrics. 2014;45:3-9.

