Tumors of the spinal cord grow slowly and often show few, insidiously developing symptoms until their increasing size causes severe paralysis and gait disturbances. They may grow infiltratively like astrocytoma or have a relatively clear and defined surface like ependymoma. Surgery is the treatment of choice. However, it places the highest technical demands on the neurosurgical team. Spinal cord tumors require specialized surgical and multistage simultaneous monitoring techniques. A new kind of mapping, in the development of which Inselspital was involved, can accurately determine the localization of the trajectory and thereby increase the safety of the procedure.
Which tumors occur in the spinal cord?
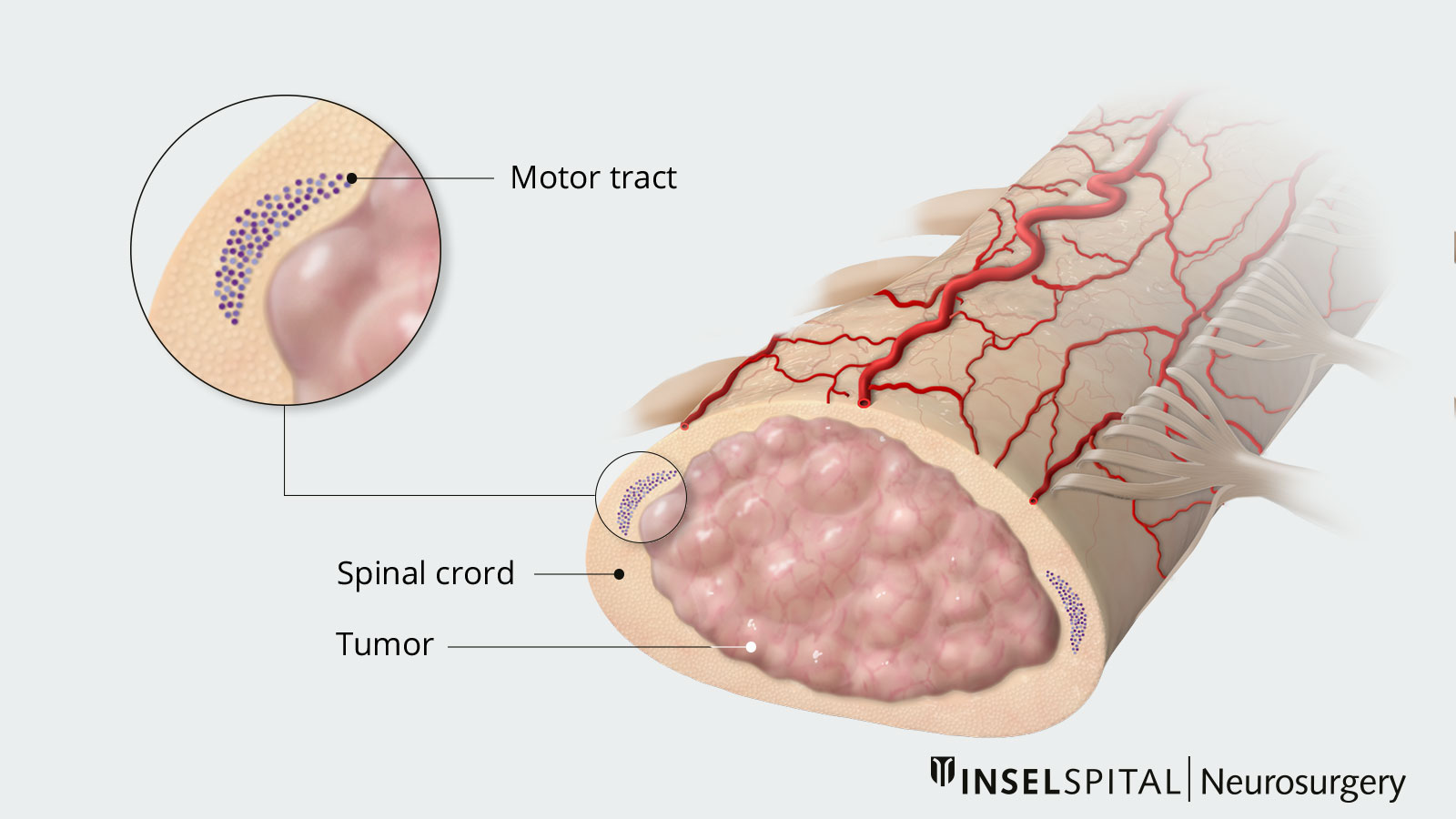
The typical spinal cord tumors are intramedullary ependymomas, astrocytomas, hemangioblastomas, or cavernomas. Intramedullary tumors are located within the spinal cord.
The most common are ependymomas, hemangioblastomas, and cavernomas with mostly smooth surfaces. They can usually – but not always – be completely removed.
Astrocytomas usually have an infiltrative growth pattern, that is, with extensions between the spinal cord tracts. Therefore, they often cannot be removed completely.
What are the risks of spinal cord tumors?
Tumors in the spinal cord grow very slowly and are often benign. However, they are located in one of the most functionally densely packed sites of the nervous system. Without treatment even benign tumors can lead to paraplegia because of the compression of the spinal cord.
In addition, spinal cord surgery is always associated with a serious risk of sensory or motor dysfunction. It is therefore necessary to evaluate the tumor carefully and find the right time for the intervention.
Main risk: paraplegia
Partial, or in the worst case, total paralysis: damage to the spinal cord resulting in paraplegia is the most serious complication following surgery on the spinal cord. Despite careful surgery, it can develop due to a circulatory disruption or mechanical stress. The risk increases with increasing size of the tumor.
Electrophysiological monitoring during the operation is therefore a must.
When should surgery be performed on a spinal cord tumor?
In the absence of symptoms and for small tumors, except for justified exceptions, a wait-and-see attitude with regular MRI follow-up is appropriate. Intramedullary tumors often grow very slowly, with long pauses, and are sometimes stable for decades.
However, if there are clear symptoms such as numbness, pain, or paralysis, surgery should be performed early because surgical outcomes are better in the early stages and with smaller tumors than with large tumors and already advanced paralysis.
Breakthrough in surgical safety
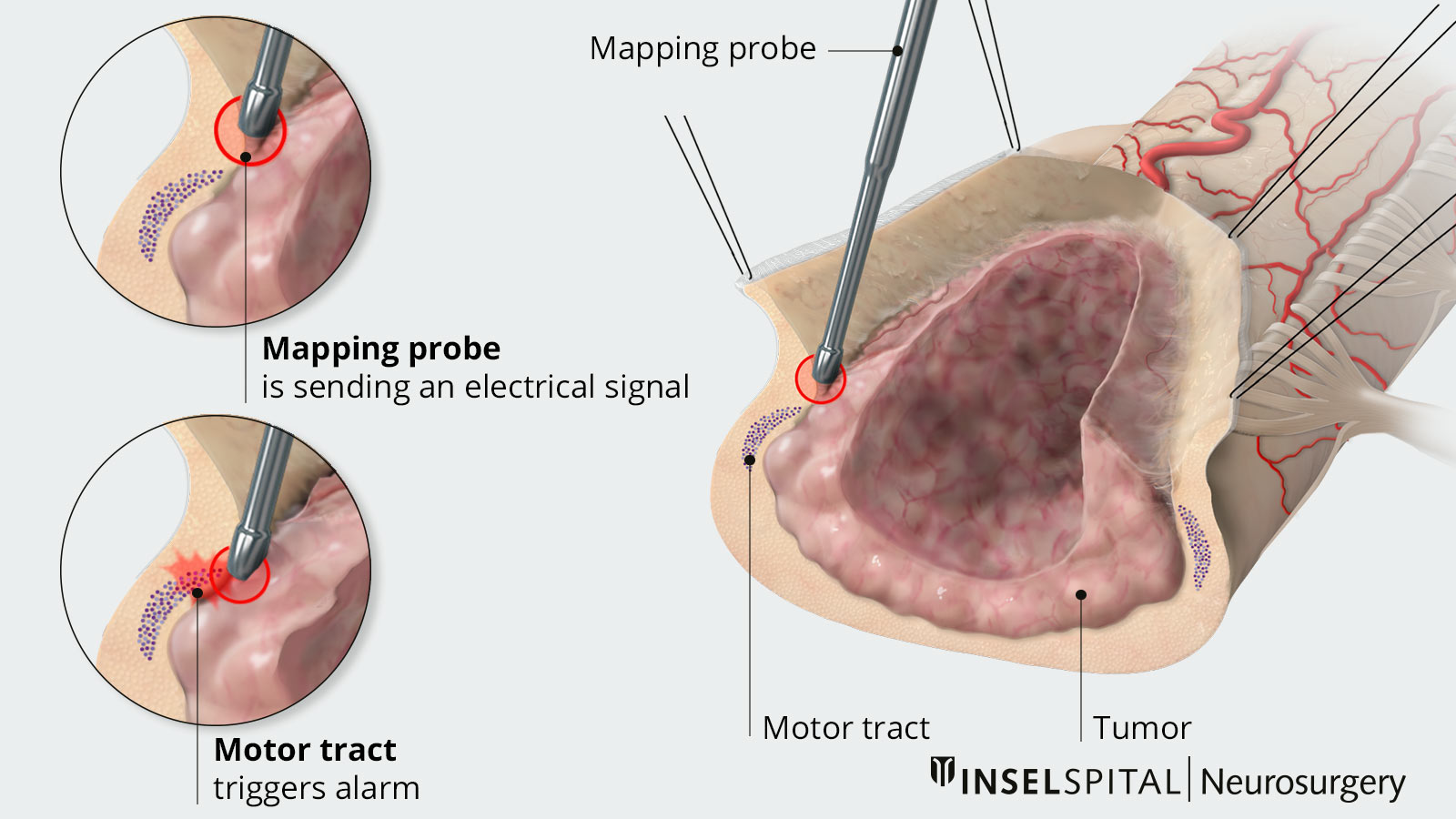
An international team, including some neurosurgeons from Inselspital Bern, was the first to develop a method for localizing important pathways in the spinal cord. This innovative procedure, which has been awarded a research prize, is now routinely used at Inselspital and increases spinal cord surgery considerably.
If the surgeon knows the exact location of the pyramidal tract, this has an influence on the surgical technique and the individual steps of tumour removal in many cases. While this so-called mapping – i.e. finding the pyramidal pathway with a pulsed microcurrent – is already established in brain surgery, this technique has not been possible on the spinal cord until now. Because the sensitive pathway and the motor pathway are interconnected via reflex neurons, the surgeon could not distinguish between the two pathways when stimulating the tissue. However, an international working group with participation of neurosurgeons from Inselspital Bern has now succeeded in making precisely this distinction: Since the motor pathway can transmit a new impulse after a short stimulus already after 60 milliseconds, but the sensitive pathway needs longer for this, the new technique of "double-training" can now selectively predict the position of the pyramidal pathway.
This new mapping is particularly important for intramedullary astrocytomas because the fibers of the trajectory are indistinguishable from the tumor. The tumor does not have a smooth boundary to the normal tissue. Intramedullary astrocytomas therefore cannot be completely removed in most cases.
Mapping can illuminate the tissue like a radar and detect the dangerous proximity of the pyramidal tract, signaling that surgery must be stopped at this point for safety reasons. For very small tumors, on the other hand, it is possible to remove them completely if the mapping indicates a sufficient safety distance.
Monitoring techniques for spinal cord tumors
Intramedullary tumors place the highest demands on surgery, especially the monitoring of spinal cord function during tumor removal. The ultimate goal of microsurgery is preservation of function with simultaneous complete removal (ependymoma, cavernoma, hemangioblastoma) or maximal reduction (astrocytoma). In addition to specialized instruments and optimized resection technique, neurophysiological monitoring is crucial. Classic neuro-monitoring is not sufficient because the motor evoked potentials are interpreted differently spinally and the sensory potentials are not meaningful for motor function.
Monitoring and mapping
Since the functional density of nerve cells and pathways is greatest in the spinal cord and brainstem, each patient must be fully informed about the possibility of additional neurological disorders. In addition to surgical experience and technique, special intraoperative spinal cord monitoring and now also mapping, which should be performed by a specialized team, help.
Motor-evoked potentials (MEPs)
The electrical stimulation of the motor center sends out impulses that propagate to the muscle via the motor pathway – the tractus corticospinalis – and are transmitted at a velocity of 60 m/s. In the muscle, the responses are derived as curves (motor-evoked potentials) and interpreted by trained personnel. They provide direct feedback on motor functions during the operation.
Somatosensory-evoked potentials (SEPs)
The activity in the dorsal column which carries the signals for sensation and the sense of orientation is measured by somatosensory-evoked potentials (SEP) during surgery. Both pathways must be spared so that the patient does not have any impairments in walking postoperatively.
Vegetative monitoring: In addition, the bulbus cavernosus reflex (BCR) is used to monitor rectal and sexual functions and now also intraoperative bladder pressure monitoring.
D-wave
The D-wave (from direct wave) is the signal directly measured at the motor pathway. Today, it is considered the "gold standard" and decisively determines the strategy of surgery and also the time of a possible termination of the procedure. As long as the D-wave is stably derivable, the patient will not have severe paralysis after surgery or will certainly recover in the course of the next few weeks. This signal has therefore a significant predictive power and has a direct influence on the technique and strategy of surgery.
Access to the tumor
Wherever possible and safe, we perform the operation through a hemilaminectomy approach. For larger exposures, we prefer the technique of laminoplasty with reinsertion of the bony vertebral arches. Both techniques preserve the spinous processes and ligaments, the so-called posterior traction ligament, which is important for the posture and stability of the spine.
Aftercare and check-ups
Surgery is always part of an interdisciplinary treatment concept. Regular follow-up examinations such as MRI scans are essential. Additional treatments such as radiation or chemotherapy can follow in case of malignant tissue diagnosis or continue the treatment in case of inoperable tumors. For most tumors, however, surgery is sufficient. Even if a small residual tumor remains, its growth is usually very gradual and the residual tumor is stable for many years or decades.
After the procedure, specialized neurorehabilitation, is very important, either on an outpatient or inpatient basis, for example in our Hospital Riggisberg. Nestled in a pre-Alpine landscape with a magnificent view of the Gantrisch chain and the high Alps, Riggisberg provides ideal conditions for a successful rehabilitation stay. An early and adequately long rehabilitation treatment can significantly reduce existing deficits.
Further reading
- Deletis V, Seidel K, Sala F, Raabe A, Chudy D, Beck J et al. Intraoperative identification of the corticospinal tract and dorsal column of the spinal cord by electrical stimulation. Journal of Neurology, Neurosurgery & Psychiatry. 2018;89(7):754-761.
- Deletis V, Seidel K. Intraoperative Neurophysiology during Surgery for Spinal Cord Tumors. Spinal Cord Tumors. Springer; 2019. p. 109-125.
- Deletis V, Shils JL, Sala F, Seidel K. Neurophysiology in Neurosurgery: A Modern Approach. 2020