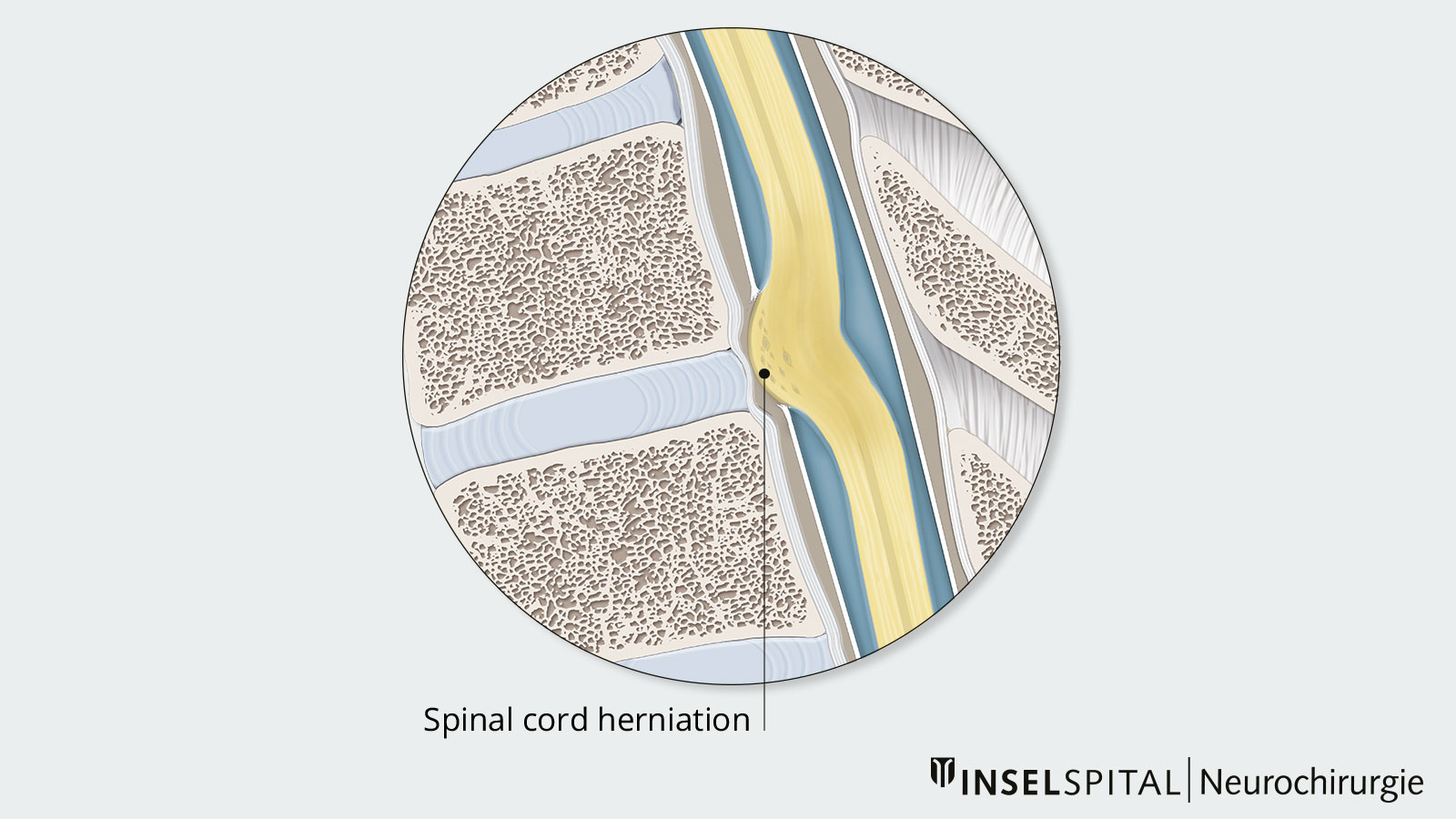
Idiopathic spinal cord herniation (ISCH) is a rare condition. Due to a dural defect, the spinal cord emerges from the nerve tube and is squeezed. The protrusion and herniation of the spinal cord causes damage to the nerve tracts. The symptoms can vary greatly: from barely noticeable to paraplegia. Often surgical relief of the entrapped spinal cord is the only therapeutic option. However, this operation is very demanding and requires not only an experienced surgeon but also intraoperative neuromonitoring to preserve spinal cord function.
How does spinal cord herniation develop?
In idiopathic spinal cord herniation (ISCH), the spinal cord protrudes outward into the epidural space through a defect in the hard meninges (dura). The herniation occurs exclusively in the anterior thoracic spine, facing the abdomen. Due to the constriction and crushing of the spinal cord in the dura, neurological damage occurs. Since the blood supply may also be impaired, vascular damage may also play a role.
Why the defect in the dura occurs and why the spinal cord bulges through is not yet known exactly. However, various triggers are discussed. These include
- a structural weakness of the dura
- mechanical pressure due to a thoracic spinal curvature (kyphosis)
- trauma
- a herniated disc.
Our experience at Inselspital shows that dural defects are located at the level of the disc space. In some cases, a herniated disc is also revealed during surgery, which is located directly in front of the dural defect and could also be a possible cause *. Constant pressure can cause the dura to perforate and the spinal cord to protrude.
This pathomechanism has similarities to that seen in spontaneous intracranial hypotension (SIH), also called cerebrospinal fluid leak). In this case, a defect in the anterior dura results in a continuous loss of cerebrospinal fluid (CSF). This defect is most commonly caused by a calcified micro spur – similar to a herniated disc. Patients complain of severe position-dependent headaches as a result of the CSF loss. The medical profession refers to this as orthostatic headache. It is not clear why some patients develop a cerebrospinal fluid leak with typical headaches and other, rare cases, develop spinal cord herniation. At Inselspital, we pay special attention to this condition.
How common is spinal cord herniation?
Spinal cord herniation is an extremely rare condition. It was first described in 1974 by Wortzman et al *. Since then, only slightly more than 100 cases have been reported worldwide.
What are the symptoms of spinal cord herniation?
Spinal cord herniation does not have specific symptoms, but it does have characteristic symptoms. Symptoms usually develop insidiously. These include:
- Sensory and gait disorders
- Muscle weakness
- Increased reflexes
- Vegetative conditions such as bladder and fecal incontinence
Typically, Brown-Séquard syndrome also occurs. This is a neurological syndrome caused by hemiplegic spinal cord damage affecting motor and sensory pathways. This is explained by the crossing of the nerve structures at the level of the spinal cord and the brain stem. On the damaged side of the spinal cord, there is a weakness of voluntary motor function and a deep and delicate sensibility. On the opposite side of the body, there are insensations to touch, temperature, and pain. This is why patients with Brown-Séquard syndrome perceive the water as differently warm on the two sides of the body when showering. The syndrome is variable and rarely occurs in its full expression.
How is spinal cord herniation diagnosed?
Spinal cord herniation and the damage it causes to the spinal cord are best visualized using magnetic resonance imaging (MRI). Spinal cord herniation must be distinguished from a dorsal arachnoid cyst. In this clinical picture, a cyst consisting of the thin meningeal layer arachnoid presses from behind against the spinal cord and displaces it forward in the direction of the spinal column. On imaging, this arachnoid cyst can easily be mistaken for spinal cord herniation. However, a definitive diagnosis is only possible during surgery.
Computed tomography (CT) complementary with contrast medium in the nerve fluid space (CT myelography) can provide additional information about constrictions in the spinal canal, such as in arachnoid cysts or an active CSF leak in spinal cord herniation.
In addition to imaging procedures, electrophysiologist examinations (sensory and motor evoked potentials) are also performed in some cases. These can be used to quantify the extent of spinal cord damage.
How is spinal cord herniation treated?
The severity of the neurological disorders determines whether and when treatment is required. If no or only very mild neurological disorders are present, progress controls at short intervals are initially sufficient.
In most cases, however, more serious neurological disorders are present. As these continue to increase over time, surgery with microsurgical repositioning of the spinal cord is necessary to prevent further progression of the disease.
As a general rule, neurological disorders that are already present will not always be reversed by surgery. Therefore, the goal of surgery is to prevent further damage and to maintain the current neurological status. For precisely this reason, surgery should be performed at an early stage. An improvement of neurological deficits may occur after surgery, but always remains to be seen.
Surgical procedure
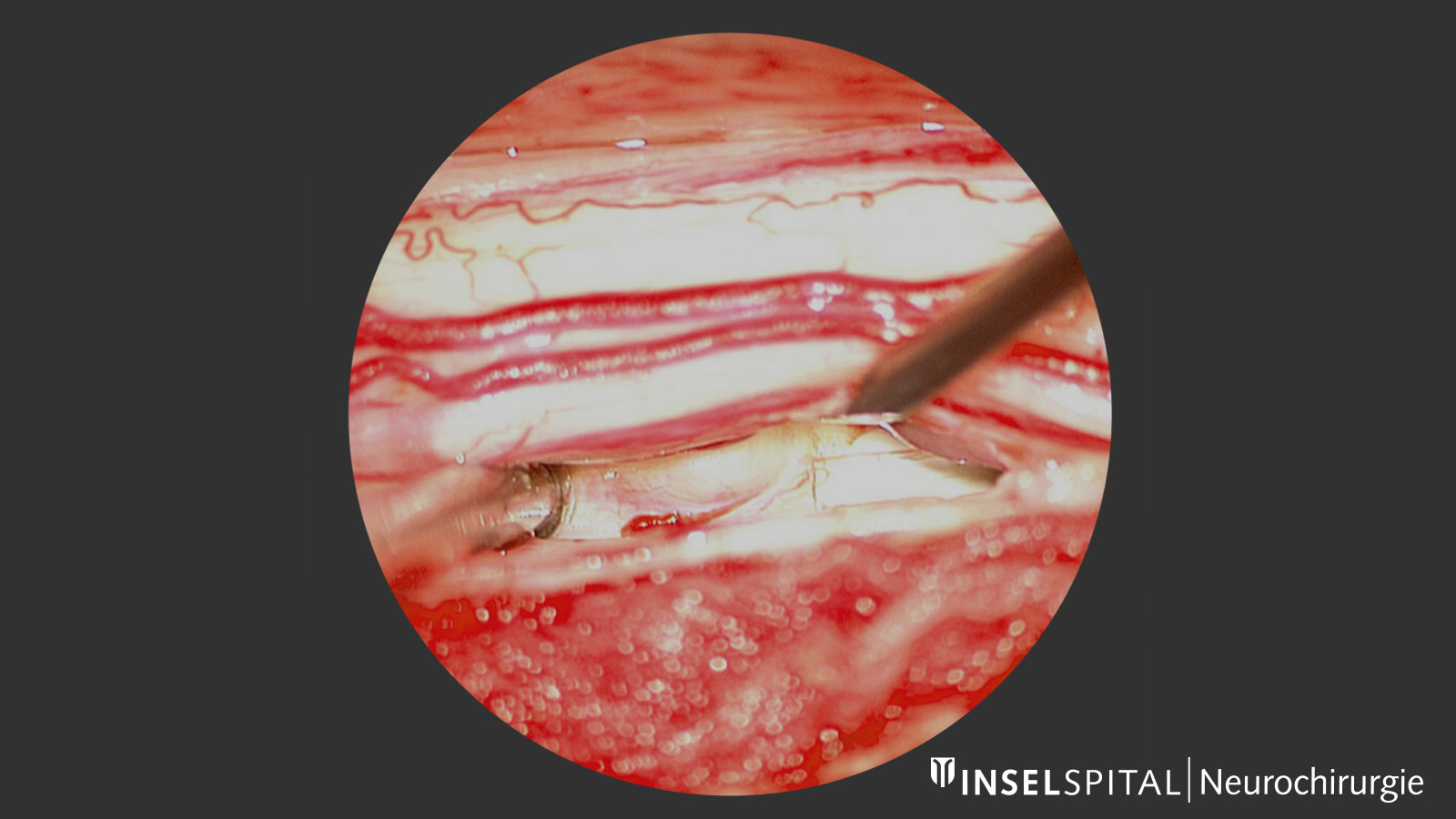
Surgery is to reposition the spinal cord to its normal position and close the defect in the dura. Surgery on the prolapsed spinal cord is challenging because it is trapped in the dura defect and may even be fused to the surrounding tissue. Additional damage can occur when the adhesions are released. Innovative safety techniques such as intraoperative neuromonitoring can be used to monitor whether damage to the spinal cord is imminent, even though the patient is under general anesthesia.
The access is chosen so that as minor tissue damage as possible is caused, but at the same time, maximum safety is ensured when operating on the spinal cord. Therefore, in almost all cases of spinal cord herniation, a complete removal of the vertebral arch (laminectomy) via a dorsal approach is necessary. An alternative is a lateral approach via the thoracic cage. The stability of the thoracic spine is not affected by either approach. Stabilization of the spine with screws is, therefore, usually not necessary.
Under the microscope, the spinal cord is released from its jammed position using microsurgical instruments. In the process, the protrusion must not simply be pulled out of the dural defect, but must be carefully excised. This allows the spinal cord to move back into its normal position. Finally, the defective area in the nerve membranes is closed with dura substitutes and sutures (duraplasty).
After the surgery
After the operation, our patients are observed overnight in the neurosurgical monitoring ward. Back on the ward, mobilization takes place on the first day after the procedure under the guidance of our physiotherapy team. There are no restrictions in the mobility or stability of the spine. After only a few days, the patient can be discharged. Depending on the severity of the neurological disorders, there is the possibility of special neurological rehabilitation or discharge home.
Why you should seek treatment at Inselspital
Spinal cord herniation is a very rare condition and a rarity even at large centers. Inselspital is one of the three largest centers in Europe for the diagnosis of spontaneous intracranial hypotension (SIH). This disorder is very similar to that of spinal cord herniation. Therefore, we can draw on a wealth of experience in diagnosis and treatment with highly standardized imaging, surgical methods and monitoring techniques.
-
Wortzman G, Tasker RR, Rewcastle NB, Richardson JC, Pearson FG. Spontaneous incarcerated herniation of the spinal cord into a vertebral body: A unique cause of paraplegia: Case report. J Neurosurg. 1974;41:631–5
-
Ulrich CT, Fung C, Piechowiak E, Gralla J, Raabe A, Beck J. Disc herniation, occult on preoperative imaging but visualized microsurgically, as the cause of idiopathic thoracic spinal cord herniation. Acta Neurochir (Wien). 2018 Mar;160(3):467-470.