Spondylolisthesis is an instability of the spine in which individual vertebrae shift forward or backward against each other. In the vast majority of cases, this occurs in the area of the lumbar spine and leads to pain and restricted mobility. If the spinal cord is compressed and the nerves damaged, neurological functional deficits can also occur.
What are the causes of spondylolisthesis?
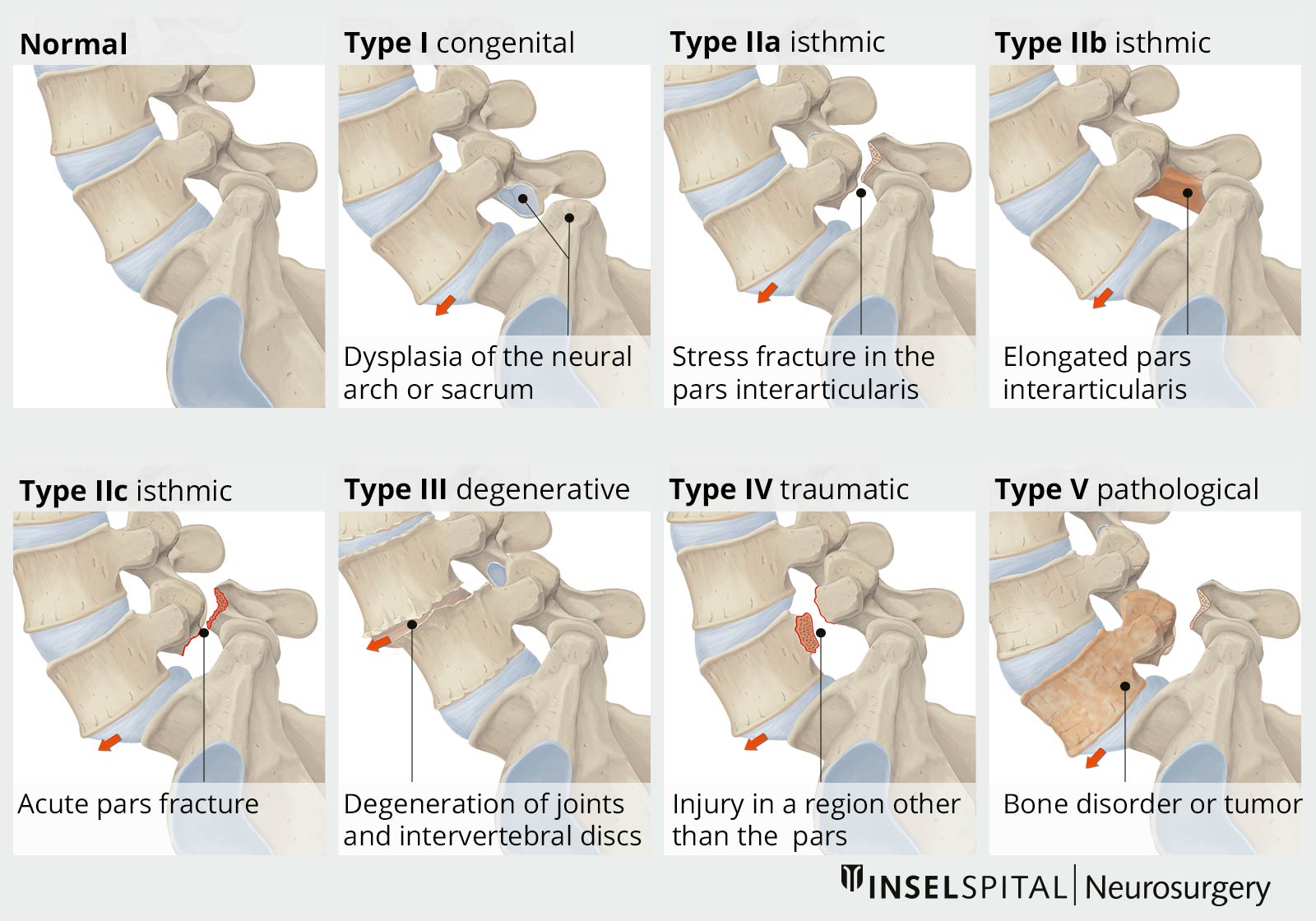
Spondylolisthesis can have very different causes, which is why different classifications exist. The most common is the classification of Wiltse * which takes both anatomical and etiological factors into account and divides spondylolisthesis into 6 categories:
- congenital
- isthmic
- degenerative
- traumatic
- pathological
- postoperative (category which was added later)
The original 5 forms (types I–V) are explained in more detail below.
Congenital type I is caused by a malformation in the region of the upper sacrum (Os sacrum) or the vertebral arch L5. Type I occurs in 94% of those affected together with other malformations such as spina bifida occulta.
Acquired spondylolisthesis (types II to V) can have various causes, such as spondylolysis (interruption of the vertebral arch), degenerative changes, trauma or pathological changes in the bone.
Wiltse type II is defined by a defect of the pars interarticularis, i.e. the area between the superior and inferior articular processes. In subtype A, a fatigue fracture of the pars interarticularis leads to spondylolisthesis. In adolescence and young adulthood, this often occurs in athletes (gymnasts or footballers), often caused by a pre-existing weakness in the pars interarticularis. The defect may also be caused by recurrent trauma. Subtype B describes a lengthening of the pars interarticularis caused by a previous fracture and subsequent healing. Subtype C is a fresh fracture.
Type III is due to degenerative changes. The lumbar vertebrae 4/5 (L4/5) are most frequently affected. Degenerative spondylolisthesis occurs more frequently in old age. It is usually a result of wear and tear on the intervertebral discs and the slackened ligamentous structures of the spinal column, which are necessary for stabilization. For this reason, degenerative spondylolisthesis usually occurs in combination with other signs of wear and tear of the spinal column, such as bulging of the intervertebral discs or wearing out of the ligaments, and then also leads to compression of the nerve fibers or the spinal cord.
Type IV of spondylolisthesis is traumatic in origin. In contrast to type II, the fracture site lies outside the pars interarticularis.
Type V occurs in connection with pathological changes in the bone. This can be the case with osteogenesis imperfecta, also known colloquially as brittle bone disease.
Spondylolisthesis of the cervical spine is much less common, and is almost never found in the thoracic spine.
What are the symptoms of spondylolisthesis?
Congenital spondylolisthesis is often an incidental finding during an imaging examination of the spine and does not always cause symptoms. Degenerative spondylolisthesis, which is caused by war and tear of the spine, is also often found incidentally in patients without complaints.
However, sliding vertebrae can also constrict and irritate individual nerve roots (radiculopathy) or compress the spinal canal and thus cause complaints. How exactly a spondylolisthesis becomes symptomatic depends on the cause and classification (see classification according to Wiltse *).
The degenerative form is often accompanied by a narrowing of the spinal canal and compression of the spinal cord. This is usually manifested by leg pain that is dependent on walking distance, known as spinal claudication.
In the congenital forms or those occurring in young adulthood, on the other hand, the patient complains of clearly defined, dermatoma-dependent leg pain in the area supplied by a nerve root. A radiculopathy is present.
In both cases, there may also be load-dependent pain in the lower back, which may be an expression of spondylolisthesis-related instability.
Neurological deficits with sensory disturbances and paralysis up to a loss of bladder and rectal continence (cauda syndrome) are fortunately rare.
How is spondylolisthesis diagnosed?
The specific anamnesis is an important part of the diagnosis and of great significance for the subsequent therapy decision. Depending on the cause of the spondylolisthesis, the patient is asked about risk factors and the exact complaints: family history, sporting activity, previous operations or accidents, type, severity and occurrence of the complaints.
During the neurological examination, attention is paid to visible step formations in the continuity of the spinal column (skew phenomenon). Malpositions such as a hollow back (hyperlordosis), a tilting of the pelvis or scoliosis, which sometimes occur in pronounced forms of spondylolisthesis, can be signs of a protective posture of the patient in order to relieve affected nerve roots. Sensitivity, motor function and reflexes of the affected extremities are checked in order to exclude damage to the nerves. Provocation tests such as a compression of the spine or raising the upper body from a stooped position by supporting it with the hands on the thighs (climbing phenomenon) serve to estimate the severity of the disease.
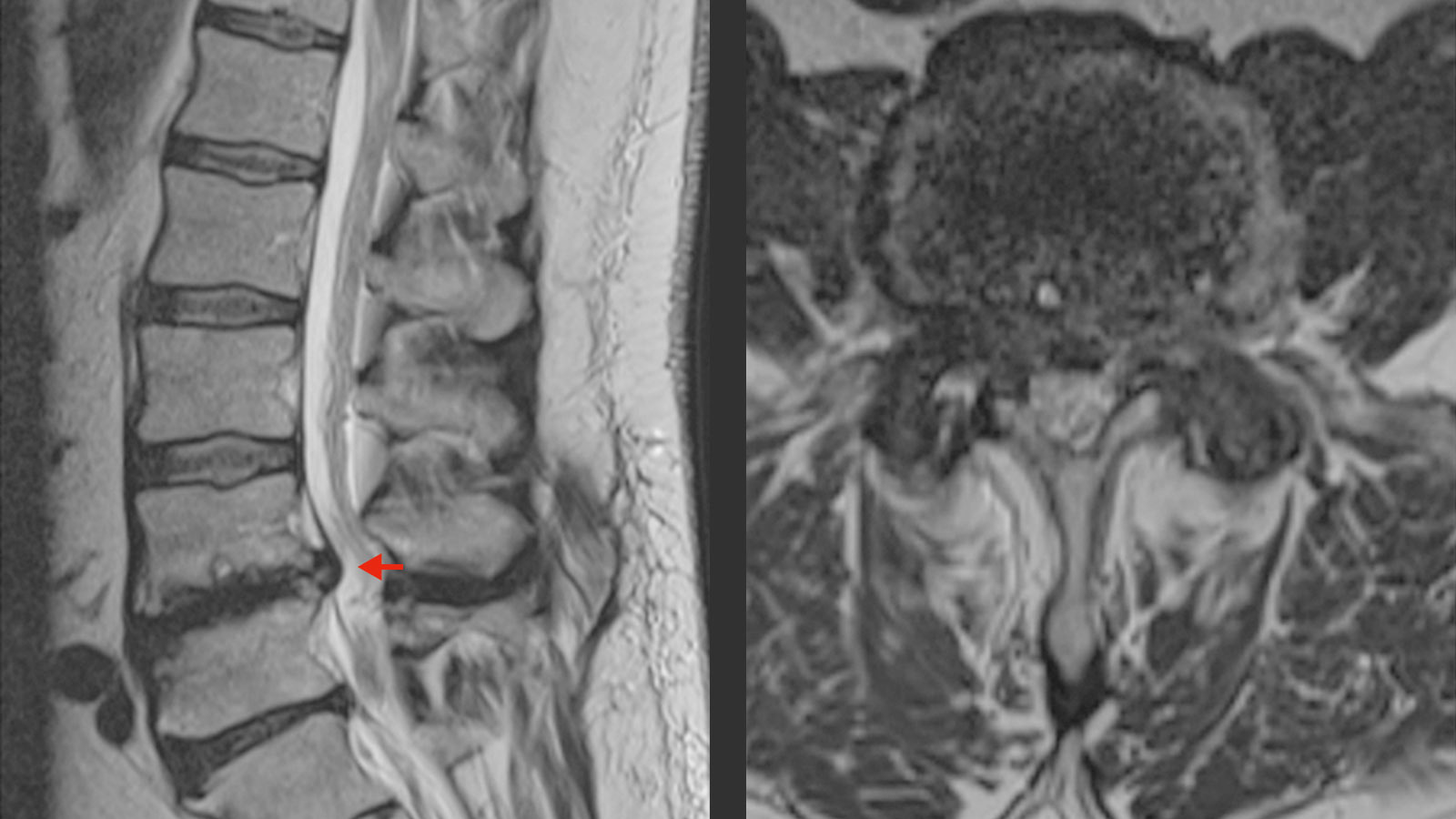
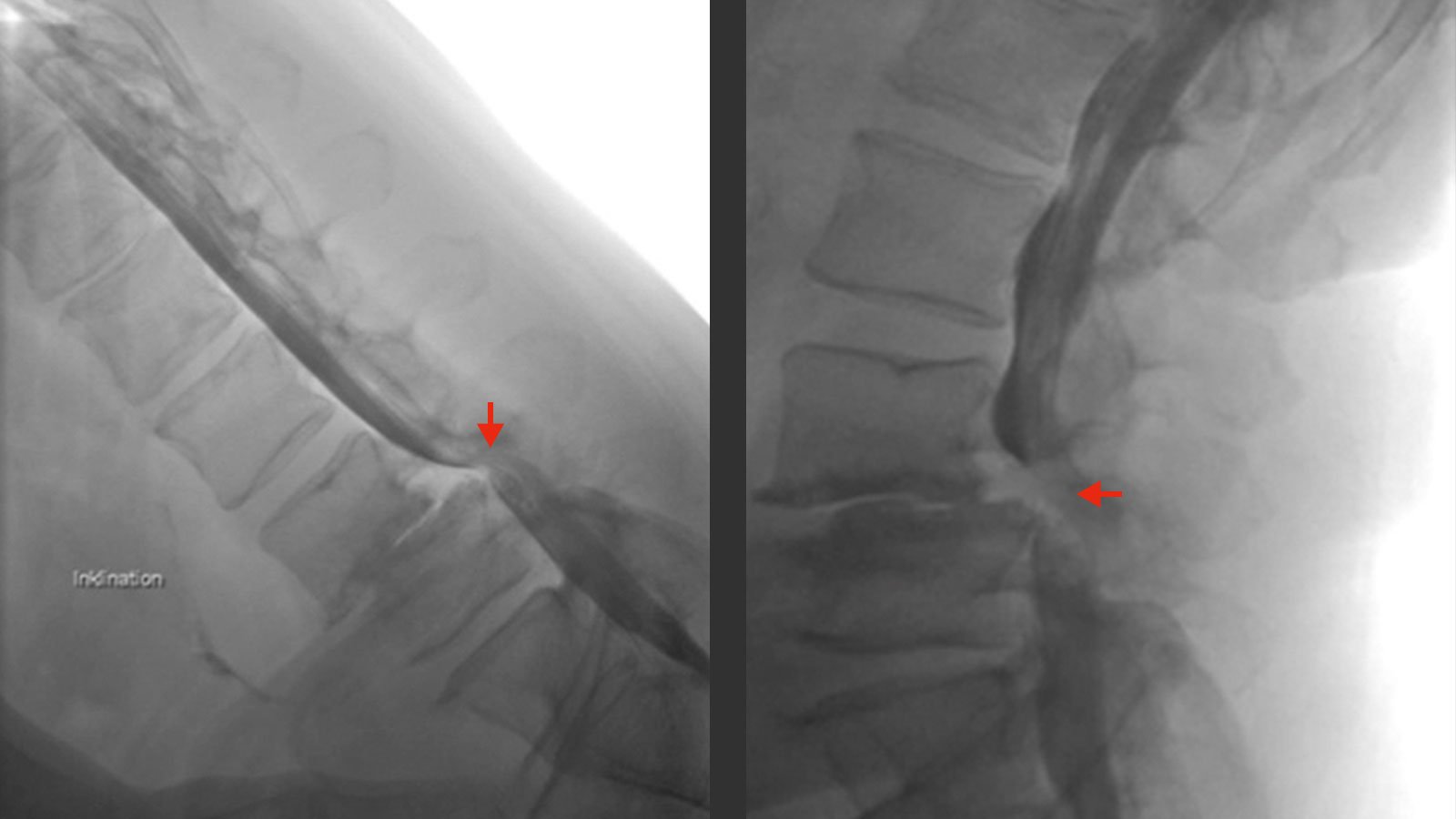
Magnetic resonance imaging (MRI) is the radiological examination of choice for the diagnosis of spinal diseases and provides detailed information on intervertebral discs, ligaments and nerve structures. In particular, MRI can show compressions by the aforementioned structures on the nerve roots very well.
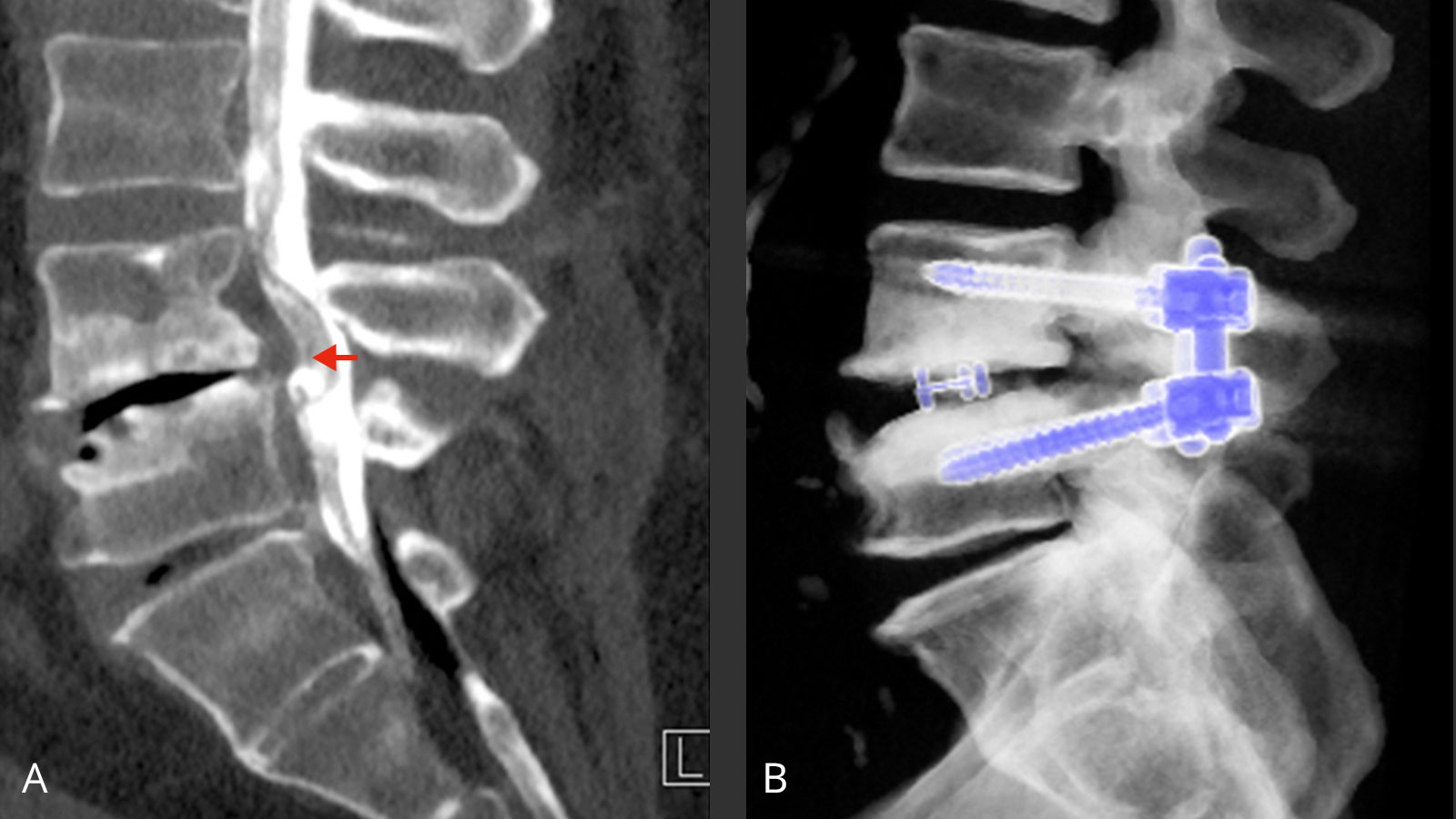
In addition, a computer tomography (CT) of the lumbar spine can be performed. It is also possible to visualize the nerve structures by injecting a contrast medium. This examination is called myelography or CT myelography. In addition, the quality of the bone and calcifications can be assessed much better in the CT than in the MRI.
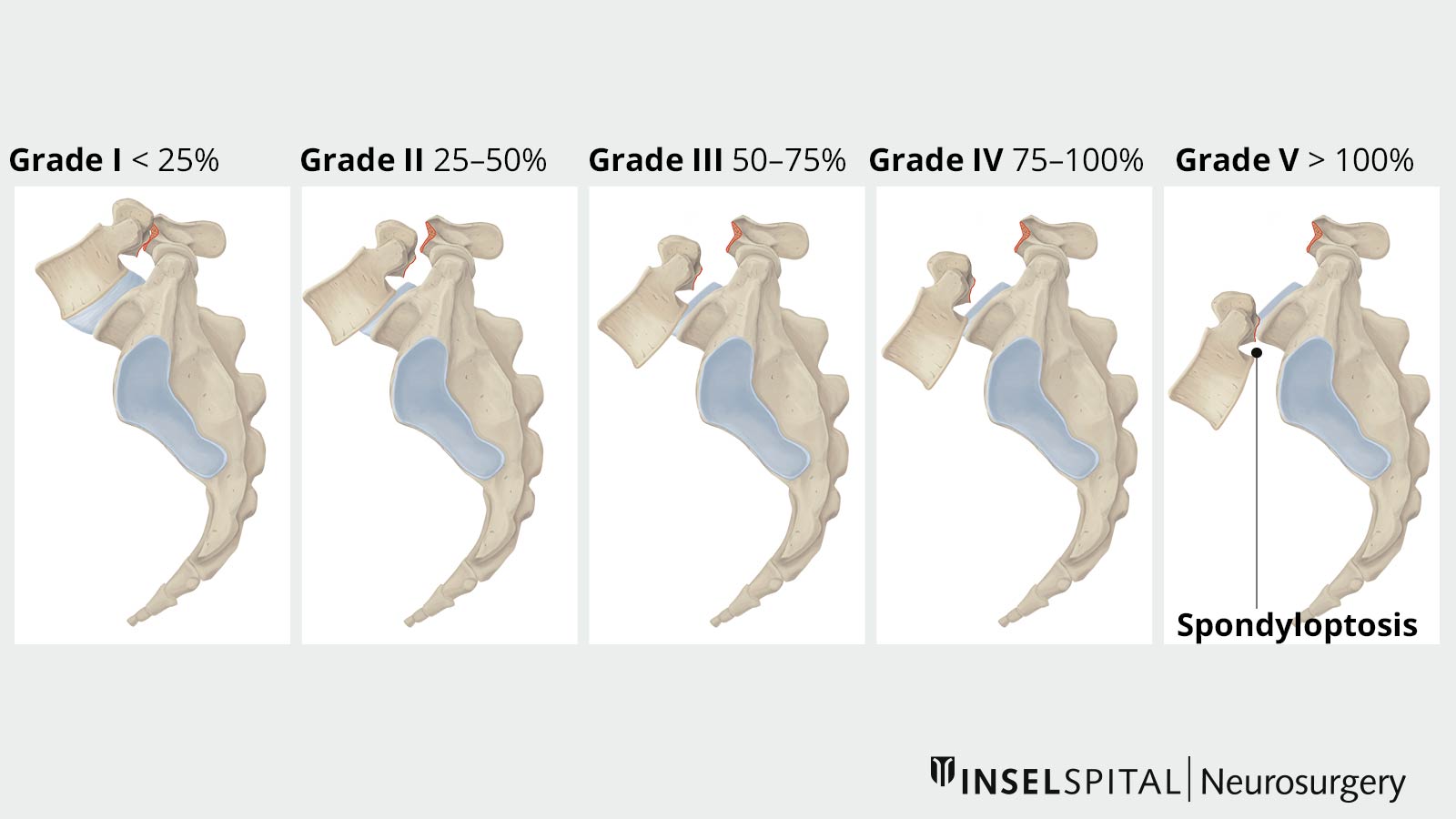
The extent of spondylolisthesis is classified according to Meyerding grading. Spondyloptosis represents the most severe form of spondylolisthesis, in which the vertebral bodies have lost contact with each other and the upper vertebra tilts forward-downward.
What are the treatment options?
The decision on the type of treatment depends largely on the causes of the spondylolisthesis.
Conservative therapy
Spondylolisthesis is primarily treated conservatively as long as there are no neurological deficits and the pain situation is under control. Conservative therapy includes painkillers and targeted physiotherapy to strengthen the back muscles and promote trunk stability. The independent continuation and regular practice of back exercises by the patients is particularly important here, because the muscular musculoskeletal system can compensate well for a possible spinal instability to a certain degree. In many cases, conservative therapy is successful in the long term.
Surgery
How spondylolisthesis becomes symptomatic depends very much on the cause. Surgical intervention is always necessary when neurological deficits are present or conservative treatment has failed. The latter becomes noticeable through increasing load- and movement-dependent back and/or leg pain. It is not uncommon for spondylolisthesis to increase in the course of the disease.
The aim of the neurosurgical intervention is to gently relieve the nerve structures. Before the operation, it must first be clarified whether the patient's complaints and the findings in the imaging match. Then the indication for surgery is critically examined by the surgeon before a surgical procedure suitable for the patient is selected. In principle, three surgical goals should be pursued for spondylolisthesis: decompression, stabilization and reduction.
Decompression of the spinal canal and nerve roots under the microscope is a standard neurosurgical procedure. It is usually sufficient in degenerative spondylolisthesis, provided that no obvious instability can be demonstrated in the X-ray and clinically.
If clinical symptoms or imaging criteria are present in degenerative spondylolisthesis that indicate greater instability, stabilizing surgery such as spondylodesis is necessary so that the spine's load-bearing capacity can be restored. In other forms of spondylolisthesis (for example, spondylolysis, trauma, postoperative), spondylodesis is usually necessary to achieve a good long-term result.
The surgical techniques for stabilization are varied and are chosen according to the pathology and the surgeon's preference. Minimally invasive techniques are usually used. In some operations, especially when the spondylolisthesis is pronounced, open techniques are preferred in order to perform a safe reduction of the vertebral bodies under visual control of the nerves.
When stabilizing the vertebral bodies, the preservation or reconstruction of the natural spinal curvatures must be taken into account. The medical profession speaks of sagittal balance. Unnatural positions of the spinal segments can otherwise lead to overstraining of the muscle and ligament apparatus and thus to incorrect loading with further degeneration and pain.
On the first day after the operation, the patient is completely mobilized with the help of our physiotherapy specialists. He is also shown movements that relieve back strain. Only a few days after the operation, during which wound healing and neurological status are checked, the patient can be discharged. Depending on the severity of the neurological disorders, a rehabilitation program may follow or the patient may be discharged home. At regular intervals, of which the patient is informed upon discharge, a clinical and imaging check-up is carried out in our consulting room in order to monitor the healing process.
Why you should seek treatment at Inselspital
At Inselspital, we have a great deal of experience in the treatment of spondylolisthesis. Thanks to the optimal networking of conservative and surgical disciplines, we are able to offer each patient a therapy that is individually tailored to their needs. In the surgical treatment of spondylolisthesis, we always choose the procedure that is the least invasive and yet guarantees satisfactory relief of symptoms. In doing so, the personal patient history as well as the individual anatomical situation must be given special consideration. We can guarantee this by discussing each case in our special consultation hours.
-
WILTSE L, MAN N, MACNAB I. Classification of Spondylolisis and Spondylolisthesis. Clinical Orthopaedics and Related Research. 11976 Jun;(117):23-9.
Further reading
The following is a list of higher-quality studies for the treatment of spondylolisthesis:
In the low-grade degenerative and isthmic form of spondylolisthesis, surgical treatment is superior after failure of conservative therapy (evidence class I).
- Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. The New England journal of medicine. May 31 2007;356(22):2257-2270.
- Ekman P, Moller H, Hedlund R. The long-term effect of posterolateral fusion in adult isthmic spondylolisthesis: a randomized controlled study. The spine journal: official journal of the North American Spine Society. Jan-Feb 2005;5(1):36-44.
Two very high-quality studies conclude that in low-grade degenerative spondylolistheses, decompression (exposure) of the nerve structures alone is often sufficient and stabilization surgery is therefore often unnecessary.
- Ghogawala Z, et. al. Laminectomy plus fusion versus laminectomy alone for lumbar spondylolisthesis. New England Journal of Medicine. 2016;374(15), 1424-1434.
- Försth P, et. al. A randomized, controlled trial of fusion surgery for lumbar spinal stenosis. New England Journal of Medicine. 2016;374(15), 1413-1423.
Numerous surgical strategies exist in the literature for spondylolisthesis, but they do not correspond to high-level evidence (class IV).