The aim of research in the field of intraoperative neuromonitoring (IONM) is to increase the safety and success of neurosurgical procedures. IONM enables continuous monitoring of important nerve functions during surgery and helps the team to react to potential hazards at an early stage. This helps to prevent damage to sensitive brain and nerve structures and to minimize the risk of permanent loss of function, which improves treatment outcomes and quality of life for patients.

Where does IONM research stand today?
Research in the field of intraoperative neuromonitoring (IONM) has made significant strides in recent years, particularly in the integration of cutting-edge technology for real-time monitoring during surgery. Advances in electrophysiology and imaging have made it possible to monitor specific neural pathways and brain areas more accurately and reliably, further improving the precision with which damage can be avoided.
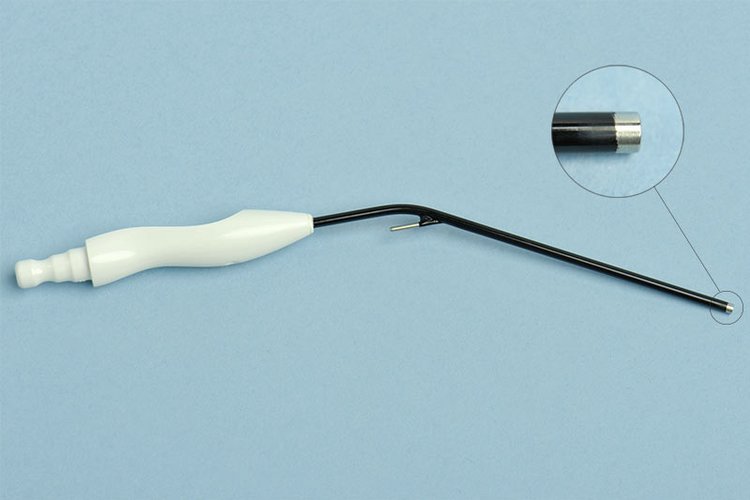
At Inselspital, continuous dynamic mapping was developed, which reduced the rate of paralysis after brain tumor surgery from about 10% with conventional mapping/monitoring procedures to 3–5%. To achieve this, we developed a hybrid instrument that enables continuous subcortical stimulation without interrupting the surgical procedure of tumor removal. In this instrument, a stimulation probe was integrated into a conventional surgical suction device.
A current focus of IONM research is also on automation and data analysis using artificial intelligence (AI), which can help doctors to interpret early warning signs more quickly.
In addition, scientists are researching multimodal monitoring methods that combine various techniques to obtain an even more comprehensive picture of neural activity and its changes. These developments help to further increase patient safety and minimize complications.
Your donation can help with
- the development and improvement of monitoring technologies: Investment in more modern devices and software for real-time monitoring of nerve function during surgery.
- automated data analysis and AI integration: Support for the development of artificial intelligence that detects changes in nerve activity at an early stage and warns surgeons in real time.
- multimodal monitoring: Funding research into combined monitoring methods that combine different techniques such as electrophysiology and imaging.
- patient safety studies: Funding clinical studies that examine the influence of improved IONM methods on patient safety and the prevention of postoperative complications.
- training and education: Providing resources for training surgeons and specialists in the use of modern IONM to achieve the best possible outcomes.
- long-term follow-up studies: Researching the long-term effects of IONM on the recovery and quality of life of patients after complex neurosurgical procedures.
Support our research for more patient safety
MEPO trial
Optimization of Transcranial Motor Evoked Potentials in Supratentorial Surgeries (MEPO)
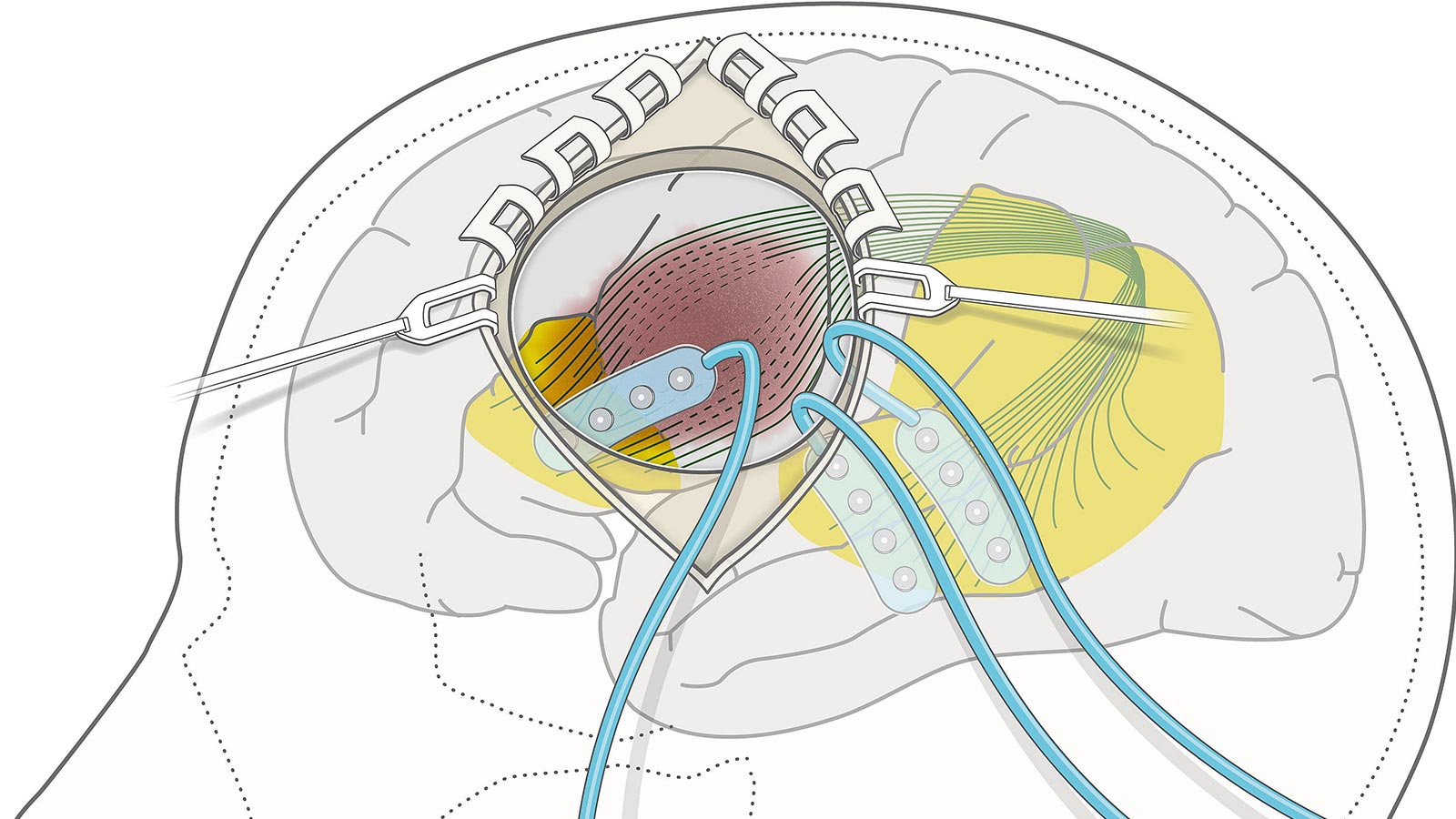
In this study, we investigate how to improve transcranial motor evoked potential (MEP) monitoring during brain surgery. While MEPs are widely used to prevent motor deficits, electrical stimulation often induces patient movement in the surgical field, which can disrupt the procedure.
Our project introduces innovative approaches to measure and reduce this movement, including intraoperative accelerometers and quantitative video analysis of surgical microscope recordings. By refining stimulation circuits, parameters, and recording montages, we aim to establish optimized techniques that minimize movement while ensuring reliable MEP acquisition. This could allow more continuous monitoring, provide earlier warnings of potential deficits, and ultimately improve surgical outcomes.
| Head of study: | Prof. Kathleen Seidel, MD |
| Study coordinator: | Pablo Abel Alvarez Abut, MD |
| Study identifier: | NCT06480370 |
CCEPs for language monitoring project
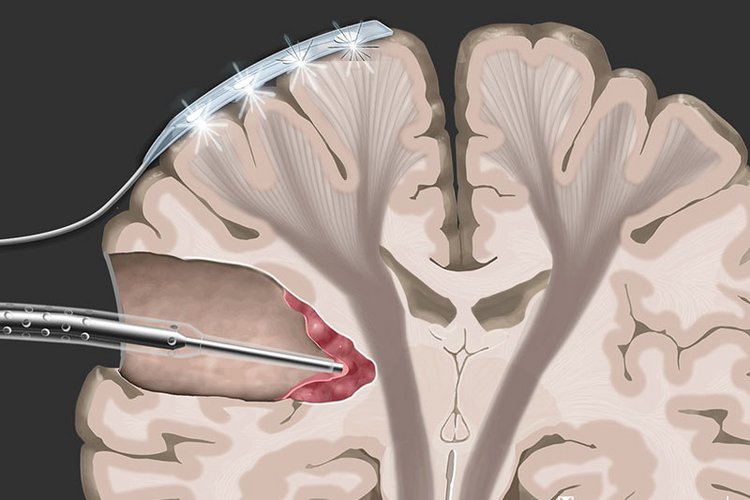
Research in cortico-cortical evoked potentials (CCEPs) aims to enhance the mapping and preservation of critical language pathways during tumor surgeries near language-related brain regions. CCEPs enable direct measurement of functional connectivity between cortical areas, providing insight into individual variations in language networks. By refining CCEP techniques, we seek to improve intraoperative identification of language areas, reduce the risk of postoperative language deficits, and support safer resections in eloquent brain regions.
Publication on this research project:
Seidel K, Wermelinger J, Alvarez-Abut P, Deletis V, Raabe A, Zhang D, Schucht P. Cortico-cortical evoked potentials of language tracts in minimally invasive glioma surgery guided by Penfield stimulation. Clin Neurophysiol. 2024 May;161:256-267. doi: 10.1016/j.clinph.2023.12.136.
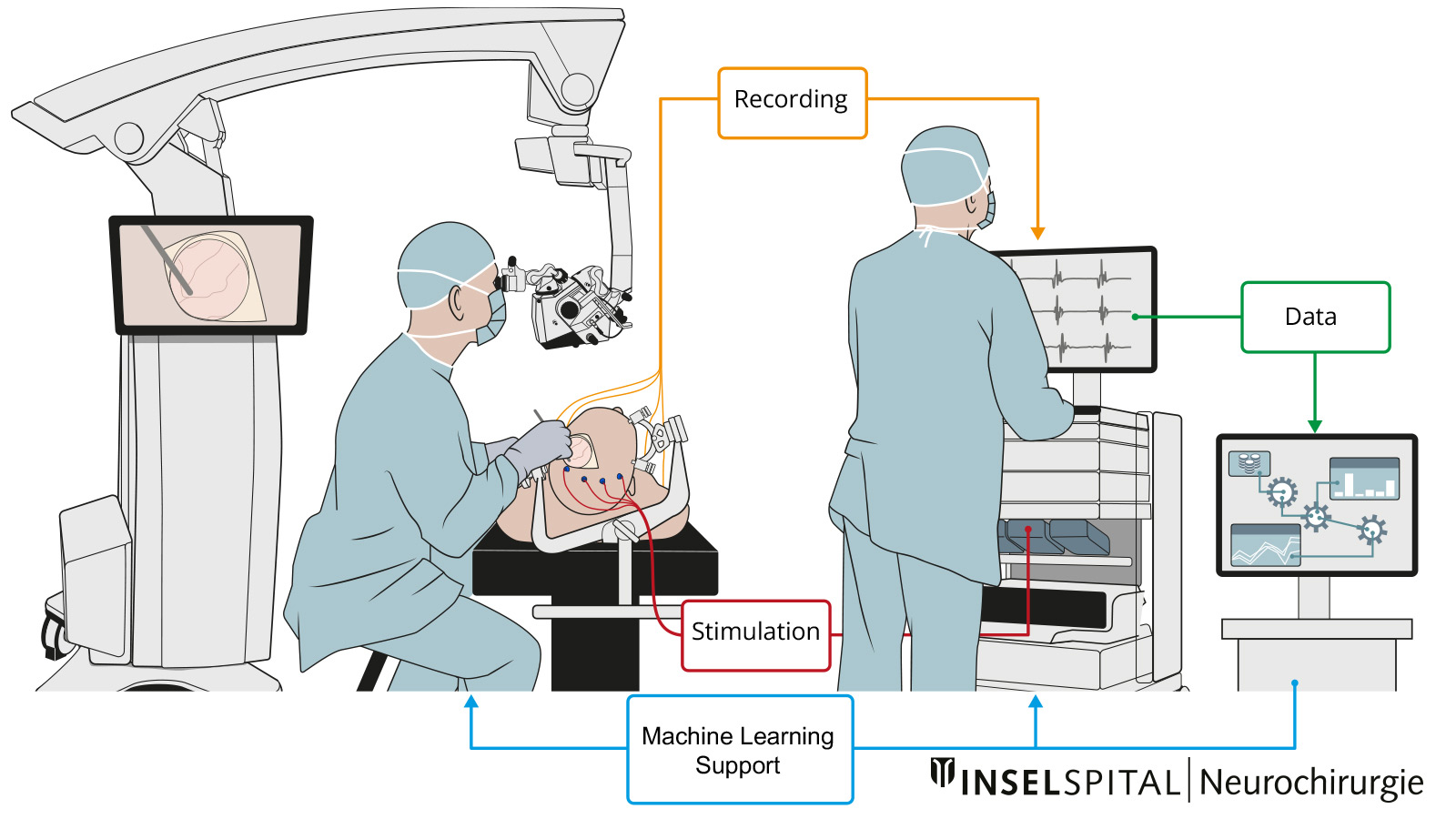
Project Machine Learning in IOM
In this research project, we apply machine learning to intraoperative neurophysiological monitoring (IOM) to improve patient safety and surgical outcomes.
During surgery, IOM tracks the functional integrity of neural pathways in real time; however, interpreting complex signals quickly can be challenging and prone to human variability.
Machine learning has the potential to assist by detecting subtle changes, reducing false alarms, and predicting adverse events earlier than conventional methods. This approach could enhance decision-making for the surgical team, support consistent signal interpretation, and ultimately reduce the risk of neurological injury.
Publications on this research project:
Wermelinger J, Parduzi Q, Sariyar M, Raabe A, Schneider UC, Seidel K. Opportunities and challenges of supervised machine learning for the classification of motor evoked potentials according to muscles. BMC Med Inform Decis Mak. 2023 Oct 2;23(1):198. doi: 10.1186/s12911-023-02276-3.
Parduzi Q, Wermelinger J, Koller SD, Sariyar M, Schneider U, Raabe A, Seidel K. Explainable AI for Intraoperative Motor-Evoked Potential Muscle Classification in Neurosurgery: Bicentric Retrospective Study. J Med Internet Res. 2025 Mar 24;27:e63937. doi: 10.2196/63937.