Epileptic seizures are one of the most common neurological conditions. The list of possible causes is long and includes strokes, brain injuries, brain tumors or neurodegenerative diseases such as Alzheimer's dementia. However, not all patients who experience a single seizure will actually develop epilepsy. Epilepsy is defined as multiple spontaneous seizures that are not related to a temporary health condition, as is the case with fever, alcohol withdrawal, or low blood sugar level.
How common is epilepsy?
Epilepsy is a chronic disease. In Switzerland, an estimated 1% of the population is affected, which corresponds to around 100,000 people. For those affected, there are enormous consequences for their entire living environment - private, family, professional and social. For this reason, it is very important for epilepsy patients to consult a specialized center that can carry out the correct medical assessments and offer appropriate therapies.
What are the different types of epileptic seizures?
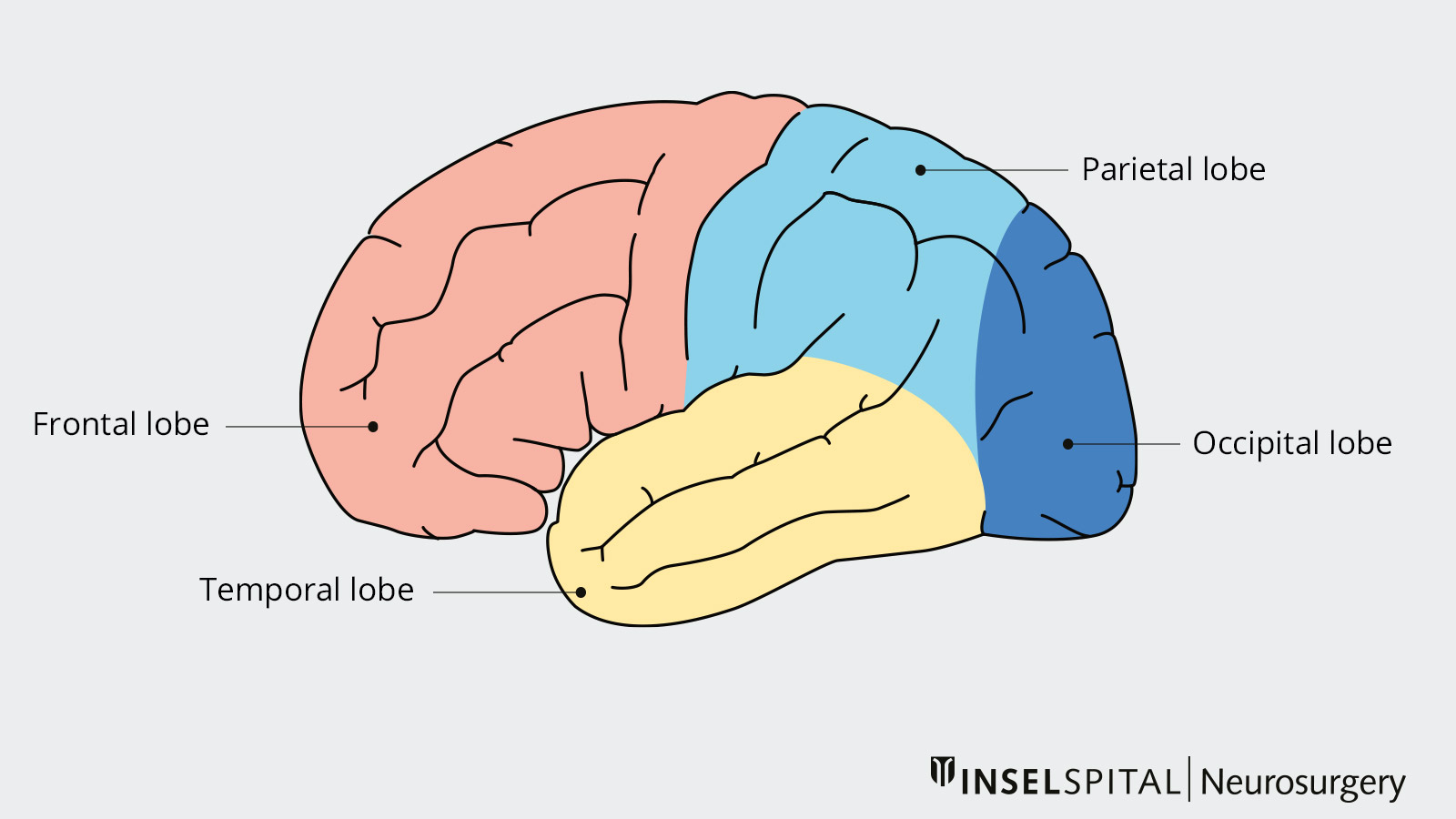
An epileptic seizure is the result of a temporary disturbance in electrical signal transmission between nerve cells. This results in a rhythmic overactivity of many nerve cells involved. Nerve cells from different regions of the brain can be affected. Accordingly, the appearance of seizures can vary greatly depending on which brain region is affected by the epileptic activity.
In general, a distinction is made between:
- Simple focal seizures: the affected person is conscious, jerking or tingling sensations occur in a certain part of the body
- Focal complex seizures: similar to a focal seizure, only with a brief loss of consciousness
- Generalized seizures: generally occur with loss of consciousness, possibly with tonic-clonic motor spasms (grand mal) or without motor manifestations (petit mal).
What is pharmacoresistant epilepsy?
50–60% of all forms of epilepsy have a focal onset. This means that the epilepsy is triggered in a specific brain region and spreads from there to neighboring brain regions. This trigger zone, the so-called seizure onset zone, may be associated with a brain lesion (tumor, malformation, nerve tissue scar), but may also look inconspicuous. 20–30% of all patients with focal epilepsy continue to have epileptic seizures despite multiple attempts at drug therapy. In such cases, one speaks of pharmacoresistant epilepsy. Patients with focal and/or pharmacoresistant epilepsy are candidates for epilepsy surgery.
When is epilepsy surgery indicated?
The goal of epilepsy surgery is to cure epilepsy. This can be achieved in approx. 80% of cases if the lesion can be removed without damaging important neighboring brain areas that are responsible for speech, vision or motor function. Therefore, a detailed pre-surgical evaluation at a specialized center is particularly important. Here, all questions can be answered and the success of the treatment as well as the therapy risks can be precisely assessed. The necessary examinations before surgery include long-term video EEG monitoring (telemetry). The EEG electrodes can be attached to the surface of the scalp or, in the case of specific issues, temporarily implanted on the surface of the brain or at certain locations in the depth of the brain. The aim of this long-term EEG monitoring is to identify the seizure onset zone unequivocally.
What are the types of epilepsy surgery?
There are various surgical procedures for the treatment of the different forms of epilepsy. These include both curative procedures (with the aim of curing the epilepsy) and non-curative procedures (with the aim of reducing the frequency of seizures). In the following, we briefly discuss the different procedures offered at Inselspital.
Curative procedures
A surgical procedure that precisely removes the brain tissue from which the epileptic seizures originate is called resection. The goal is the complete resection of this epileptogenic focus. Resective procedures are the most commonly used procedures in epilepsy surgery and have the best success rates. Resective procedures include:
Lesionectomy
The surgical removal of a lesion that triggers the epileptic seizures is called a lesionectomy. Lesions are well-defined structural abnormalities in the brain. These include, for example, tumors, vascular malformations such as cavernomas, or defined brain abnormalities such as focal cortical dysplasia. During surgery, the lesion itself and the surrounding brain tissue are removed. Success rates are very high, with approximately 80% freedom from seizures. Most patients are subsequently able to discontinue their antiepileptic medication.
Amygdalohippocampectomy and partial temporal lobe resection
If the epileptogenic focus is located within certain anatomical structures in the temporal lobe, more precisely in the amygdala or in the hippocampus, these temporal structures as well as the surrounding parts of the cerebrum can be removed without causing relevant disturbances to the affected patients. This however requires a good pre-surgical evaluation. The surgical results are very good and 70–80% of patients are seizure-free after surgery, with about half of these patients being able to discontinue their antiepileptic medication.
Partial lobectomy
If the epileptogenic focus is located in the frontal lobe, parietal lobe, or occipital lobe, these parts of the brain can be partially removed. In most cases, this type of surgery is used when there is a lesion or structural abnormality within these parts of the brain. The success rate of partial lobectomy is approximately 50–60%.
Functional hemispherectomy
This form of epilepsy surgery is used almost exclusively when the epileptic activity originates predominantly of one hemisphere of the brain. The epileptogenic focus, which in these cases affects only one hemisphere of the brain, is very extensive and cannot be completely removed. This usually affects children with a large vascular malformation, perinatal cerebral hemorrhage or infarcts as well as patients with Rasmussen's encephalitis. During the operation, all fiber bundles are separated, through which the two brain hemispheres communicate with each other.
The goal of surgery is to prevent seizure spread to the healthy, unaffected half of the brain. The diseased, epileptogenic hemisphere is usually without residual function due to the underlying disease. The chances of success of this operation are also very good. More than 80% of the patients usually have a significantly reduced frequency of seizures, and many are even completely free of seizures. The prognosis is slightly worse for diseases that progress, such as Rasmussen's encephalitis.
Laser Interstitial Thermal Therapy
Laser Interstitial Thermal Therapy (LITT) is a laser ablation. This type of therapy is based on the principle of heating and obliterating diseased brain tissue using laser technology. During treatment, magnetic resonance imaging (MRI) of the head is performed in order to precisely visualize the area of the brain that is to be obliterated by LITT. The laser is introduced into the lesion or the affected area using a high-precision process called stereotaxy. The entire procedure is performed in a minimally invasive manner without having to open the skull bone extensively.
This minimally invasive procedure is suitable for the treatment of minor, narrowly defined epileptogenic zones. The advantages of this method compared to the classic resective procedures are:
- Shorter treatment duration
- Less stressful, since no large opening of the skull bone (craniotomy) is necessary
- Fewer complications (infections, wound healing disorders)
- Shorter hospital stay
Initial data from this relatively new form of treatment show a success rate of approximately 50% seizure freedom for selected indications. LITT is subject to further research and clinical evaluation.
Non-curative procedures
For certain forms of epilepsy, a resection cannot be performed because the expected treatment success is too low or the surgical risks associated with resection are too great. In these cases, the following non-curative procedures are available:
Neuromodulation
Surgical procedures that modulate or reduce the electrical activity of the epileptogenic focus or the affected neuronal network rather than resecting the epileptogenic focus are called neuromodulation. In this procedure, delicate electrodes are implanted in a high-precision technique at the site of stimulation and connected to a pacemaker (implantable pulse generator). There are currently two neuromodulative procedures for epilepsy:
Vagus nerve stimulation
Vagus nerve stimulation (VNS) is an approved treatment for focal epilepsy when resective procedures are not applicable. In this procedure, a small pacemaker is implanted under the collarbone and connected to an electrode that is attached to the vagus nerve using a microsurgical procedure. The pacemaker generates small electrical pulses that stimulate the vagus nerve. Over the long term, this reduces the frequency of epileptic seizures in patients treated in this way. The procedure reduces the frequency of seizures by about 50% in about half of the patients.
Deep brain stimulation
Deep brain stimulation (DBS) is the second treatment alternative. Here, two electrodes are implanted to a specific nucleus structure in the brain, the anterior thalamus, via a high-precision procedure (stereotaxy). The pacemaker is implanted under the collarbone and connected to the electrodes via an adapter cable that runs under the skin. The pacemaker generates small electrical pulses that stimulate the thalamus and inhibit the spread of epileptic activity. This procedure also reduces seizure frequency by about 50% in about half of the patients.
Why you should seek treatment at Inselspital
Inselspital is one of the three Swiss centers with the highest number of cases. We therefore have the necessary experience and expertise to diagnose epilepsy patients precisely and to treat them in a targeted and holistic manner according to the latest research.
The Seizure Unit of the Department of Neurology at Inselspital started operations at the beginning of 2024. The state-of-the-art monitoring unit for epilepsy patients has four beds in the new Anna Seiler Building. Thanks to a nearby control room with numerous monitors, the unit enables an even faster response time in the event of epileptic seizures. This provides valuable information for highly specialized epilepsy diagnostics and treatment.
A clinically approved ultra-high-field MRI scanner is available for epilepsy assessments. The Inselspital is thus a pioneer in Switzerland with regard to epilepsy diagnostics.
