Tarlov cysts, also known as perineural cysts, are fluid-filled protrusions of the nerve root sheaths that usually occur in the area of the sacral spine. They are asymptomatic in many cases, but can also cause pain in the back, buttocks and legs, as well as neurological deficits. The exact cause of their development is not fully understood. Treatment varies from conservative measures such as pain medication and physiotherapy to surgical intervention for severe symptoms.
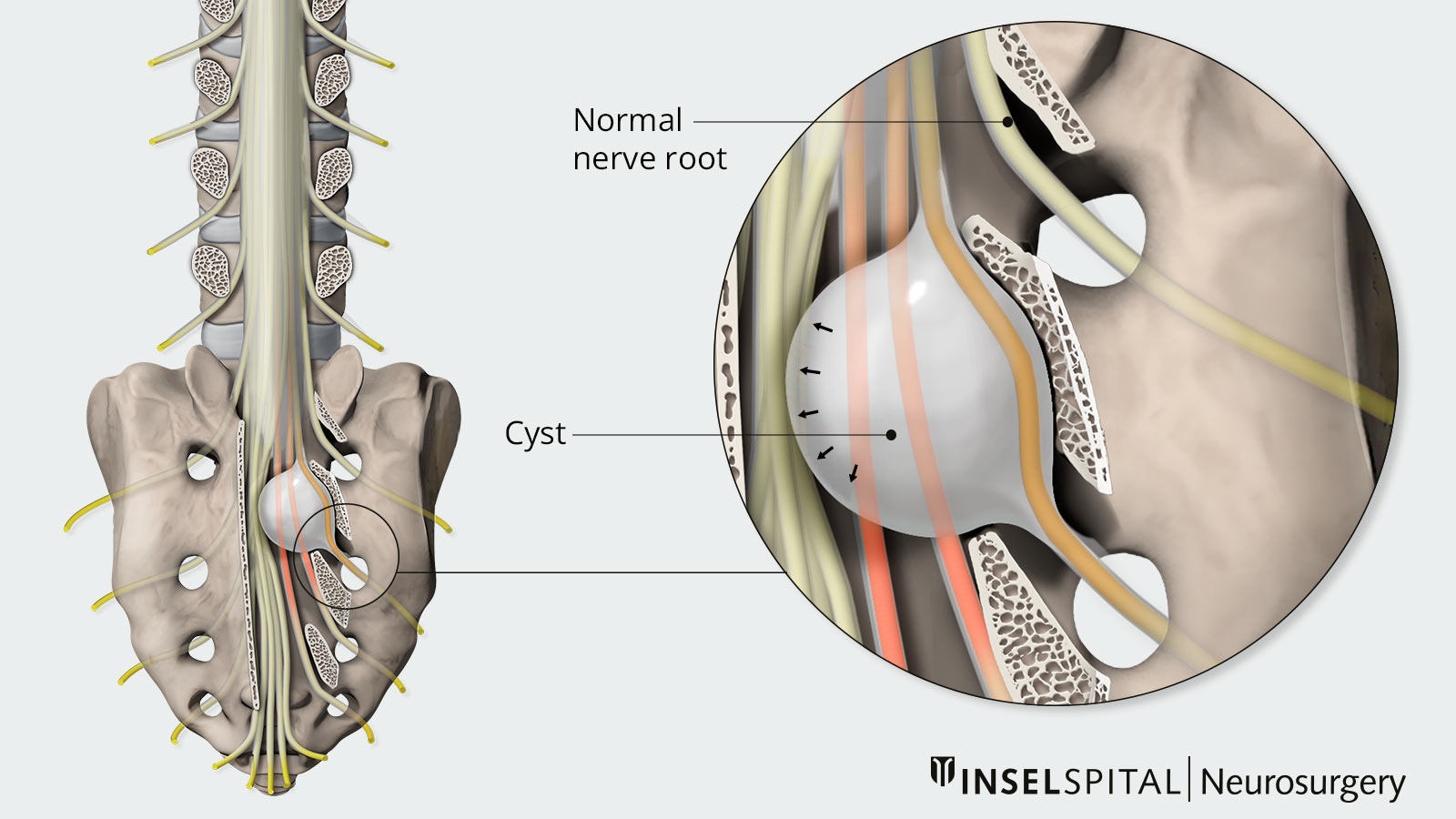
Tarlov cysts most commonly occur in the sacral area and typically affect the sacral nerve roots S2 or S3 *. In principle, however, they can occur anywhere along the spine. *, *
They develop when fluid leaks into the space between the perineurium (which surrounds individual nerve fiber bundles) and the epineurium (which surrounds the entire nerve) *. Usually there is a small connection to the cerebral spinal fluid space, which can cause nerve roots to be compressed *, *. In contrast to other meningeal cysts, Tarlov cysts take longer to fill with contrast agent during myelography, an imaging technique used to visualize the cerebrospinal fluid space, and do not collapse immediately during CSF drainage. *, *, *
How are Tarlov cysts classified?
Classically, cysts associated with the meninges of the spinal column are categorized into three types *:
- Type I: extradural (outside the original meninges) meningeal cysts without nerve fibers
- Type II: extradural meningeal cysts with nerve fibers
- Type III: intradural meningeal cysts
The classic Tarlov cysts are type II cysts according to Nabors et al. *
How common is a Tarlov cyst?
Depending on the imaging technique and analysis used, a Tarlov cyst can be found in approximately 1–13% of all individuals and is an incidental finding in the vast majority of cases *, *, *, *. Women are affected more often than men *, *. This high number makes it clear that only a very small proportion of the cysts actually cause symptoms, which often makes diagnosis difficult.
What is the cause of a Tarlov cyst?
The exact cause of Tarlov cysts is still unclear. It is assumed that factors such as inflammation, injury, degenerative changes or a genetic predisposition can contribute to the formation of these cysts. The most common hypotheses include an inherited risk, an enlargement of the soft meninges with subsequent encapsulation or increased pressure in the cerebral fluid space due to connective tissue weakness *.
What symptoms does a Tarlov cyst cause?
Most Tarlov cysts do not cause any symptoms *. Only a small percentage of them lead to symptoms, usually when they grow due to the pressure of the cerebral fluid *, *, *, *, *. This can cause the cysts to stretch nerve fibers or press against surrounding bone *, *. Depending on their location, various symptoms of nerve compression *, *, * may occur, such as:
- pain radiating along the nerve roots, similar to sciatica
- problems with the bladder or bowel
- localized low back pain, especially with larger cysts *, *, *, *
In rare cases, Tarlov cysts have also been associated with sexual dysfunction, but this has not been sufficiently studied *, *, *. Most commonly, pain radiates to the thigh, the area around the anus or the perineum and can be aggravated by standing, coughing or pressing *. Large cysts also exert pressure on the periosteum of the sacrum, causing local pain.
Even relatively small cysts can cause symptoms. In addition, problems such as bladder, bowel or sexual dysfunction are often not addressed or asked about during the doctor's appointment. As a result, Tarlov cysts are often considered an incidental finding and left untreated, which can lead to long-term psychological strain for those affected. In addition, incorrect or inadequate treatment can lead to recurring symptoms, lasting discomfort and frustration for the treating physicians. *
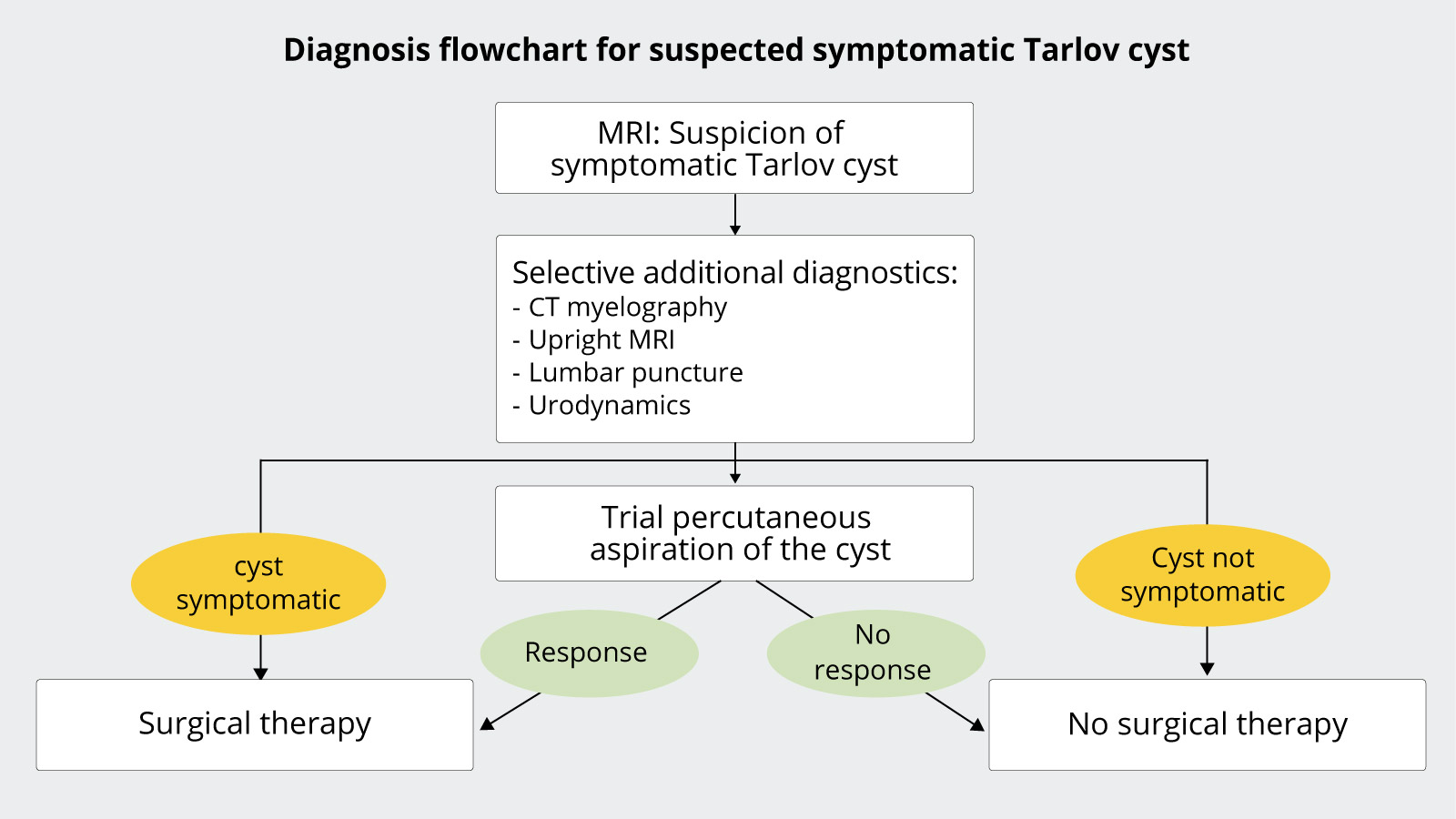
How is a Tarlov cyst diagnosed?
Tarlov cysts are usually visible in magnetic resonance imaging (MRI) of the spine. Based on this, further diagnostic measures such as CT myelography and urodynamic examination are used selectively.
How is a Tarlov cyst treated?
If a Tarlov cyst is detected by imaging, careful investigation is needed to determine whether it is actually the cause of the symptoms, as it is not always responsible for them *. As mentioned earlier, the majority of Tarlov cysts do not cause any symptoms and should therefore not be treated *. This does not mean that patients' complaints are not credible, but that they often exist independently of the cyst.
Larger cysts (>1–1.5 cm) can, however, cause radicular pain or bladder and bowel dysfunction, and in such cases treatment should be considered *, *. In particular, patients whose symptoms worsen when they change position or strain could benefit from therapy *. A thorough examination and additional diagnostic tests are essential.
Surgical treatment
To determine whether surgery is appropriate, it may be helpful to first drain the cyst using a CT-guided needle. If patients experience symptom relief, they are likely to benefit from surgical treatment. *
Treatment options
The optimal surgical approach for Tarlov cysts is still a matter of debate *, *. There are various approaches that can be divided into three categories:
- reducing the pressure of the cyst: This is done by draining the cerebral fluid to reduce the pressure in the cyst (e.g. lumboperitoneal shunt). *, *
- removing fluid from the cyst: The cyst is punctured to drain the fluid. However, this method has a high rate of relapse. *, *, *
- open surgical cyst lifting: This is usually done by ligating the communication with the dural tube . *, *, *, *, *, *
Careful patient selection and individually tailored therapy are crucial for successful treatment.
Possible complications
According to studies, the rate of complications after surgery is between 5 and 20%. The most common complications are infections, cerebrospinal fluid loss (CSF leaks), temporary pain intensification, sexual dysfunction and problems with bladder and bowel emptying. In addition, cyst recurrence can be expected in about 30% of patients. *, *
The frequency of complications also depends to a large extent on the surgeon's experience with this procedure.
Our experience at Inselspital
Many patients benefit from surgical treatment if they have been carefully selected. However, a significant improvement in symptoms can only be expected in about 50% of patients, although higher numbers are reported in many studies. *, *, *, *, *, *, *, *
The treatment is most successful for radicular pain, i.e. pain that originates from one or more nerve roots in the area of the spine. It has a rather limited effect on sexual dysfunction. *, *, * For voiding problems, the duration of the symptoms plays an important role: the shorter they have been present, the better the prognosis.
Ideal candidates for surgery are patients with large cysts (over 1.5 cm) and short-term radicular symptoms. *
-
Acosta FL Jr, Quinones-Hinojosa A, Schmidt MH, Weinstein PR. Diagnosis and management of sacral Tarlov cysts. Case report and review of the literature. Neurosurg Focus. 2003 Aug 15;15(2):E15.
-
Tarlov IM. Spinal perineurial and meningeal cysts. J Neurol Neurosurg Psychiatry. 1970 Dec;33(6):833-43.
-
Lucantoni C, Than KD, Wang AC, Valdivia-Valdivia JM, Maher CO, La Marca F, Park P. Tarlov cysts: a controversial lesion of the sacral spine. Neurosurg Focus. 2011 Dec;31(6):E14.
-
Hulens M, Rasschaert R, Bruyninckx F, Dankaerts W, Stalmans I, De Mulder P, Vansant G. Symptomatic Tarlov cysts are often overlooked: ten reasons why-a narrative review. Eur Spine J. 2019 Oct;28(10):2237-2248.
-
Nabors MW, Pait TG, Byrd EB, Karim NO, Davis DO, Kobrine AI, Rizzoli HV. Updated assessment and current classification of spinal meningeal cysts. J Neurosurg. 1988 Mar;68(3):366-77.
-
Elsawaf A, Awad TE, Fesal SS. Surgical excision of symptomatic sacral perineurial Tarlov cyst: case series and review of the literature. Eur Spine J. 2016 Nov;25(11):3385-3392.
-
Voyadzis JM, Bhargava P, Henderson FC. Tarlov cysts: a study of 10 cases with review of the literature. J Neurosurg. 2001 Jul;95(1 Suppl):25-32.
-
Neulen A, Kantelhardt SR, Pilgram-Pastor SM, Metz I, Rohde V, Giese A. Microsurgical fenestration of perineural cysts to the thecal sac at the level of the distal dural sleeve. Acta Neurochir (Wien). 2011 Jul;153(7):1427-34; discussion 1434.
-
Huang Q, Li J, Zhou Q, Li H, Yang X, Peng L, Chen L, Qi S, Lu Y. Management of Symptomatic Sacral Perineural Cysts: A New Surgical Method. World Neurosurg. 2022 Nov;167:e978-e989.
-
Langdown AJ, Grundy JR, Birch NC. The clinical relevance of Tarlov cysts. J Spinal Disord Tech. 2005 Feb;18(1):29-33.
-
Paulsen RD, Call GA, Murtagh FR. Prevalence and percutaneous drainage of cysts of the sacral nerve root sheath (Tarlov cysts). AJNR Am J Neuroradiol. 1994 Feb;15(2):293-7; discussion 298-9.
-
Kuhn FP, Hammoud S, Lefèvre-Colau MM, Poiraudeau S, Feydy A. Prevalence of simple and complex sacral perineural Tarlov cysts in a French cohort of adults and children. J Neuroradiol. 2017 Feb;44(1):38-43.
-
Klepinowski T, Orbik W, Sagan L. Global incidence of spinal perineural Tarlov's cysts and their morphological characteristics: a meta-analysis of 13,266 subjects. Surg Radiol Anat. 2021 Jun;43(6):855-863.
-
Ma Q, Xie J, Yang C, Wu C, Zhang J, Yin X, Si Y, Liu Y, Yang J, Sun J. Multiple dimensions of radiographic reconstruction for the optimal operative strategy of sacral meningeal cysts. Eur Spine J. 2022 Nov;31(11):3146-3158.
-
Sugawara T, Higashiyama N, Tamura S, Endo T, Shimizu H. Novel wrapping surgery for symptomatic sacral perineural cysts. J Neurosurg Spine. 2021 Oct 1;36(2):185-192.
-
Fletcher-Sandersjöö A, Mirza S, Burström G, Pedersen K, Kuntze Söderqvist Å, Grane P, Fagerlund M, Edström E, Elmi-Terander A. Management of perineural (Tarlov) cysts: a population-based cohort study and algorithm for the selection of surgical candidates. Acta Neurochir (Wien). 2019 Sep;161(9):1909-1915.
-
Medani K, Lawandy S, Schrot R, Binongo JN, Kim KD, Panchal RR. Surgical management of symptomatic Tarlov cysts: cyst fenestration and nerve root imbrication-a single institutional experience. J Spine Surg. 2019 Dec;5(4):496-503.
-
Feigenbaum F, Parks SE, Chapple KM. Prospective Validation of a Quality-of-Life Measure for Women Undergoing Surgical Intervention for Symptomatic Sacral Tarlov Cysts: The Tarlov Cyst Quality of Life Scale. World Neurosurg. 2022 Sep;165:e276-e281.
-
Feigenbaum F, Boone K. Persistent Genital Arousal Disorder Caused by Spinal Meningeal Cysts in the Sacrum: Successful Neurosurgical Treatment. Obstet Gynecol. 2015 Oct;126(4):839-843.
-
Lim VM, Khanna R, Kalinkin O, Castellanos ME, Hibner M. Evaluating the discordant relationship between Tarlov cysts and symptoms of pudendal neuralgia. Am J Obstet Gynecol. 2020 Jan;222(1):70.e1-70.e6.
-
Porche K, Hoh DJ. Editorial. Microsurgical treatment of sacral Tarlov cysts. J Neurosurg Spine. 2022 Jul 1;37(6):902-903.
-
Morio Y, Nanjo Y, Nagashima H, Minamizaki T, Teshima R. Sacral cyst managed with cyst-subarachnoid shunt: a technical case report. Spine (Phila Pa 1976). 2001 Feb 15;26(4):451-3.
-
Sharma M, SirDeshpande P, Ugiliweneza B, Dietz N, Boakye M. A systematic comparative outcome analysis of surgical versus percutaneous techniques in the management of symptomatic sacral perineural (Tarlov) cysts: a meta-analysis. J Neurosurg Spine. 2019 Feb 8;30(5):623-634.
-
Tsitsopoulos PP, Marklund N, Salci K, Holtz A, Mani M. Management of symptomatic sacral perineural cysts with microsurgery and a vascularized fasciocutaneous flap. J Spine Surg. 2018 Sep;4(3):602-609.
-
Chu W, Chen X, Wen Z, Xue X, He G, Zhang H, Liu J, Zhang Y, Feng H, Lin J. Microsurgical sealing for symptomatic sacral Tarlov cysts: a series of 265 cases. J Neurosurg Spine. 2022 Jul 1;37(6):905-913.
-
Galarza M, Chaban G, Gazzeri R, de la Rosa P, Montoya CG, Laut MM, Sosa F. Functional recovery following resection of large Tarlov cyst malformation: a multicentre longitudinal cohort study. Acta Neurochir (Wien). 2021 Oct;163(10):2769-2776.
-
Sun JJ, Wang ZY, Teo M, Li ZD, Wu HB, Yen RY, Zheng M, Chang Q, Yisha Liu I. Comparative outcomes of the two types of sacral extradural spinal meningeal cysts using different operation methods: a prospective clinical study. PLoS One. 2013 Dec 26;8(12):e83964.
-
Guo D, Shu K, Chen R, Ke C, Zhu Y, Lei T. Microsurgical treatment of symptomatic sacral perineurial cysts. Neurosurgery. 2007 Jun;60(6):1059-65; discussion 1065-6.
-
Burke JF, Thawani JP, Berger I, Nayak NR, Stephen JH, Farkas T, Aschyan HJ, Pierce J, Kanchwala S, Long DM, Welch WC. Microsurgical treatment of sacral perineural (Tarlov) cysts: case series and review of the literature. J Neurosurg Spine. 2016 May;24(5):700-7.
-
Warnke JP, Mourgela S. Endoscopic treatment of lumbar arachnoiditis. Minim Invasive Neurosurg. 2007 Feb;50(1):1-6
-
Di Ieva A, Barolat G, Tschabitscher M, Rognone E, Aimar E, Gaetani P, Tancioni F, Lorenzetti M, Crotti FM, Rodriguez Baena R, Warnke JP. Lumbar arachnoiditis and thecaloscopy: brief review and proposed treatment algorithm. Cent Eur Neurosurg. 2010 Nov;71(4):207-12
-
Warnke JP, Tschabitscher M, Nobles A. Thecaloscopy: the endoscopy of the lumbar subarachnoid space, part I: historical review and own cadaver studies. Minim Invasive Neurosurg. 2001 Jun;44(2):61-4.
-
Warnke JP, Köppert H, Bensch-Schreiter B, Dzelzitis J, Tschabitscher M. Thecaloscopy part III: first clinical application. Minim Invasive Neurosurg. 2003 Apr;46(2):94-9.
-
Warnke JP, Mourgela S, Tschabitscher M, Dzelzitis J. Thecaloscopy part II: anatomical landmarks. Minim Invasive Neurosurg. 2001 Dec;44(4):181-5.
-
Warnke JP, Di X, Mourgela S, Nourusi A, Tschabitscher M. Percutaneous approach for thecaloscopy of the lumbar subarachnoidal space. Minim Invasive Neurosurg. 2007 Jun;50(3):129-31.
-
Warnke JP, Mourgela S. Lumbale adhäsive Arachnoiditis. Endoskopische Subarachnoepidurostomie als neue Behandlungsmöglichkeit [Adhesive lumbar arachnoiditis. Endoscopic subarachnoepidurostomy as a new treatment]. Nervenarzt. 2007 Oct;78(10):1182-7. German.
-
Mauer UM, Gottschalk A, Kunz U, Schulz C. Arachnoscopy: a special application of spinal intradural endoscopy. Neurosurg Focus. 2011 Apr;30(4):E7.
-
Maxmauer U, Danz B, Gottschalk A, Kunz U. Endoscope-assisted surgery of spinal intradural adhesions in the presence of cerebrospinal fluid flow obstruction. Spine (Phila Pa 1976). 2011 May 20;36(12):E773-9.
-
Kameda-Smith MM, Fathalla Z, Ibrahim N, Astaneh B, Farrokhyar F. A systematic review of the efficacy of surgical intervention in the management of symptomatic Tarlov cysts: a meta-analysis. Br J Neurosurg. 2024 Feb;38(1):49-60.
-
Wang Z, Jian F, Chen Z, Wu H, Wang X, Duan W, Wang K, Guan J, Liu Z. Percutaneous Spinal Endoscopic Treatment of Symptomatic Sacral Tarlov Cysts. World Neurosurg. 2022 Feb;158:e598-e604.