A herniated disc of the cervical spine, also known as cervical disc herniation or cervical disc hernia, is a common condition that can occur from middle age. Wear, loss of elasticity and tears in the fibrous ring of the disc are the causes. In the process, nerves or the spinal cord can be compressed and damaged, causing symptoms. Treatment depends primarily on the severity of the symptoms. If the pain is bearable and there are no neurological deficits, a classic treatment with physiotherapy and medication is sufficient. However, if there is no improvement for weeks or if the symptoms progress, surgery should be performed. The operation is a relatively short, microsurgical procedure in which the affected nerve and spinal cord are relieved from pressure.
Our experience at Inselspital
Decompression of the nerves structures in the cervical spine is performed at Inselspital by a specialized neurosurgical spine team. Minimally invasive and microsurgical techniques, such as surgery under a high-resolution microscope, are part of the daily standard in neurosurgery. They enable an operation that is gentle on the tissue and ensure that our patients recover more quickly.
At Inselspital, specialists from all disciplines work closely together under one roof and coordinate with each other. Thanks to the cooperation of rheumatology, physiotherapy, neurology, neuroradiology, pain center and orthopedics on a daily basis, the optimal treatment strategy can be developed for our patients. Complicated cases are discussed in an interdisciplinary board and often operated on jointly by neurosurgeons and orthopedists. In this way, we create the conditions for the best possible treatment for each individual patient.
What is the cause of a herniated disc in the cervical spine?
A herniated disc is the result of aging and wear and tear of the spine, which begins as early as the age of 20. The incidence of the disease increases continuously up to the age of 45 and then slightly decreases again. Heavy physical work, incorrect strain and genetic factors favor these processes and degenerative changes. Additional risk factors such as smoking also play an important role.
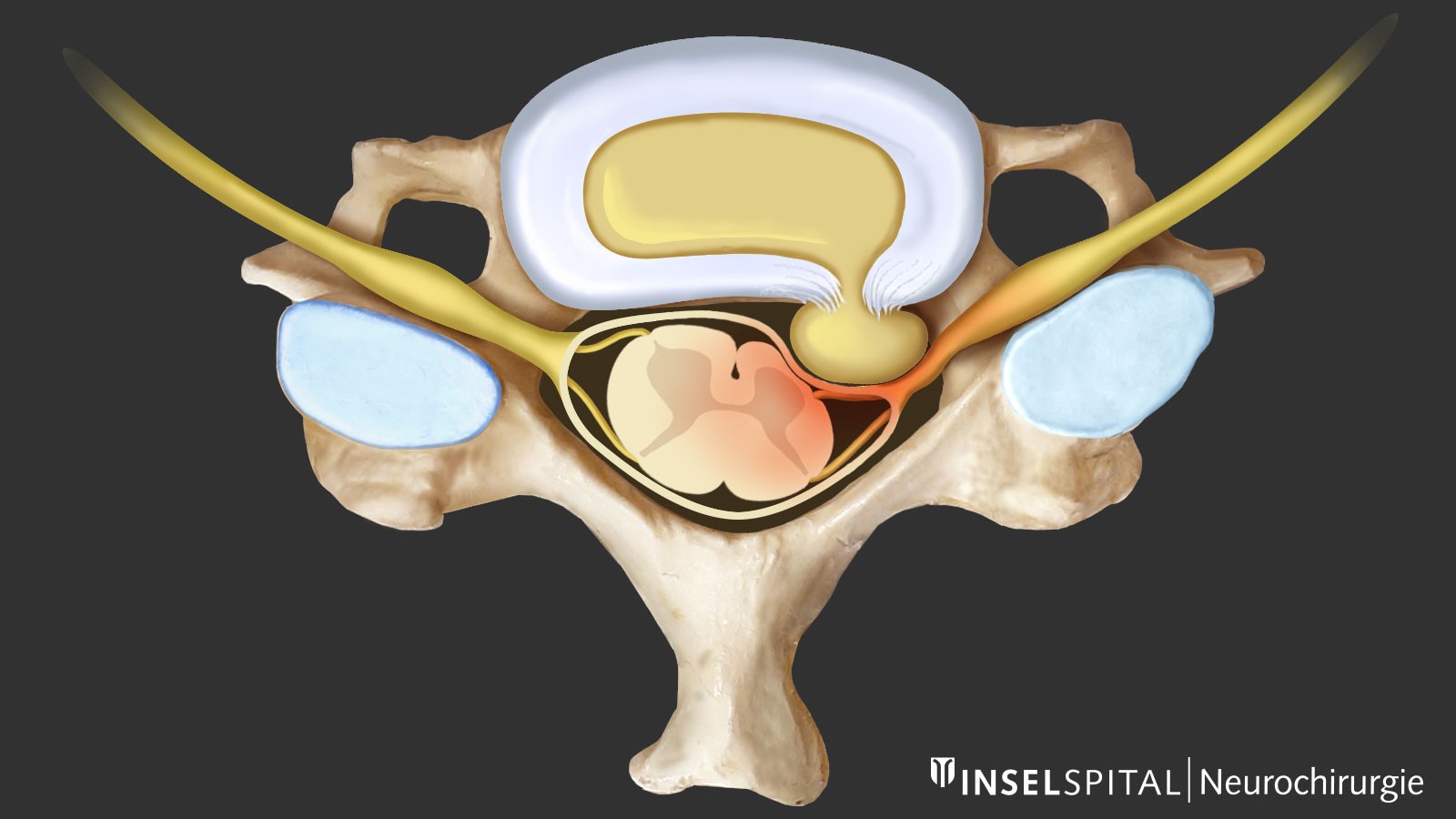
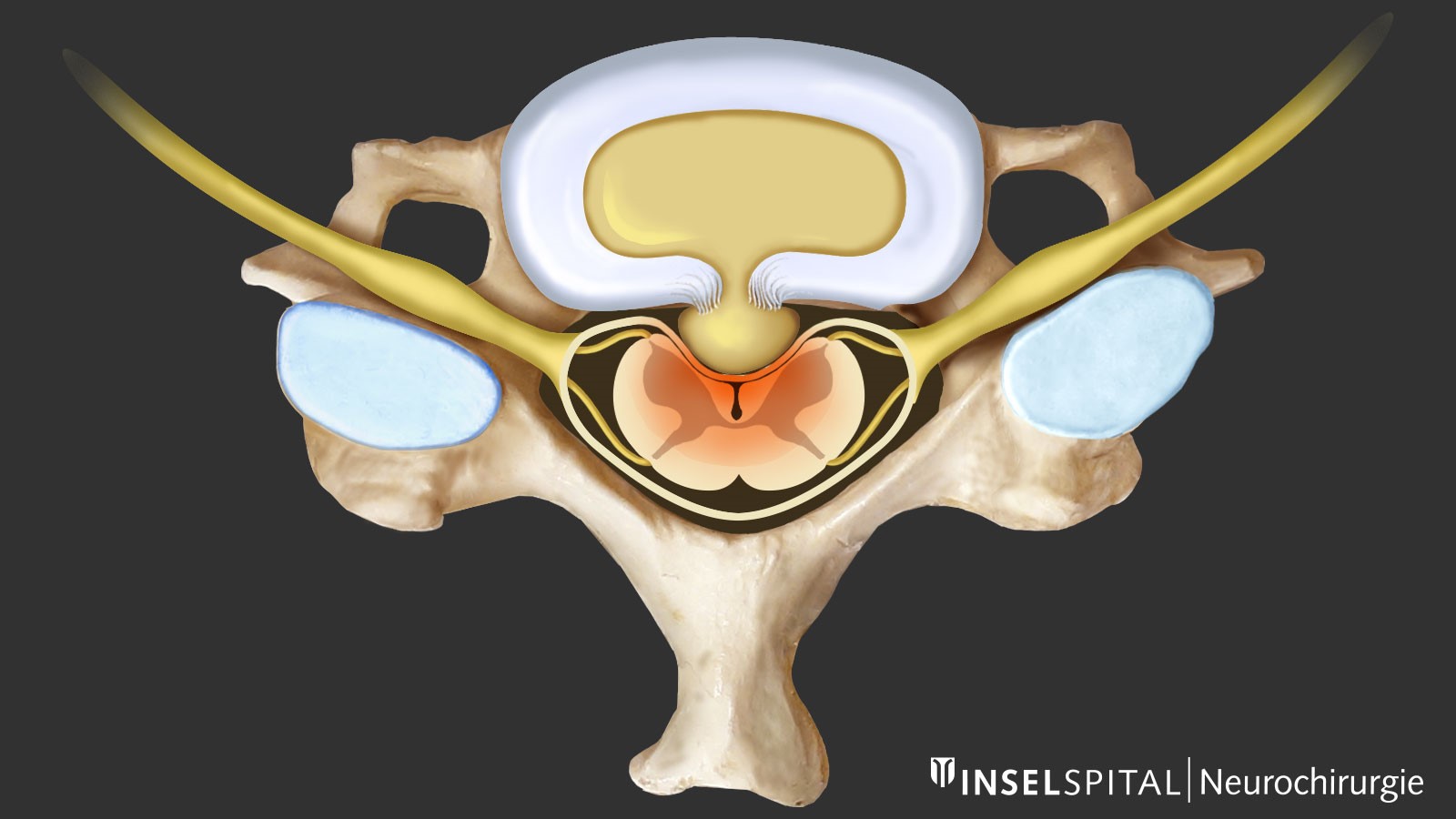
Tears develop in the outer fibrous ring of the intervertebral disc (annulus fibrosus) so that pieces of tissue can escape from the interior of the intervertebral disc (nucleus pulposus) into the nerve canal. These pieces of disc can compress the nerves or the spinal cord and cause the corresponding symptoms. There are no endogenous repair mechanisms in the disc space itself, which is why advanced degeneration can no longer heal spontaneously.
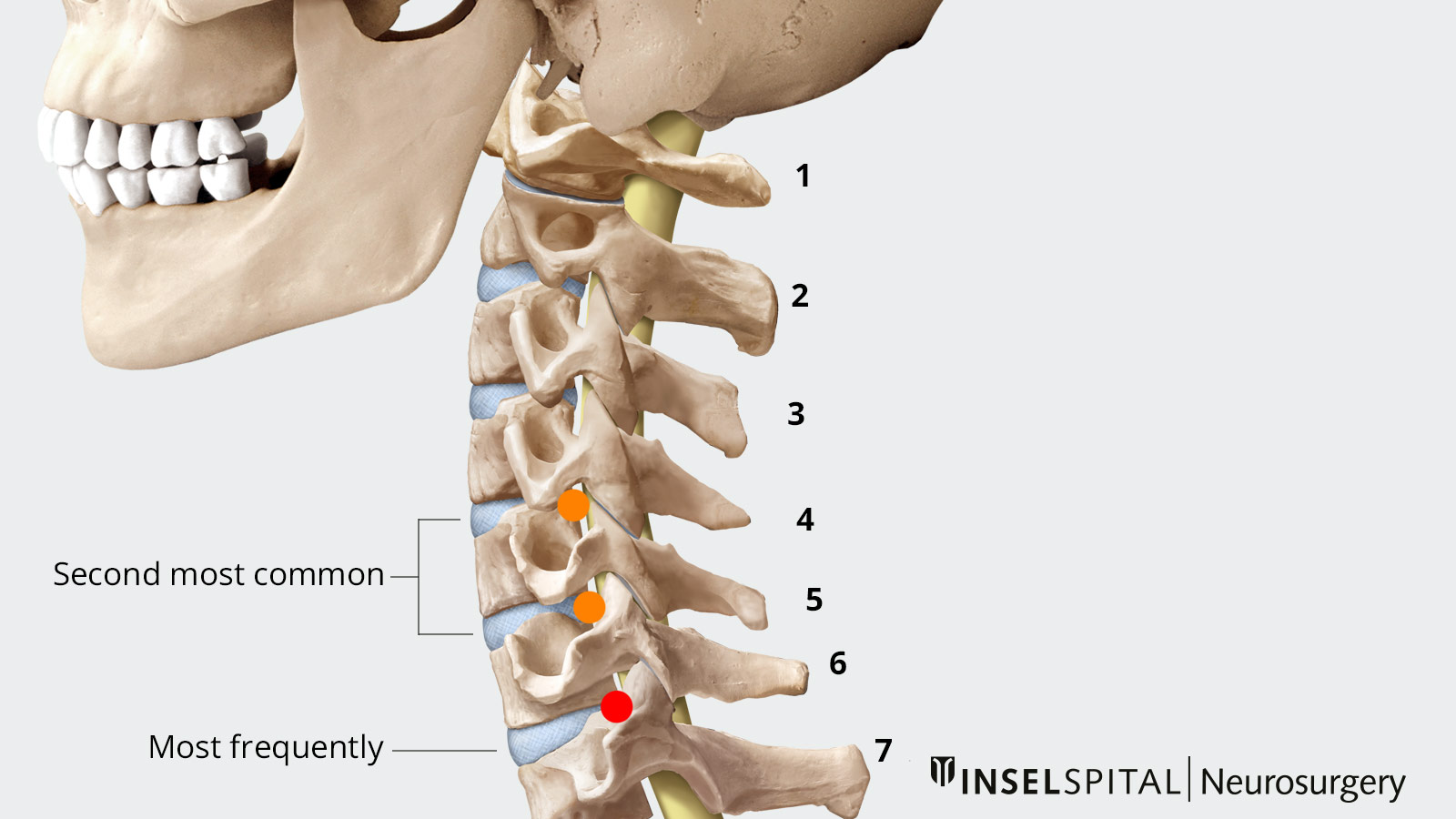
Where does the herniated disc occur most frequently?
The most common location for a herniated cervical disc is between the 6th and 7 th cervical vertebrae. The second most common location is between the 5 th and 6 th or between the 4 th and 5th cervical vertebrae. Men are usually affected more often than women.
Can an accident cause a disc hernia?
In exceptional cases, yes. However, trauma can only be claimed as the cause in cases of considerable violence in patients who were previously completely symptom-free. So-called "lifting trauma" is generally not recognized by insurance companies as an accidental cause of herniated discs.
What is the difference to cervical spinal stenosis?
Cervical spinal stenosis is a narrowing of the spinal canal or the nerve exit canals of the spine (neuroforamen). Although cervical spinal stenosis has many similarities in treatment to cervical disc herniation, it is a condition that occurs more frequently at an older age (> 50 years) and can be associated with rheumatoid diseases. In the case of a herniated disc, the patient has the chance that the symptoms will improve on their own with the resorption of the tissue fragments. With stenosis, on the other hand, spontaneous improvement is rarer.
What are the most frequent symptoms?
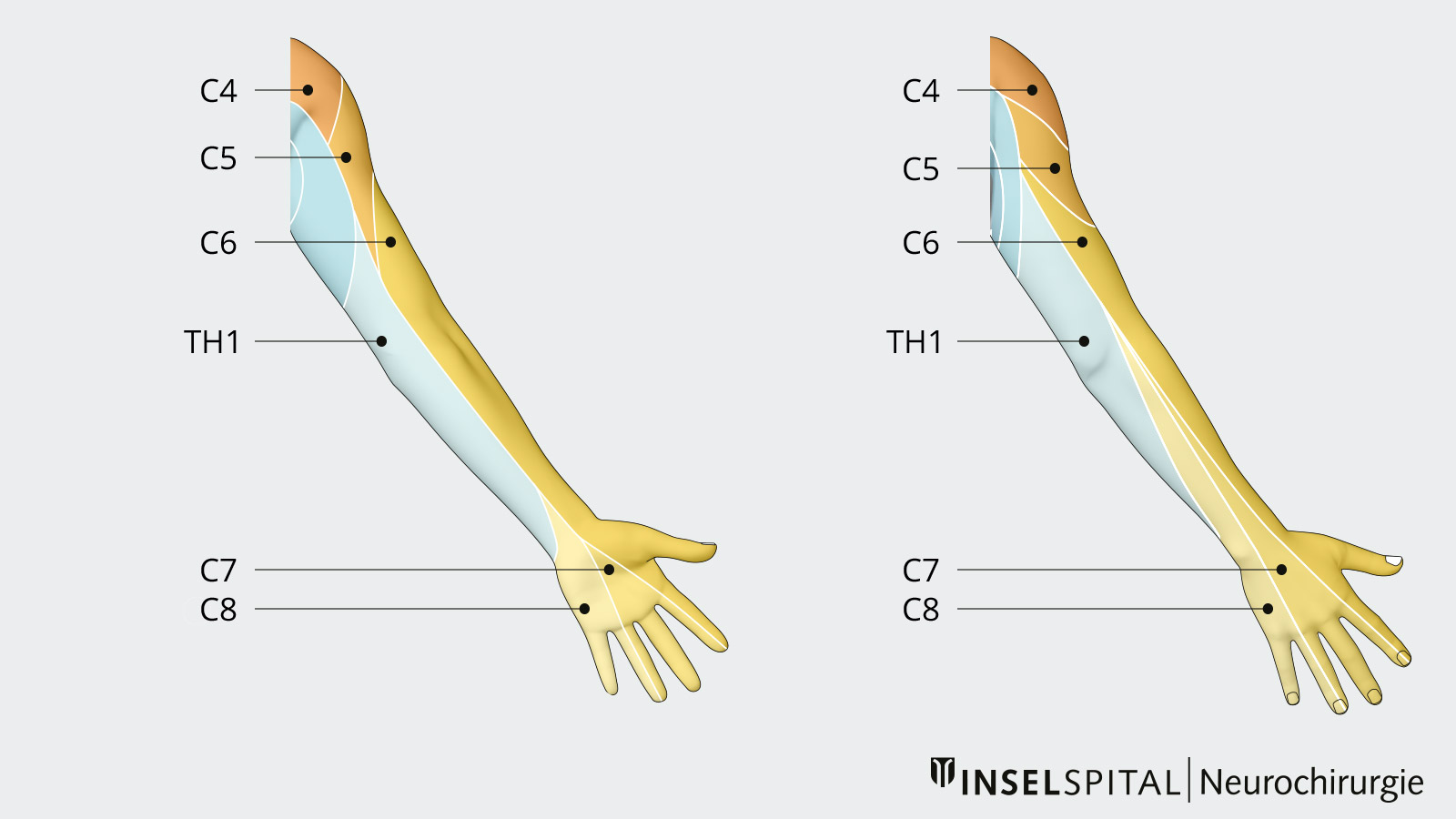
A herniated disc of the cervical spine often causes a pain sensation in the neck and at the same time in the arm – the characteristic radicular pain (originating from the nerve roots). Depending on the affected nerve root, patients then describe, for example, a typical radiation of pain into the thumb, the middle fingers or even just the little finger. The radicular arm pain can be accompanied by a loss of strength and sensitivity. Such symptoms are signs of significant compression of a nerve. Each nerve has a specific area of pain and sensory misperception and supplies different muscles. For example, if there is a cervical disc herniation at the level of C6/C7 on the right side, this can lead to compression of the C7 nerve root. This in turn can be associated with pain in the area of the posterior upper and lower arm up to the index and middle finger of the right hand. Clinical examination often shows a reduction in the triceps tendon reflex, which depends on an intact C7 root. There may also be weakness in elbow and wrist extension. Thus, there is a specific pattern of deficits and disorders for each nerve.
If the herniated disc is located in the center of the spinal canal, compression of the spinal cord may occur. This manifests itself as gait or coordination disorder as well as weakness and sensory disorders in the legs. This spinal cord damage (myelopathy), which is also visible in the MRI image, is one of the severe symptoms and must be investigated as soon as possible. In the worst and rarest cases, myelopathy can lead to a paraplegic syndrome.
How is a cervical disc hernia diagnosed?
Every diagnosis is preceded by a detailed interview and focused neurological examination. The clinical suspicion must then be confirmed with imaging. The examination of choice is a magnetic resonance imaging (MRI) of the cervical spine. The computed tomography (CT) is more focused on the bone. For special questions and in patients with a contraindication to MRI imaging, myelo-CT is also available.
As with many other degenerative diseases of the spine, a cervical disc herniation can also progress without symptoms and be a purely visual finding.
If the clinical symptoms and the image findings do not correspond to a herniated disc, other causes must also be considered. Tumors, inflammations, diseases of the ligamentous apparatus (such as periarthropathia humeroscapularis, epicondylitis radialis) or compression syndromes of the brachial plexus and the peripheral nerves are possible.
What are the treatment options?
Conservative therapy
Since most patients do not have any major neurological symptoms, conservative therapy is the primary treatment for pain. This includes individually adapted pain medication, rest and relief during the acute phase and, in the case of severe symptoms, an injection of cortisone directly into the nerve root. These measures lead to an improvement of the symptoms within the first 6–8 weeks in 90% of all patients with acute radicular pain as a result of a herniated disc with nerve root compression without the need for surgery.
Nerve root infiltration
In patients with persistent radicular pain under conservative therapy, a CT-guided nerve root infiltration can lead to symptom relief. In this procedure, a local injection of anti-inflammatory (cortisol) and analgesic (lidocaine) is administered into the area of the compressed nerve under constant careful CT monitoring. This treatment can be repeated at intervals of a few weeks and shows a success rate of about 70% in pain reduction.
Surgical treatment
Rapid surgical intervention is indicated in cases of severe pain, paralysis and disorders in urination (urinary retention, involuntary urination) or defecation. On the other hand, the indication for surgery in cases of treatment-resistant moderate pain is relative and strongly dependent on the degree of suffering of the patient.
Relative surgical indications are:
- Lack of pain relief under conservative therapy and high patient suffering after 6–8 weeks or earlier in individual cases.
Absolute surgical indications are:
- Patients with clear signs of paralysis
- Significant compression of the spinal cord due to a large herniated disc and signs of myelopathy on imaging (with or without neurological deficits).
How does a cervical disc surgery work?
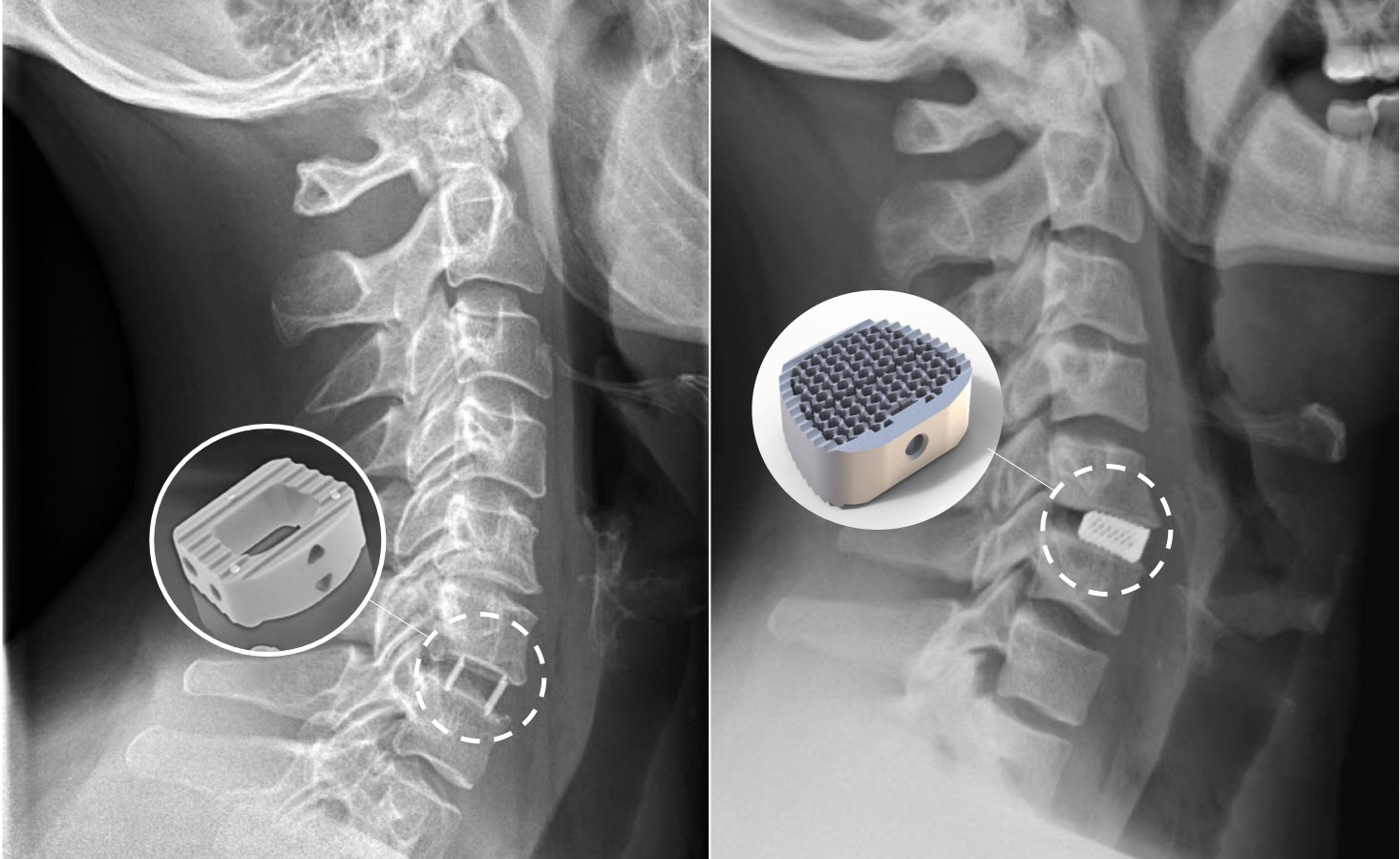
The type of surgical treatment depends primarily on the localization of the herniated disc. The operation is performed either from the front with replacement of the disc by a prosthesis or a cage implant, or from the back by a pure decompression.
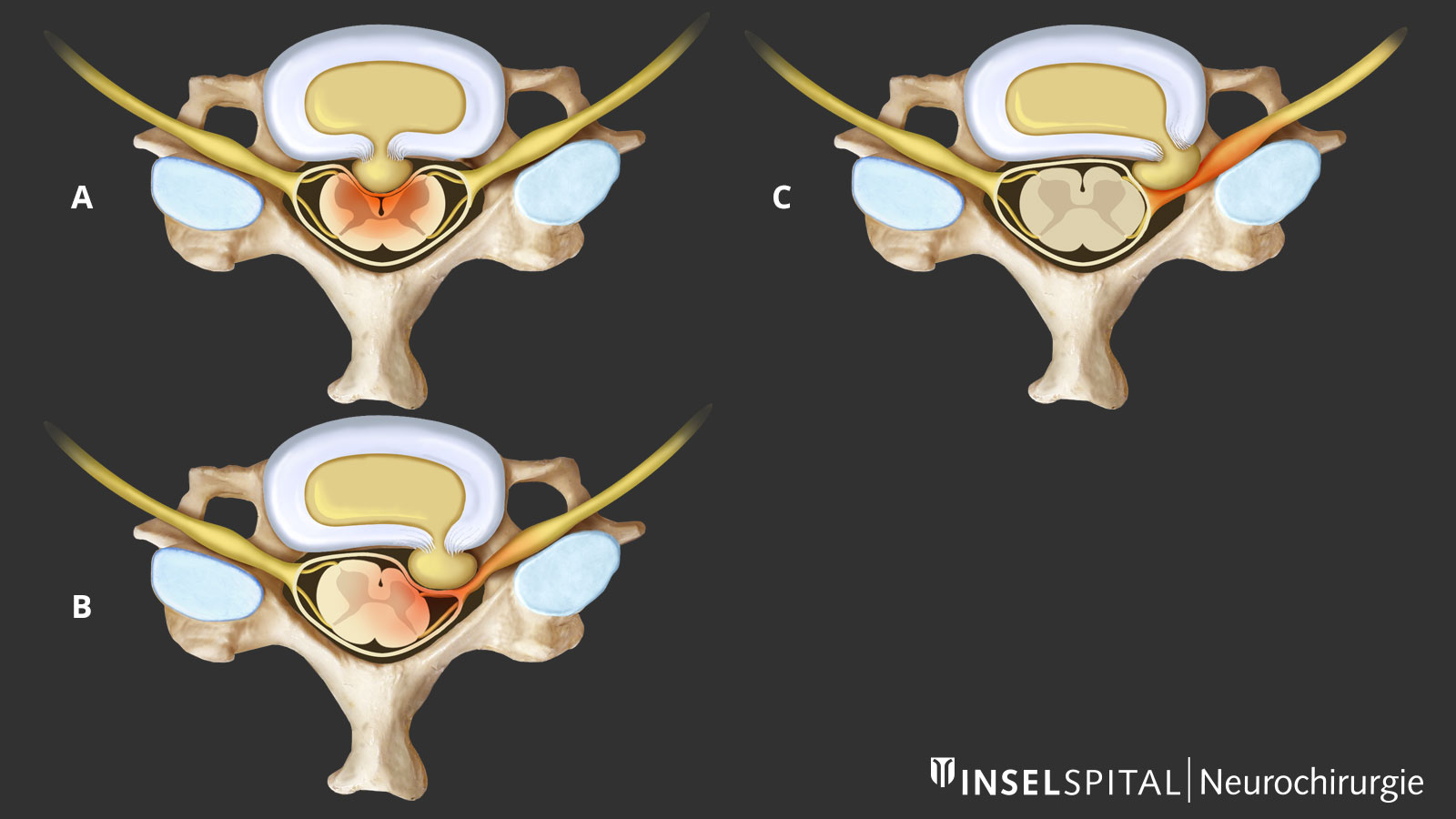
| Localization | Meaning | Surgical approach |
|---|---|---|
| Median | The herniated disc is centrally located and often leads to compression of the spinal cord. Radicular pain radiation is rather rarely present in these cases. | From the front with removal of the intervertebral disc |
| Paramedian | The herniated disc is located laterally and can lead to unilateral nerve root compression and pain in the arm. | From the front with removal of the intervertebral disc or from behind by pure decompression (foraminotomy according to Frykholm). |
| Foraminal | Most of the herniated disc is located in the intervertebral foramen. This is the exit channel of the cervical nerve from the spinal canal and is located on the very outside. These herniated discs are associated with unilateral nerve root pain. | From the front with removal of the intervertebral disc or from behind by pure decompression (foraminotomy according to Frykholm). |
Surgery from the front (anterior approach)
Median and paramedian disc hernias can be operated on through an anterior approach. This involves removing the affected disc and the part pressing on the nerve or spinal cord through a 4 cm incision under the surgical microscope. A cage implant is inserted as a replacement to maintain or reconstruct the shape of the spine and the height of the disc space. The aim of this operation is a bony fusion between the vertebrae. This technique is accompanied by a slight loss of cervical spinal mobility (approx. 7º per segment), which does not interfere with everyday life, but leads to increased wear in the adjacent segment in 3% of patients.
The alternative operation is the implantation of a disc prosthesis. It maintains mobility in the operated segment and thus prevents too much strain on the neighboring segments. Large studies have shown the success and, if used correctly, also the superiority of the disc prosthesis compared to conventional fusion. However, criteria such as the age of the patient, the position and mobility of the spine and the underlying pathology must be taken into account. In addition, neck pain can occur later, as even the best prosthesis does not achieve the same joint mobility as the normal spine.
The risk of nerve root or spinal cord injury with the anterior approach is low, less than 1%. Possible complications include temporary hoarseness or dysphagia and local postoperative bleeding. Very rarely, a displacement of the cage or the prosthesis is observed.
Surgery from behind (posterior approach)
In the case of isolated foraminal or lateral disc herniations of the cervical spine, a minimally invasive decompression of the affected nerve root from behind via the neck can be considered. This surgical procedure is also called the Frykholm operation. The procedure is performed using the so-called MISS technique (minimally invasive spine surgery) via a tubular system without major muscle or bone trauma. In this operation, only the prolapse is removed, while the disc is left in place. The success rates of this technique are around 90%.
Intraoperative neuromonitoring
In the Department of Neurosurgery at Inselspital, special intraoperative neuromonitoring is used for operations on the spinal column with existing compression of the spinal cord. This procedure significantly increases the safety of the operations. With neuromonitoring, the nerve pathways are electrophysiologically stimulated during the operation and the response signals in the nerve are measured. These then in turn lead to the adjustment of the surgical procedure. Important functional areas can thus be efficiently spared.
How long does recovery take after the operation?
After one of the described operations on the cervical spine, it is not necessary to wear a cervical collar. The patient can go home from the 2nd day after the operation at the earliest; most patients stay with us at the clinic for about 4 days.
After an operation, a variable recovery time of 2–6 weeks must be expected. We see patients who can return to work on their laptops immediately the day after the operation, and others who have to wait until the bone wound has completely healed because of their physical activity. The rest period therefore depends on existing neurological deficits as well as the physical strain at work and will vary from case to case.