In contrast to primary brain tumors, brain metastases are metastases of tumor cells from a tumor located outside the brain. Whereas in the past a metastasis in the brain meant a poor prognosis, surgical treatment of brain metastases is now standard therapy. The different types of brain metastases require a personalized approach because they respond differently to surgery, radiosurgery, chemotherapy or standard radiation.
How common are brain metastases?
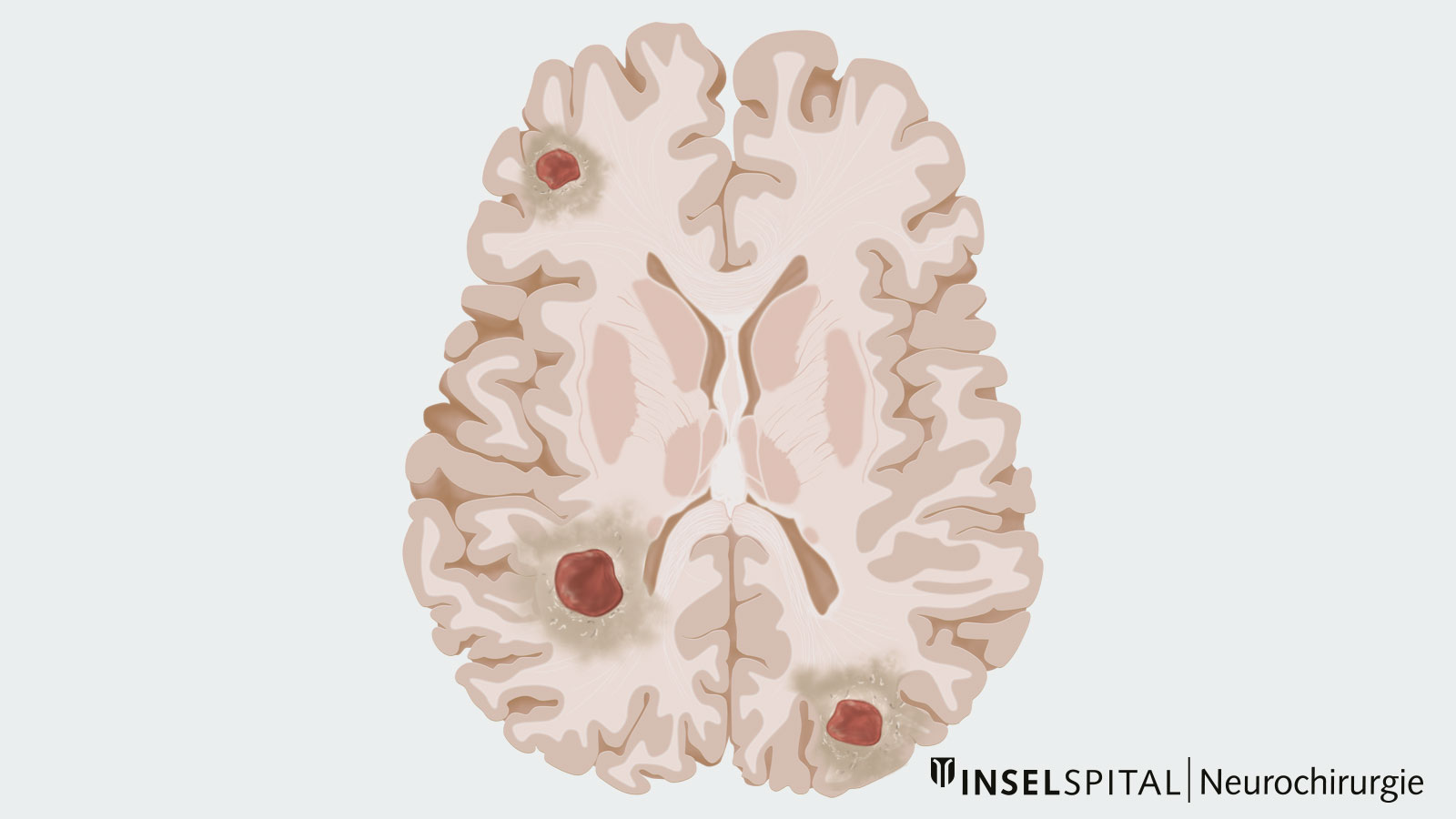
Brain metastases are the most common tumors in the brain in adults, occurring in 10–15 out of 100,000 individuals annually. In 30-50% of cases, they are singular metastases. However, multiple brain metastases are often already present *. Primary tumors of brain metastases are mainly tumors in the lung, breast, skin, colon and kidney. Of these primary tumors, melanoma, the black skin cancer, has the highest tendency to metastasize to the brain *. In about 10% of cases, the primary tumor is unknown when a brain metastasis is first diagnosed, which means that the metastasis in the brain is the patient's first symptom.
Brain metastases are the most common cause of neurological complications in tumor diseases, which are no longer localized to one organ but affect the whole body *. About 10–15% of all patients with systemic tumor disease develop brain metastases *, *.
What are the symptoms of brain metastases?
If the metastases are located in eloquent brain areas or close to them, they often cause symptoms such as failures of the visual field, speech disorders, sensory disturbances or reductions in strength. However, depending on the location and number of brain metastases, the symptoms of brain metastases are varied. For example, if a metastasis blocks the drainage of cerebrospinal fluid, it can lead to a buildup with headaches, nausea and vomiting. Also common are first-ever epileptic seizures or headaches as the most common leading symptom *.
- Headaches 24%
- Disturbances of functions (e.g., paralysis, visual disturbances, speech disturbances) 20%
- Cognitive and behavioral changes 14%
- Epileptic seizures (focal or generalized) 12%
- Ataxia (disturbances of movement coordination) 7%
In contrast, the incidental discovery of brain metastases during cranial imaging, without patients having had prior symptoms, is relatively rate at only about 7% *.
How are brain metastases diagnosed?
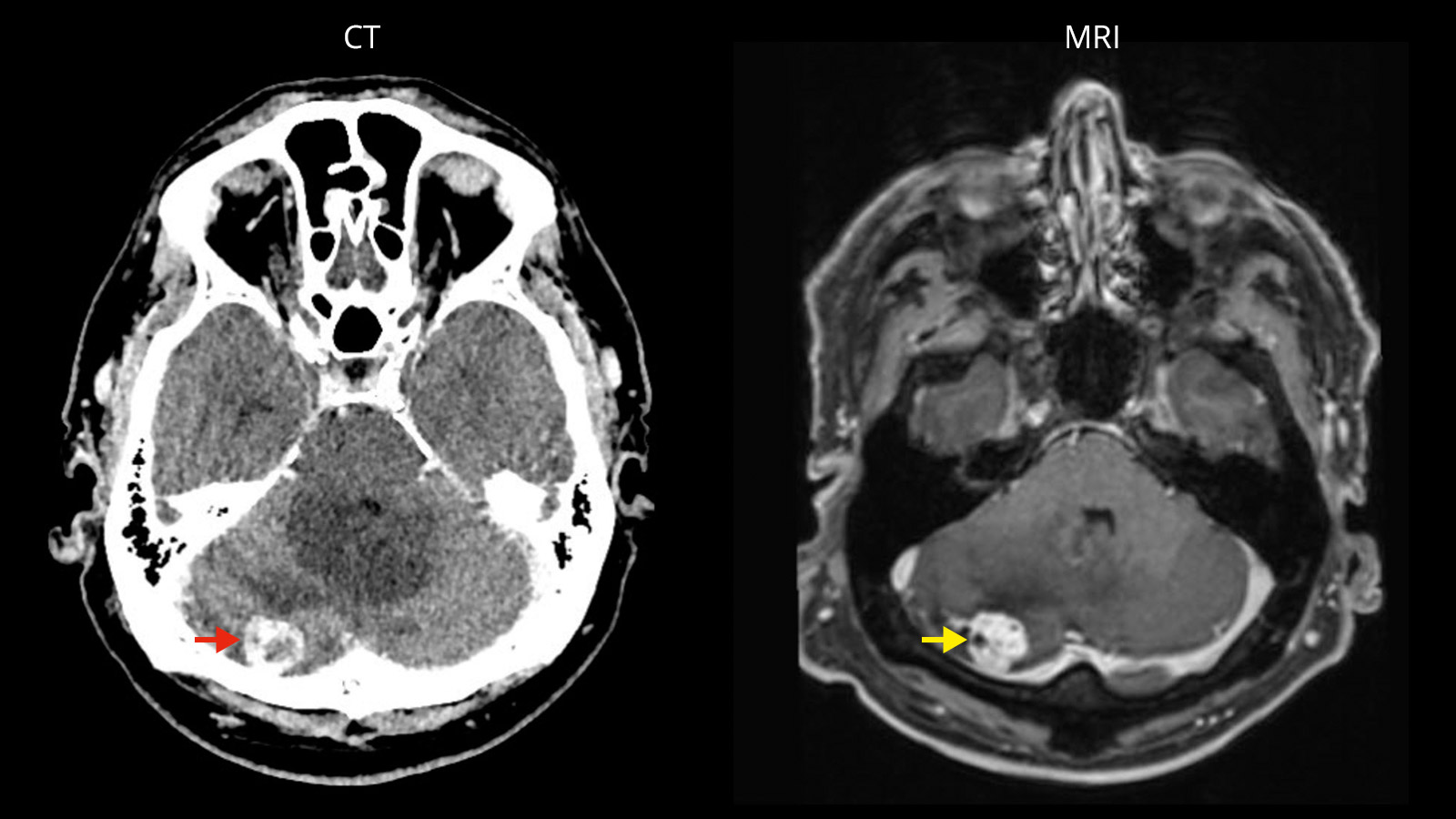
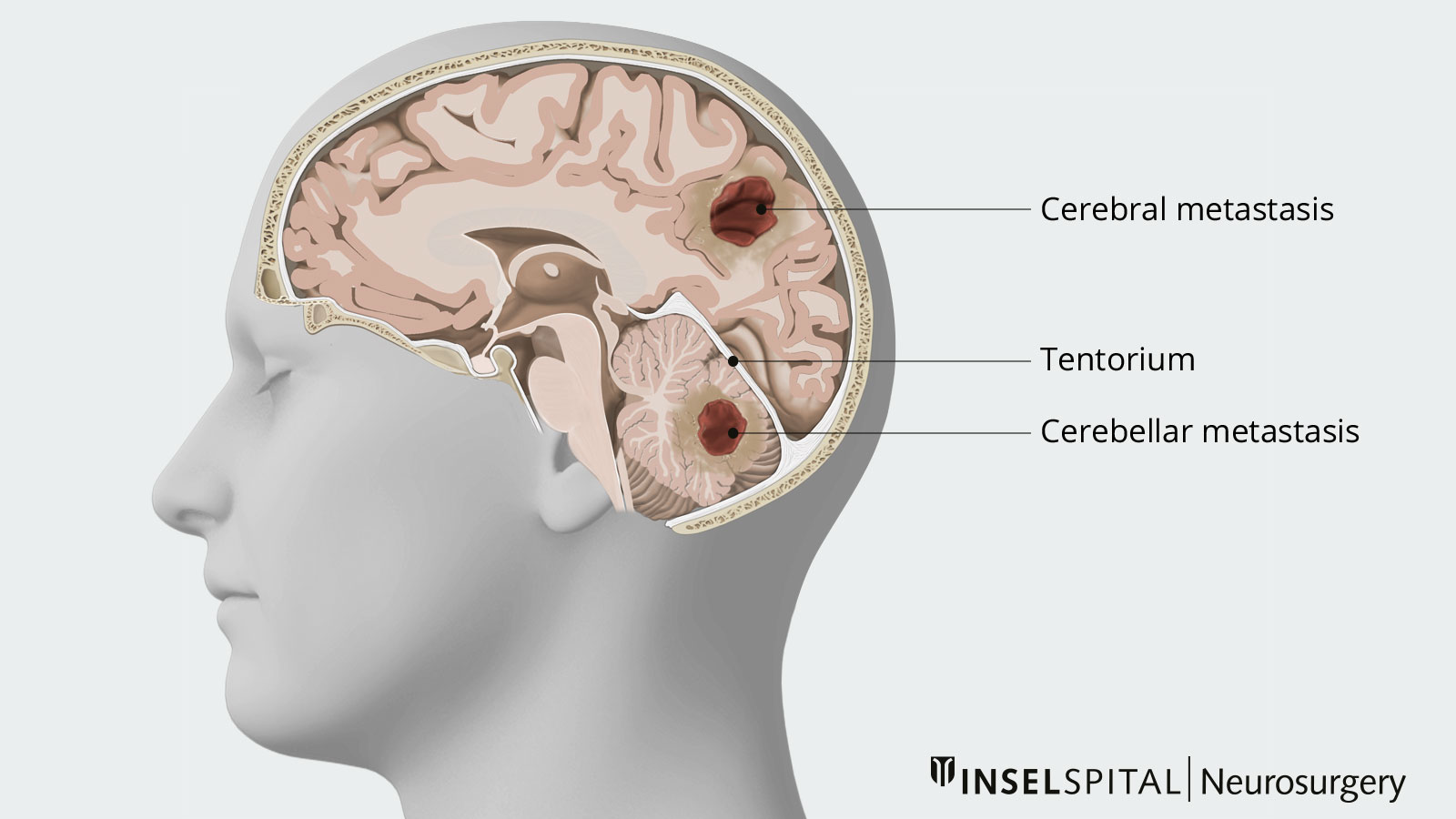
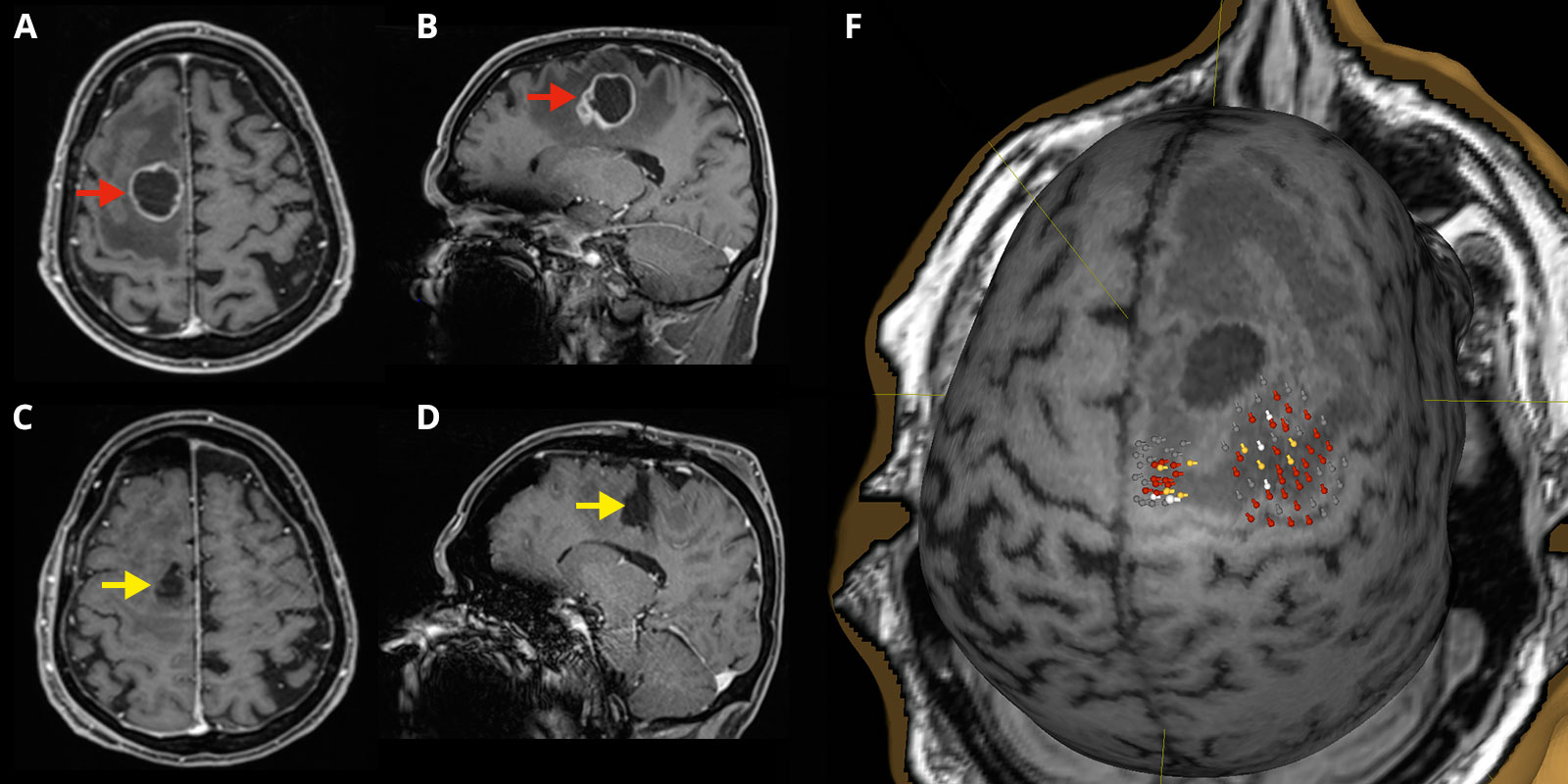
Brain metastases form solid or cystic tumors surrounded by edema, i.e., a pathological accumulation of fluid in the tissue. Brain metastases are diagnosed with magnetic resonance imaging (MRI) or, less frequently, with computed tomography (CT). MRI imaging is usually indispensable for surgical planning and to exclude further metastases.
Most brain metastases are localized in the cerebrum, but may also occur in the cerebellum in about 10% of cases. An exception are metastases from primary tumors in the pelvis and abdomen, which settle in the cerebellum with a frequency of up to 50% *.
If a brain metastasis is detected by imaging without a known primary tumor, further imaging of the chest and abdomen is performed to find the primary tumor as soon as possible. If a metastasis to the meninges is suspected, a rare and serious complication of tumor diseases, a diagnosis can also be made by sampling cerebrospinal fluid from the spinal canal, as the tumor cells can often be detected here.
Certified Brain Tumor Center
At Inselspital, the best possible treatment strategy is determined individually for each patient. This is done in the certified Brain Tumor Center, where an interdisciplinary team discusses and determines all treatment options individually for each patient.
This weekly tumor board is composed of specialists from neurosurgery, neurology, neuro-oncology, nuclear medicine, radio-oncology as well as pathology.
What is the best treatment for brain metastases?
In the past, brain metastases were indicative of end-stage systemic tumor disease with only a few weeks of survival remaining *. In the mid-20th century, the establishment of whole-brain radiation and the use of steroids resulted in a significant improvement in the average survival time as well as the quality of life of patients *.
Until 1990, surgical removal (resection) of brain metastases was highly controversial. Then two scientific studies *, * were able to demonstrate the clear benefit of surgical removal of brain metastases with supporting data.
Nowadays, the treatment of brain metastases is always carried out in a multidisciplinary approach, in which surgical resection plays a very decisive role in the success of the therapy. At Inselspital, each individual patient is discussed within the framework of our interdisciplinary neuro-oncological tumor board. Neurosurgeons, neurologists, neuroradiologists, oncologists and radiation oncologists jointly determine the optimal therapy for each individual patient.
Especially if no information on the primary tumor is available, a tissue sample is crucial for further therapy, because depending on the tumor, the response to further treatment by radiotherapy can vary greatly. For example, metastases from renal cell carcinoma and from melanoma respond significantly worse to standard radiotherapy than metastases from small cell lung cell carcinoma *. Radiosurgery is therefore more successful in the former.
Nowadays, there are various procedures and approaches that can be used in the treatment of brain metastases. Surgical removal of one or even several brain metastases, irradiation of the entire brain or a part of it, and targeted one-time irradiation of the metastasis(radiosurgery), in various repetitions or sequences, are all possible.
Why is supramarginal surgery for brain metastasis important?
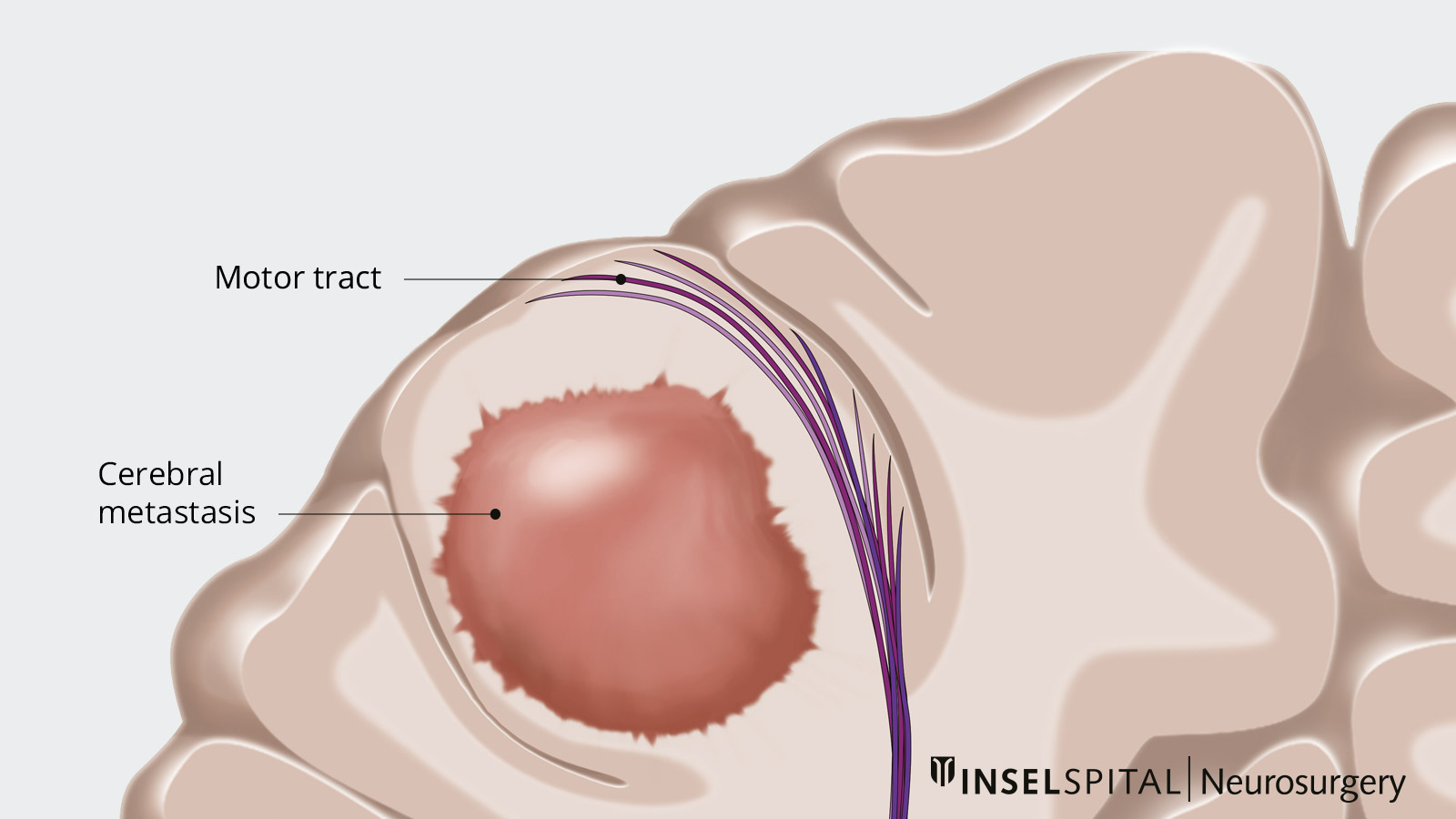
Although brain metastases, i.e., metastases of a primary tumor growing outside the brain, grow much less infiltratively compared to tumors growing inside the brain, the cells can penetrate up to 5 mm into the brain. Therefore, recurrences after surgery occurred frequently in the past. The supramarginal surgical technique aims to remove the infiltration zone as well. However, it requires electrophysiological monitoring in functionally important brain areas during surgery.
What are the main problems in treating brain metastases?
Assuming the tumor in the body is treated, under control, or cured, there are 3 major problem areas in the therapy of brain metastases:
- Brain metastases resistant to conventional standard radiation therapy (e.g., renal cell carcinoma, melanoma)
- Multiple brain metastases
- Local recurrences after surgery (approximately 30–40% in the literature).
- Subsequent metastases that were not visible at first (too small, or developed later, in 50% of patients
These constellations require different combinations of therapy methods.
Singular brain metastases
In patients with good prognostic prospects and single brain metastases larger than 3 cm, surgical resection is one of the most important cornerstones of therapy *. Studies have shown *, * that surgical resection followed by radiosurgery of the former tumor cavity leads not only to a significantly increased survival but also to a better quality of life. Standard radiation is less effective than radiosurgery, the effect of which is to kill any remaining single cell clusters in the surgical area. Radiosurgical treatment significantly reduces the probability of recurrence at the surgical site from 30-40% to 15-20% after one year, according to data from scientific publications.
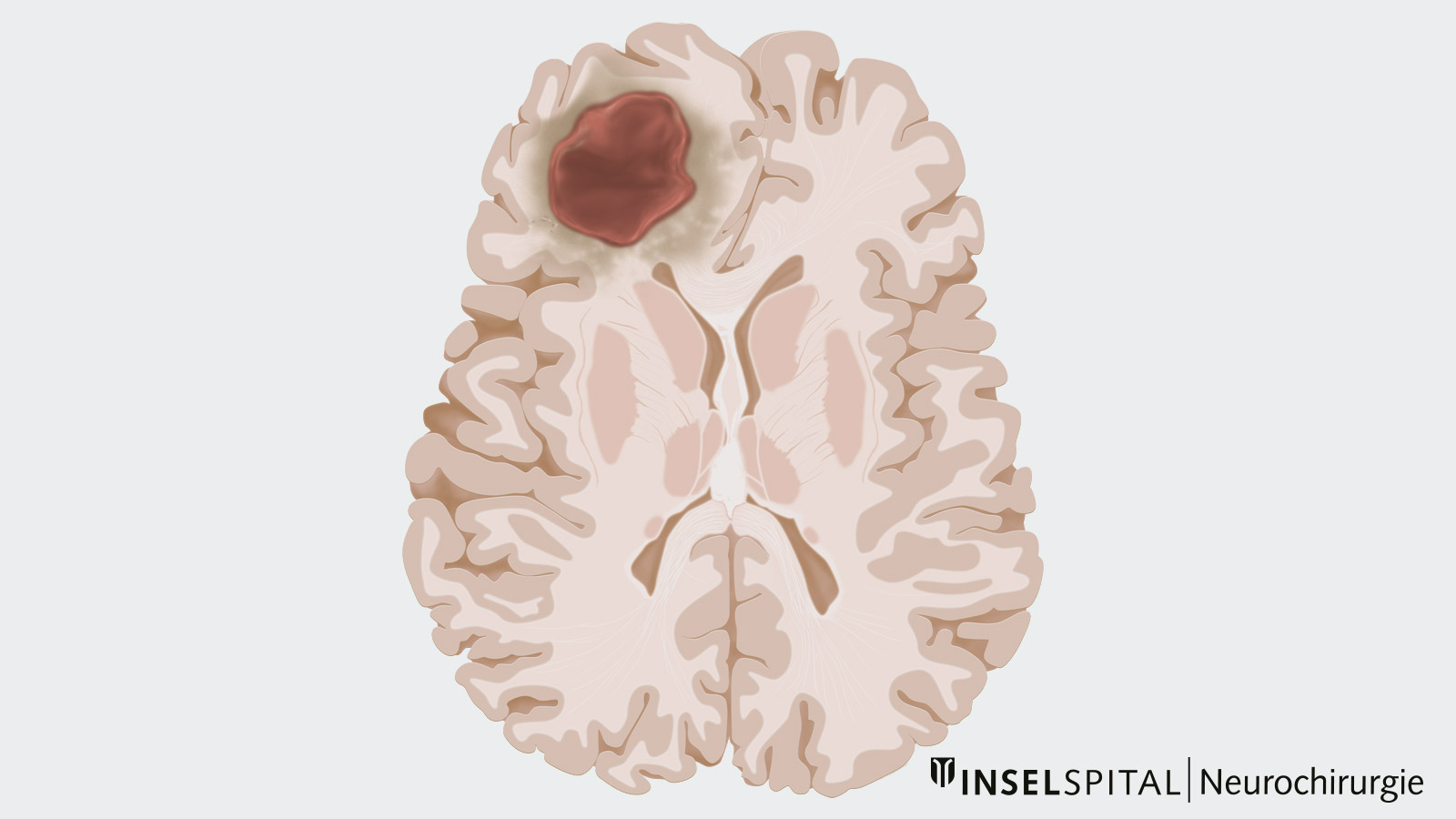
Complete microsurgical removal of a single metastasis can mean cure in a systemically tumor-free patient. The neurosurgical operation must be function-preserving and at the same time radical, i.e. the tumor should be completely removed. In addition, a minimally invasive procedure should be chosen as far as possible. Several technically innovative procedures are used to ensure maximum patient safety:
- intraoperative neuromonitoring and mapping (functional monitoring)
- neuronavigation
- fiber Tracking
- intraoperative imaging and advanced risk assessment including preoperative navigated transcranial magnetic stimulation (nTMS) before surgery
At Inselspital, we use various methods that allow us to safely surgically remove brain metastases. One example is preoperative navigated TMS examinations(nTMS) to localize the primary motor cortex. During surgery, this allows us to use motor evoked potentials (MEP) to closely monitor this motor center while locating important pathways such as the corticospinal tract (CST). Continuous feedback is made possible by the method of stimulation developed by us via our surgical instrument, known as dynamic mapping.
Multiple brain metastases
Surgery can also be performed on patients with multiple brain metastases if the patient is in good general condition and the systemic cancer is under control. As a rule, surgery is performed on 1 or 2 metastases that have exceeded the critical size of 3 cm. Additional small metastases are destroyed by radiosurgical treatment. Many patients are also treated by radiosurgery alone. Cases with more than 10 metastases and successful therapy have been reported.
Modern treatment strategies aim at combining the different therapies and delaying irradiation rather when treatment success with surgery and/or radiosurgery is likely. This is to reduce the incidence of mental deterioration after whole brain irradiation. We therefore work closely with our colleagues in oncology and radio-oncology to determine the best treatment for each individual patient.

Recurrent brain metastases – relapses
Also in case of recurrent brain metastases, a new surgical resection is often possible *, *. This is especially true in young patients in good general condition. Especially radiotherapy and radiosurgery can be applied a maximum of two times. In surgery, only the proximity of the important functional areas determines the possibility of re-treatment. Again, a personalized approach according to patient and tumor type applies.
Current guidelines for the treatment of brain metastases
The current guidelines for the treatment of brain metastases were published by the European Association of Neuro-Oncology in 2017 and provide a foundation in the interdisciplinary treatment of brain metastases.
Latest studies and therapies
A study from Italy published in 2018 investigated the resection of up to three brain metastases in one surgical procedure. The results of this study also show that patients with up to three brain metastases – provided that the underlying disease is controlled and the clinical condition is good – benefit from surgery. The side effect profile was acceptably low, and neurological outcome improved in nearly 60% of patients *.
All these modern therapy concepts are firmly integrated into the therapy decisions of our interdisciplinary neuro-oncological tumor board.
Can brain metastases be cured?
With neurosurgical operation and radiosurgery, procedures are available that enable effective treatment of local metastases. Whether patients can be cured depends mostly on whether the primary tumor can be controlled and cured and whether systemic spread of the cancer can be prevented. If these conditions are met, a patient with brain metastases can be cured.
Why you should seek treatment at Inselspital
The aim of the surgery of a brain metastasis is not only the complete removal, but also the application of a supramarginal surgical technique to prevent the metastasis from growing again. That is why the infiltration zone of the metastasis into the tissue is also removed during the surgery.
Equally important is the monitoring and protection of brain functions during this supramarginal resection. Our particular clinical and research focus at Inselspital is neurophysiological intraoperative monitoring. This allows us to achieve a rate of complete tumor removal with simultaneous preservation of function, that is among the highest in the published scientific literature.
-
Delattre J, Krol G, Thaler H, Posner J. Distribution of Brain Metastases. Archives of Neurology. 1988;45(7):741-744.
-
Schouten L, Rutten J, Huveneers H, Twijnstra A. Incidence of brain metastases in a cohort of patients with carcinoma of the breast, colon, kidney, and lung and melanoma. Cancer. 2002;94(10):2698-2705.
-
Al-Shamy G, Sawaya R. Management of brain metastases: the indispensable role of surgery. Journal of Neuro-Oncology. 2009;92(3):275-282.
-
Delattre J, Krol G, Thaler H, Posner J. Distribution of Brain Metastases. Archives of Neurology. 1988;45(7):741-744.
-
Johnson J, Young B. Demographics of Brain Metastasis. Neurosurgery Clinics of North America. 1996;7(3):337-344.
-
Posner J. Brain metastases: 1995. A brief review. Journal of Neuro-Oncology. 1996;27(3):287-293.
-
Cairncross JG, Posner JB. The management of brain metastases. In: Walker MD (ed) Oncology of the nervous system. (1983) Martinus Nijhof, Boston, 341–377
-
Kurtz J, Gelber R, Brady L, Carella R, Cooper J. The palliation of brain metastases in a favorable patient population: A randomized clinical trial by the radiation therapy oncology group. International Journal of Radiation Oncology*Biology*Physics. 1981;7(7):891-895.
-
Patchell R, Tibbs P, Walsh J, Dempsey R, Maruyama Y, Kryscio R et al. A Randomized Trial of Surgery in the Treatment of Single Metastases to the Brain. New England Journal of Medicine. 1990;322(8):494-500.
-
Vecht C, Haaxma-Reiche H, Noordijk E, Padberg G, Voormolen J, Hoekstra F et al. Treatment of single brain metastasis: Radiotherapy alone or combined with neurosurgery. Annals of Neurology. 1993;33(6):583-590.
-
Black P. Solitary Brain Metastases. Chest. 1993;103(4):367S-369S.
-
Weinberg J, Lang F, Sawaya R. Surgical management of brain metastases. Current Oncology Reports. 2001;3(6):476-483.
-
Arbit E, Wroński M, Burt M, Galicich J. The treatment of patients with recurrent brain metastases. A retrospective analysis of 109 patients with nonsmall cell lung cancer. Cancer. 1995;76(5):765-773.
-
Lohmann P, Kocher M, Ceccon G, Bauer E, Stoffels G, Viswanathan S et al. Combined FET PET/MRI radiomics differentiates radiation injury from recurrent brain metastasis. NeuroImage: Clinical. 2018;20:537-542.
-
Salvati M, Tropeano M, Maiola V, Lavalle L, Brogna C, Colonnese C et al. Multiple brain metastases: a surgical series and neurosurgical perspective. Neurological Sciences. 2018;39(4):671-677.
Further reading
- Raabe A, Beck J, Schucht P, Seidel K. Continuous dynamic mapping of the corticospinal tract during surgery of motor eloquent brain tumors: evaluation of a new method. Journal of Neurosurgery. 2014;120(5):1015-1024.
- Seidel K, Beck J, Stieglitz L, Schucht P, Raabe A. Low-Threshold Monopolar Motor Mapping for Resection of Primary Motor Cortex Tumors. Operative Neurosurgery. 2012;71(suppl_1):ons104-ons115.
- Seidel K, Beck J, Stieglitz L, Schucht P, Raabe A. The warning-sign hierarchy between quantitative subcortical motor mapping and continuous motor evoked potential monitoring during resection of supratentorial brain tumors. Journal of Neurosurgery. 2013;118(2):287-296.