Moyamoya disease is a rare disease of the cerebral vessels in which there is a slowly progressive narrowing or occlusion of the carotid artery and its main branches. As a result, bypasses of small blood vessels form that look like a cloud of fog on angiography – hence the name of the disease, which is derived from the Japanese "moyamoya" for fog. Patients suffering from the disease have a significant risk for stroke with potential neurological deficits. Neurosurgical treatment remains the only effective therapy.
Overview
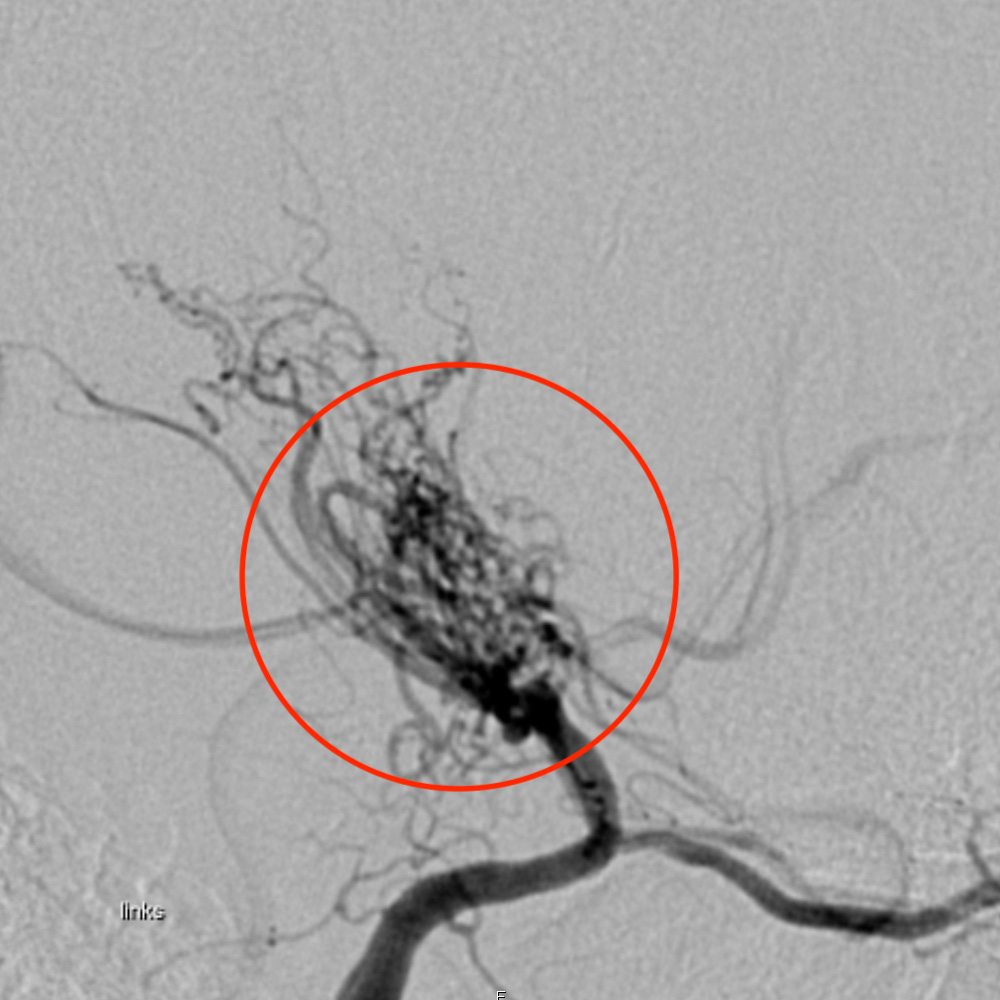
Moyamoya disease is a rare, non-inflammatory and non-atherosclerotic disease of the cerebral vessels. Its cause is still unknown. In the course of the disease, the inner vessel walls of the bilateral cerebral arteries increasingly thicken, mainly in the terminal intracranial part of the internal carotid artery (ICA), the middle cerebral artery (MCA) and the anterior cerebral artery (ACA). As a result, collateral vessels develop, forming a bypass circuit. * These small, abnormal and reticular collateral vessels are responsible for the characteristic appearance of the disease on cerebral digital subtraction angiography (DSA). The cloud-like appearance of these compensatory vessels gives the disease its name (from Japanese "moyamoya" = foggy).
The disease most commonly occurs on both sides, although the severity can vary per side. The term Moyamoya disease is reserved for this sometimes familial form in patients with vessels affected on both sides. In patients with unilateral expression, the condition is called Moyamoya syndrome. However, disease of the opposite side can also occur in Moyamoya syndrome in up to 40% of cases. *
How common is Moyamoya disease?
The cause of the disease is unknown, but the high incidence in Japan, where a familial cluster occurs in about 10–15% of patients, strongly suggests a genetic cause. * The disease is very rare overall, most commonly affecting children but also adults, typically between the ages of 30 and 50. The disease shows two age peaks and a clear female predominance, as women are affected almost twice as often as men. *, *, * The first age peak is around five years of age, with another peak in the fourth decade of life. The estimated incidence outside Japan is about 1 in 1,000,000 people. *
Several other medical conditions are associated with Moyamoya syndrome. These include *:
- Neurofibromatosis type 1
- Tuberous sclerosis
- Meningitis
- Systemic lupus erythematosus
- Sickle cell disease
- Fibromuscular dysplasia
- Down's syndrome
- Congenital heart disease
- Radiotherapy of the brain in childhood
Why do strokes occur?
The narrowing of the internal carotid artery leads to lower blood flow pressure in the brain, which can initially be compensated for by the formation of collateral vessels as well as reflex vasodilatation. As the disease progresses, it then eventually falls below the critical blood flow pressure, a process that can no longer be compensated for by the already exhausted compensatory mechanisms. The insufficient blood supply then leads to short stroke-like attacks, the so-called transient ischemic attacks (TIAs). These TIAs cause temporary neurological deficits, but can also lead to ischemic brain infarcts with permanent damage. Rupture of the collateral vessels can also lead to intracerebral hemorrhage.
How is Moyamoya disease diagnosed?
Diagnosis involves the detection of recurrent strokes. Magnetic resonance imaging (MRI) reveals the vascular changes typical for Moyamoya: narrowing of the internal carotid artery and collateral vessels. These results must then be confirmed by digital subtraction angiography (DSA), in which the vessels can be selectively visualized. It is essential to exclude the possibility that the strokes are not due to other causes, which would need to be treated differently.
In addition, it is important to prove that the blood flow to the brain is significantly restricted due to the vasoconstrictions. This evidence can be provided by several methods: magnetic resonance perfusion measurement, H2O positron emission tomography (H2O PET), SPECT examination (SPECT stands for Single Photon Emission Computed Tomography). Positron emission tomography (PET) is a diagnostic imaging technique that can effectively visualize pathological changes. At the end of 2020, the world's fastest PET-CT scanner was put into operation at the University Department of Nuclear Medicine at Inselspital. This scanner of the very latest technology enables excellent examination quality with shorter examination times and reduced radiation exposure for our patients.
What is the therapy for Moyamoya?
The progression of the disease can be very diverse. Regardless of whether disease progression is slow or rapid, the disease progresses in almost all symptomatic and also in asymptomatic patients if only drug therapy is used. *, *, * Scientific publications show that up to ⅔ of patients with symptomatic Moyamoya disease experience a relevant worsening of their symptoms within 5 years without surgery. *, *
Surgery significantly reduces this risk. About 96% of all operated patients do not have a stroke within 5 years after surgery. *, * Even in patients in whom Moyamoya disease does not yet cause symptoms, the annual risk of stroke (hemorrhagic or non-hemorrhagic) is 3.2%. *
Surgical methods
The aim of surgical therapy is to prevent strokes by improving blood flow (revascularization). Two methods of revascularization are available: direct revascularization and indirect revascularization.
Both methods can also be used in combination. Clinical studies generally show that direct revascularization is more effective than indirect revascularization. *, *, * However, the determination of the surgical technique is always an individual decision adapted to the patient, the symptoms and the clinic.
Direct revascularization
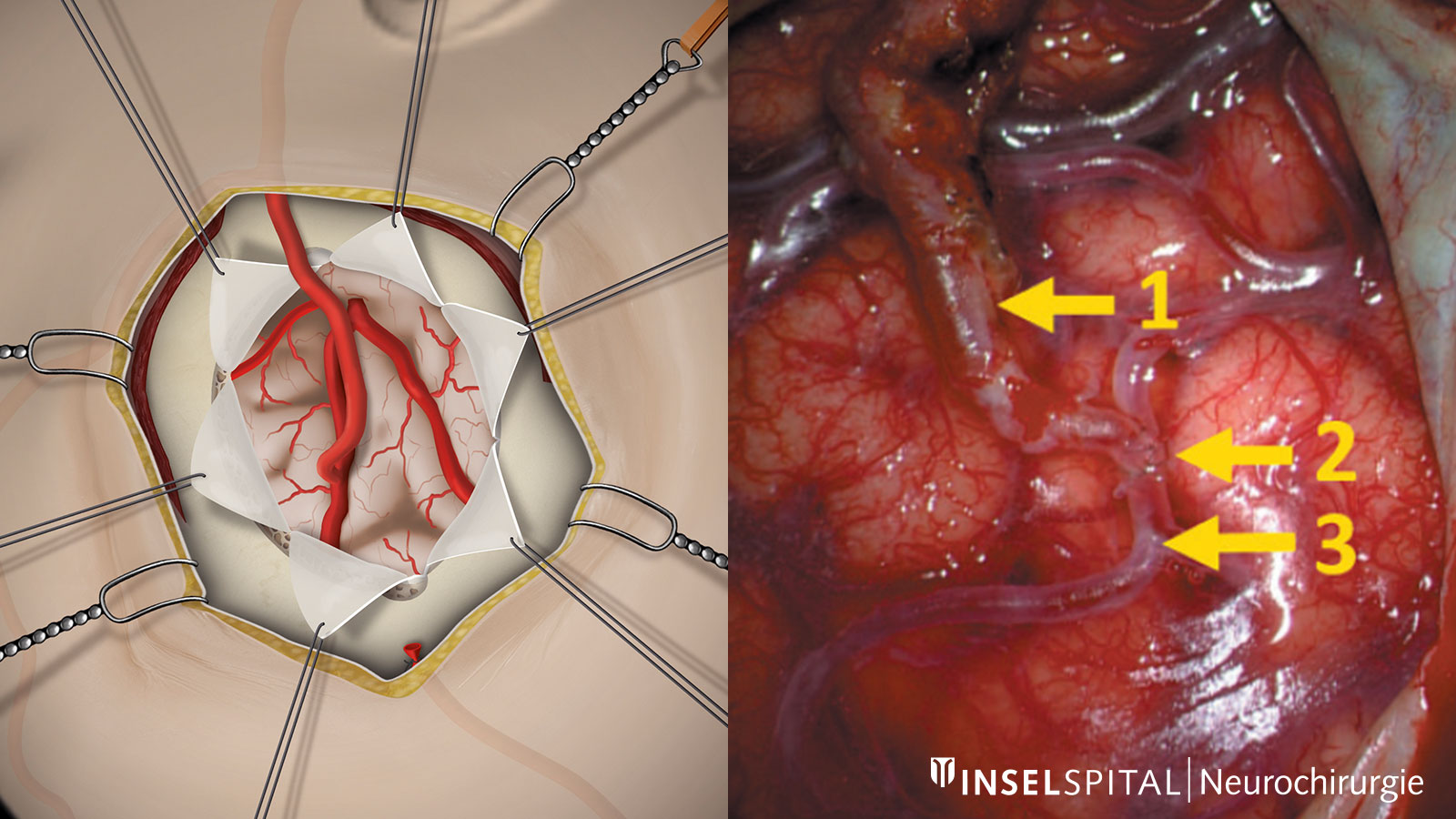
Direct revascularization creates a bypass circuit by directly connecting an extracranial artery to an artery on the surface of the brain. Through this so-called anastomosis, the narrowing of the diseased internal carotid artery can be bypassed and additional blood flow to the brain can be established. The most common operation of this type is the STA-MCA bypass (superficial temporal artery to middle cerebral artery bypass). In this procedure, the temporal artery (STA), which supplies the scalp and can often be felt on the side of the temple, is transplanted inwards through an opening in the skull and connected to a branch of the middle cerebral artery (MCA) running on the surface of the brain. The vessels are approx. 1–2 mm thick and are sutured under the microscope with a very thin thread.
Indirect revascularization
In indirect revascularization, tissue supplied by the external carotid artery is placed on the brain surface without suturing a direct vascular connection. Over time, the arteries from the tissue connect with the vessels on the brain surface and can thus also form a sufficient bypass circuit (neoangiogenesis). The tissues that can be used for this purpose include, above all, the hard meninges (encephalodurosynangiosis) and the temporalis muscle (encephalomyosynangiosis). The different variants of indirect revascularization are often used in combination with each other or in addition to direct bypasses. In general, indirect revascularization is used mainly in children up to puberty, as sufficient neoangiogenesis is more likely than in adults. *
Why you should seek treatment at Inselspital
At Inselspital we use state-of-the-art surgical techniques:
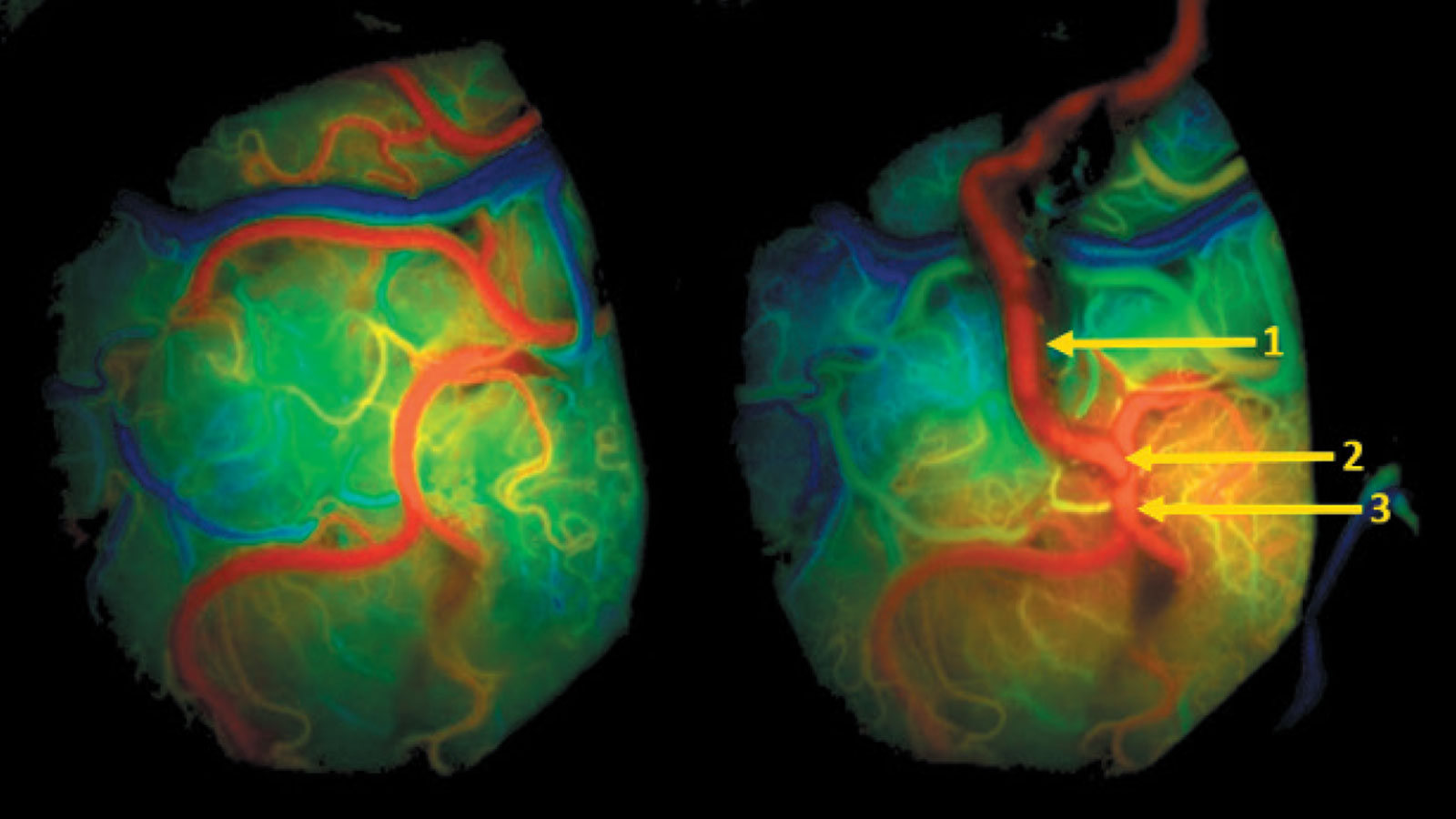
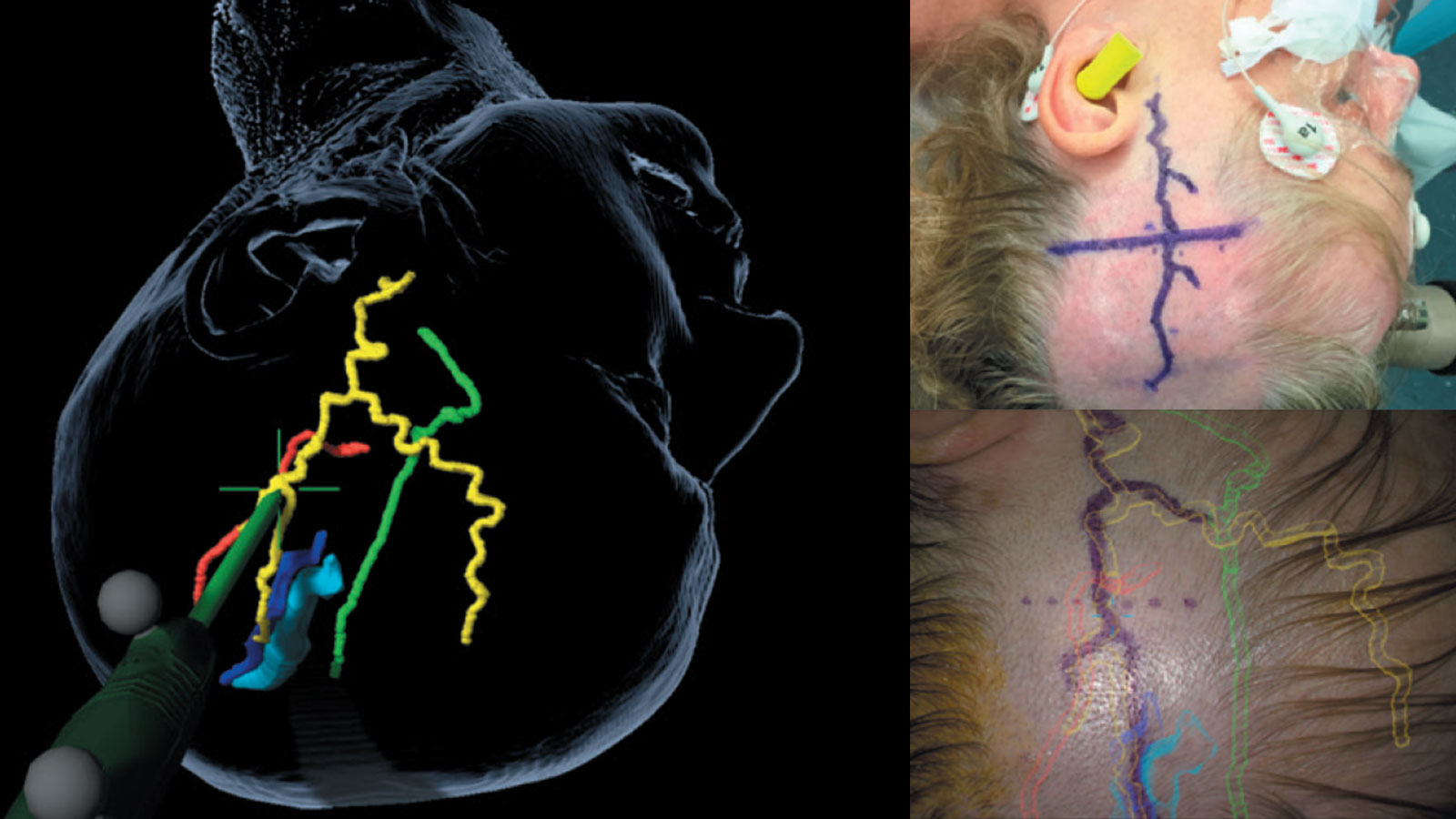
Vascular navigation and augmented reality can be used during surgery to increase accuracy and facilitate locating the donor vessel. Once the vascular anastomosis is completed, the patency of the vessels can be checked during surgery using indocyanine green infrared angiography (ICG infrared angiography for short) in an additional flow analysis.
-
Imaizumi T, Hayashi K, Saito K, Osawa M, Fukuyama Y. Long-Term Outcomes of Pediatric Moyamoya Disease Monitored to Adulthood. Pediatric Neurology. 1998;18(4):321-325.
-
Suzuki J. Cerebrovascular "Moyamoya" Disease. Archives of Neurology. 1969;20(3):288.
-
Kuroda S, Ishikawa T, Houkin K, Nanba R, Hokari M, Iwasaki Y. Incidence and Clinical Features of Disease Progression in Adult Moyamoya Disease. Stroke. 2005;36(10):2148-2153.
-
Choi J, Seok Kim D, Kim E, Lee K. Natural history of Moyamoya disease: comparison of activity of daily living in surgery and non surgery groups. Clinical Neurology and Neurosurgery. 1997;99:S11-S18.
-
Kurokawa T, Chen Y, Tomita S, Kishikawa T, Kitamura K. Cerebrovascular Occlusive Disease with and without the Moyamoya Vascular Network in Children. Neuropediatrics. 1985;16(01):29-32.
-
Scott R, Smith J, Robertson R, Madsen J, Soriano S, Rockoff M. Long-term outcome in children with moyamoya syndrome after cranial revascularization by pial synangiosis. Journal of Neurosurgery: Pediatrics. 2004;100(2):142-149.
-
Kuroda S, Hashimoto N, Yoshimoto T, Iwasaki Y. Radiological Findings, Clinical Course, and Outcome in Asymptomatic Moyamoya Disease. Stroke. 2007;38(5):1430-1435.
-
Suzuki J, Kodama N. Moyamoya disease--a review. Stroke. 1983;14(1):104-109.
-
Scott, R. and Smith, E., 2009. Moyamoya Disease and Moyamoya Syndrome. New England Journal of Medicine, 360(12), pp.1226-1237.
-
Kamada F, Aoki Y, Narisawa A, Abe Y, Komatsuzaki S, Kikuchi A et al. A genome-wide association study identifies RNF213 as the first Moyamoya disease gene. Journal of Human Genetics. 2010;56(1):34-40.
-
Baba T, Houkin K, Kuroda S. Novel epidemiological features of moyamoya disease. Journal of Neurology, Neurosurgery & Psychiatry. 2008;79(8):900-904.
-
Wakai K, Tamakoshi A, Ikezaki K, Fukui M, Kawamura T, Aoki R et al. Epidemiological features of Moyamoya disease in Japan: findings from a nationwide survey. Clinical Neurology and Neurosurgery. 1997;99:S1-S5.
-
Uchino, K., Johnston, S., Becker, K. and Tirschwell, D., 2005. Moyamoya disease in Washington State and California. Neurology, 65(6), pp.956-958.
-
Roach ES, Golomb MR, Adams R, et al. Management of stroke in infants and children: a scientific statement from a Special Writing Group of the American Heart Association Stroke Council and the Council on Cardiovascular Disease in the Young. Stroke; a journal of cerebral circulation 2008;39:2644-91.
-
Deng X, Gao F, Zhang D, Zhang Y, Wang R, Wang S et al. Direct versus indirect bypasses for adult ischemic-type moyamoya disease: a propensity score–matched analysis. Journal of Neurosurgery. 2018;128(6):1785-1791.
-
Komotar R, Starke R, Otten M, Merkow M, Garrett M, Marshall R et al. The role of indirect extracranial-intracranial bypass in the treatment of symptomatic intracranial atheroocclusive disease. Journal of Neurosurgery. 2009;110(5):896-904.
-
Mizoi K, Kayama T, Yoshimoto T, Nagamine Y. Indirect revascularization for moyamoya disease: Is there a beneficial effect for adult patients?. Surgical Neurology. 1996;45(6):541-548.
-
Rychen J, Goldberg J, Raabe A, Bervini D. Augmented Reality in Superficial Temporal Artery to Middle Cerebral Artery Bypass Surgery: Technical Note. Operative Neurosurgery. 2019;.
-
Raabe A, Nakaji P, Beck J, Kim L, Hsu F, Kamerman J et al. Prospective evaluation of surgical microscope—integrated intraoperative near-infrared indocyanine green videoangiography during aneurysm surgery. Journal of Neurosurgery. 2005;103(6):982-989.
-
Abla A, Gandhoke G, Clark J, Oppenlander M, Velat G, Zabramski J et al. Surgical Outcomes for Moyamoya Angiopathy at Barrow Neurological Institute With Comparison of Adult Indirect Encephaloduroarteriosynangiosis Bypass, Adult Direct Superficial Temporal Artery–to–Middle Cerebral Artery Bypass, and Pediatric Bypass. Neurosurgery. 2013;73(3):430-439.
-
Finkenstaedt S, Krejci V, Raabe A, Bervini D. Moyamoya-Erkrankung: Es braucht hoch-spezialisierte Zusammenarbeit. Anästhesie Journal 4/2019