Carotid artery stenosis is a narrowing of the carotid artery, usually caused by deposits on the vessel walls (atherosclerosis). There is a risk of blood clots and embolism in the brain. The treatment of carotid artery stenosis is therefore essential to prevent strokes and thus permanent disabilities. We at the Inselspital Bern have many years of experience in the treatment of carotid artery stenosis. Through the permanent further development of our intraoperative monitoring, we have succeeded in further increasing the safety of this operation.
Who is affected by carotid artery stenosis?
Carotid artery stenosis increases with age and affects about 7.5% of all men and about 5% of all women over the age of 80. * Apart from older age, other risk factors for vascular stenosis are: smoking, high blood pressure, diabetes and elevated blood lipid levels.
The risk of stroke is particularly high in patients who have already had a stroke caused by carotid artery stenosis or a short stroke-like attack (also called TIA, transient ischemic attack). These cases are called symptomatic carotid artery stenosis. Surgical removal of the atherosclerotic plaque in the carotid artery by means of a carotid endarterectomy significantly reduces the risk of stroke in these patients. *, * In patients with asymptomatic carotid artery stenosis, the risk of stroke can also be reduced by carotid endarterectomy in certain cases. *
What are the symptoms of carotid stenosis?
Atherosclerosis leads to deposits of cholesterol and fat particles, called plaque, on the inner walls of the vessels. If the inner wall of the carotid artery becomes narrowed, this is called carotid artery stenosis. This often remains asymptomatic for a long time – sometimes for years – and does not cause any symptoms. In these cases, the diagnosis is usually made as part of a pre-operative clarification for a planned operation, for example on the heart. Carotid artery stenosis can also be detected by a so-called flow noise above the carotid artery during a physical examination.
If the atherosclerotic plaque tears, tiny particles can break away from it, enter the brain with the bloodstream and trigger a TIA or stroke. Depending on the location of the blocked blood vessel, the symptoms can vary greatly. If the particles get into the ophthalmic artery, which supplies the retina of the eye with blood, a so-called amaurosis fugax or, in the worst case, a central artery occlusion with a deficient supply to the retina occurs. These manifest themselves clinically with a temporary or possibly also permanent loss of vision in the affected eye.
If the plaque particles reach the arteria cerebri media and its branches, there are disturbances of sensibility or motor function with weakness or slight paralysis. In the worst case, a carotid embolism can result in an extensive medial infarction with hemiplegia.
How is carotid artery stenosis diagnosed?
Radiological clarification and assessment of the degree of stenosis in patients with carotid artery stenosis are particularly important for assessing the risk of stroke and planning carotid endarterectomy. Duplex ultrasound, MRI angiography and CT angiography are available to us at the Inselspital Bern for this purpose.
The findings are then discussed in our interdisciplinary board together with colleagues from neuroradiology, neurology and vascular surgery. In this way, we jointly determine the optimal treatment strategy for each individual patient on an interdisciplinary basis.
Carotid endarterectomy
The operation is performed in several steps:
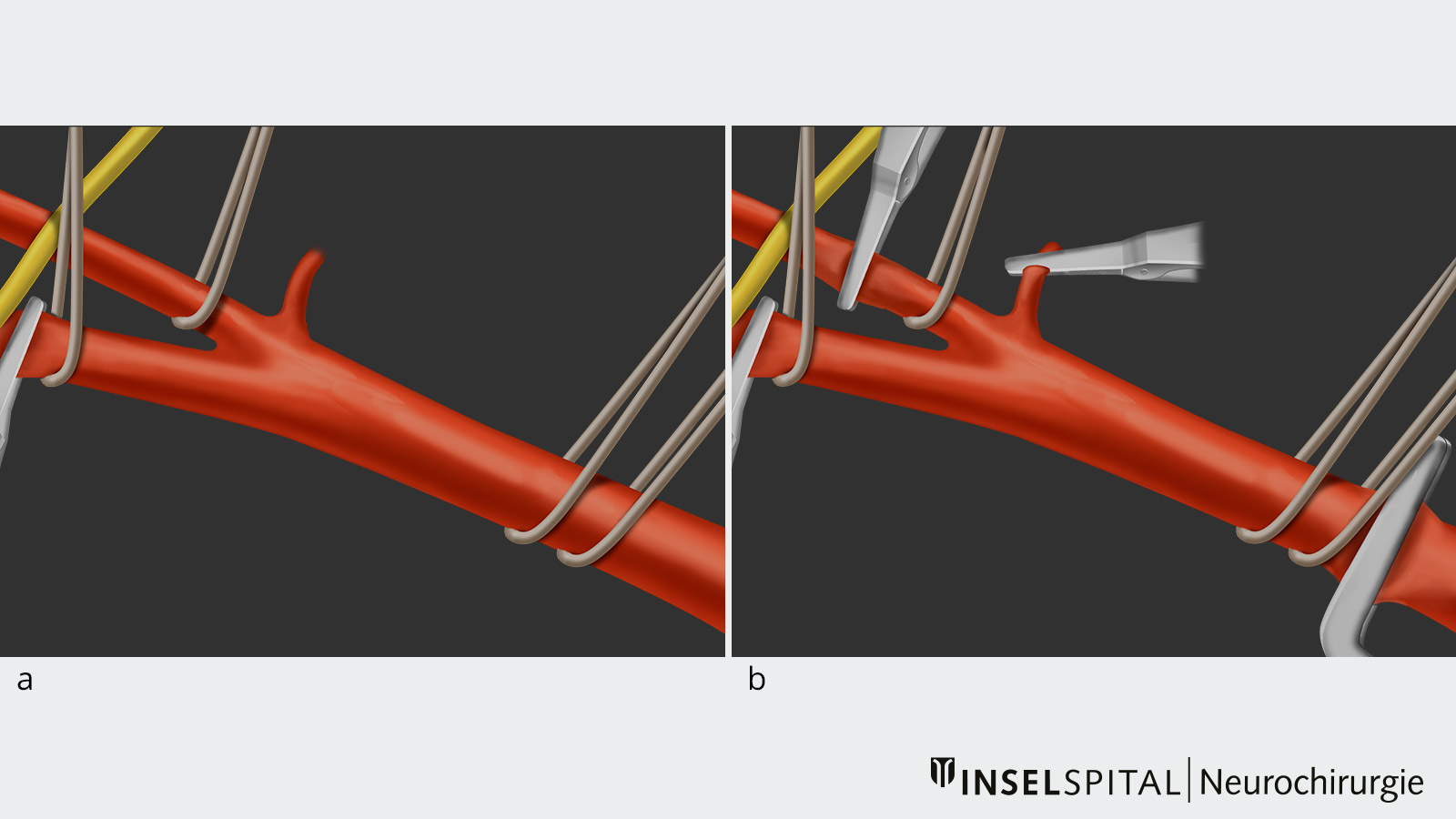
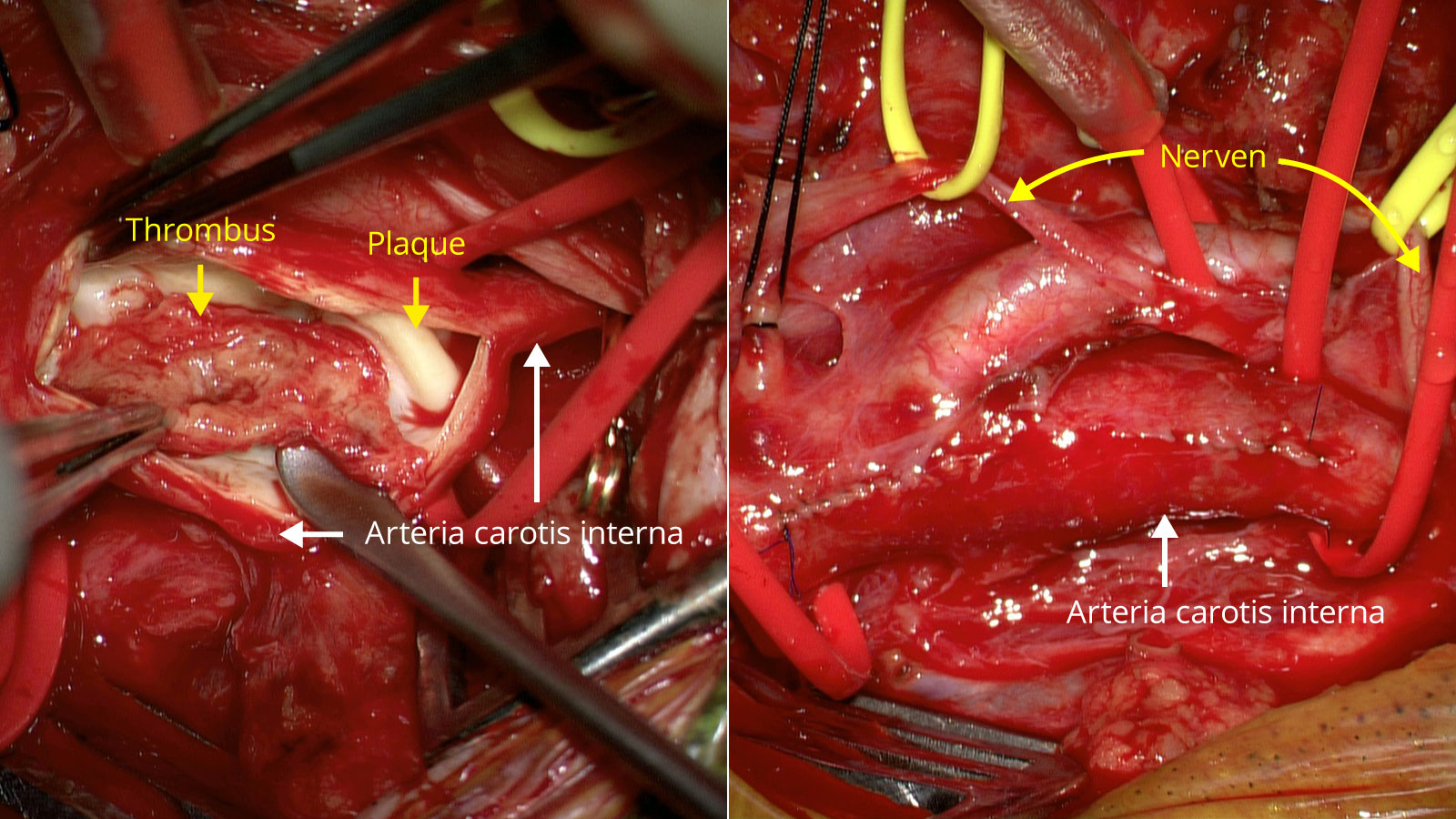
- In the first step of carotid endarterectomy, the neck arteries (common carotid artery, internal carotid artery and external carotid artery) are gently cleared.
- In a second step, these are individually wrapped with an elastic band so that the blood flow can be interrupted if necessary.
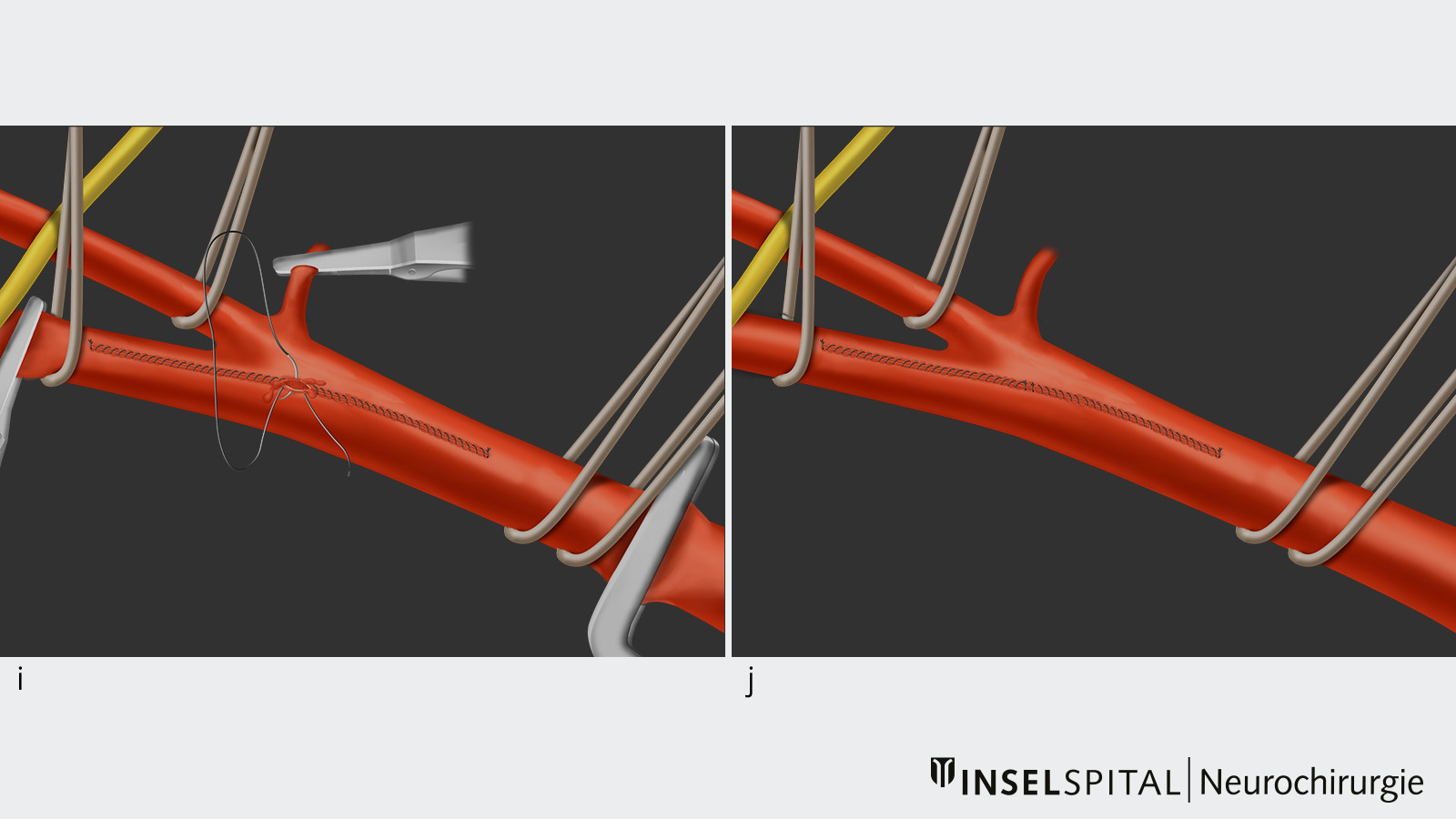
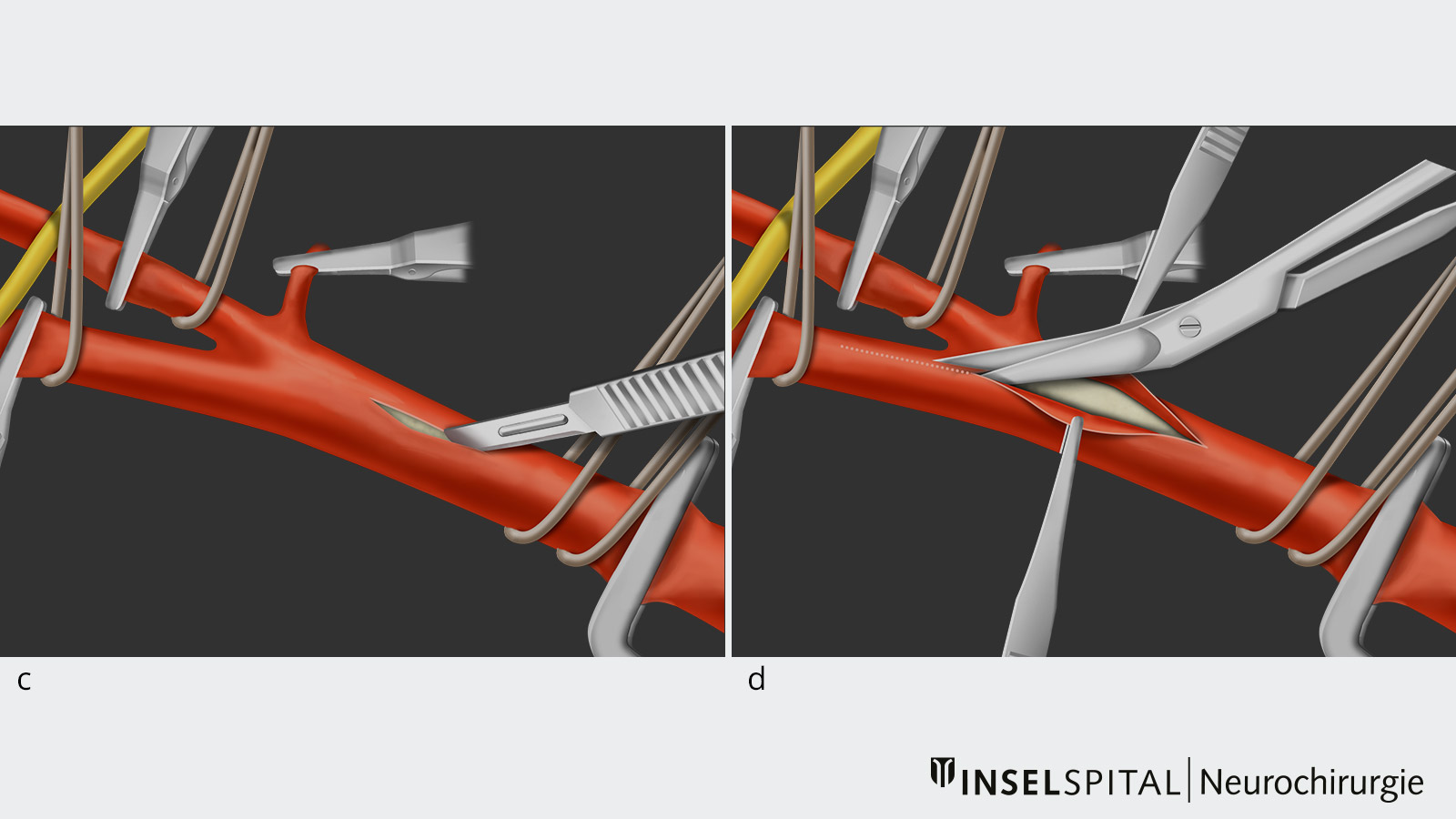
- In the next step, the clamping phase, the arteries are clamped one by one to interrupt the blood flow during the operation.
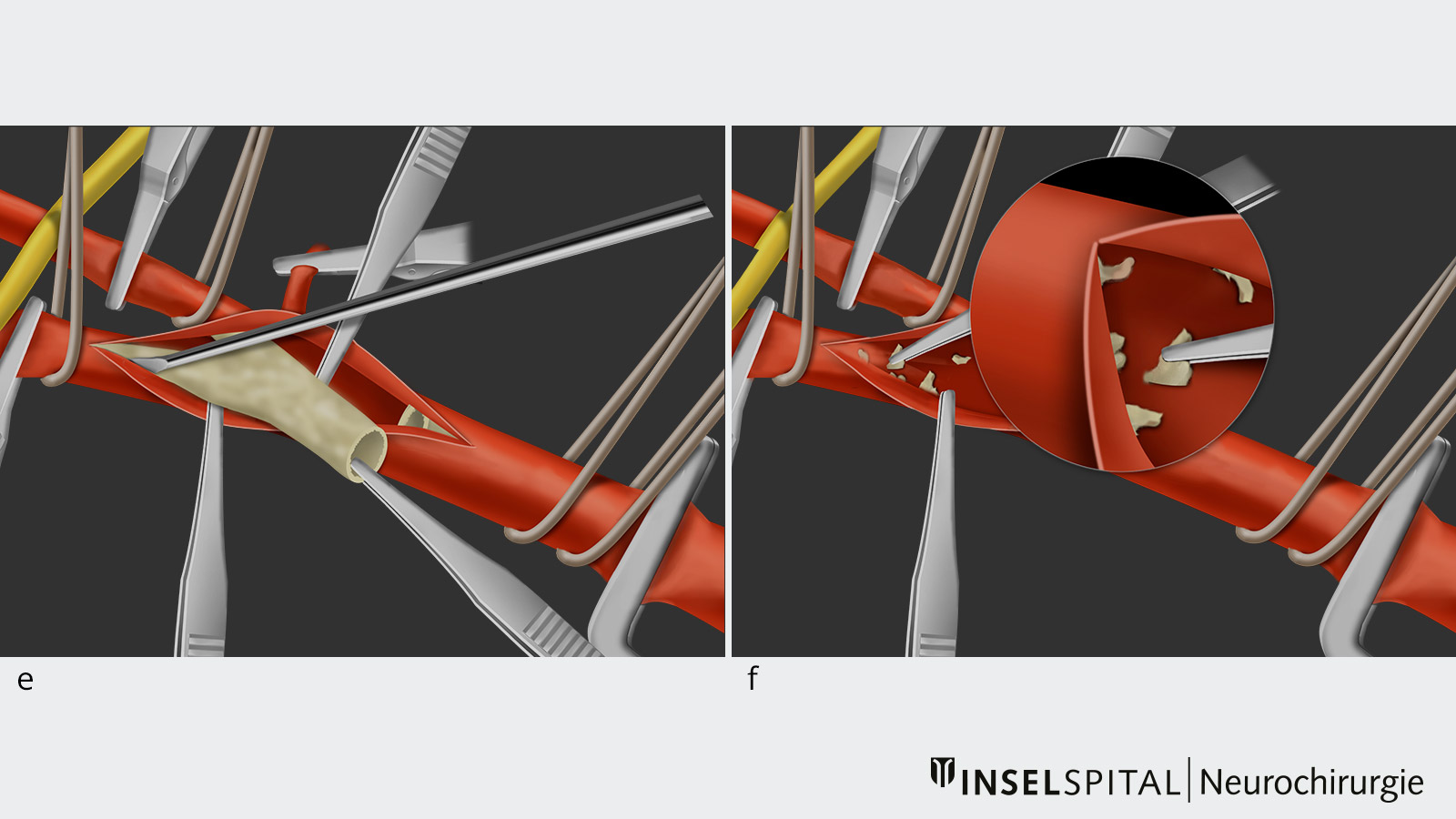
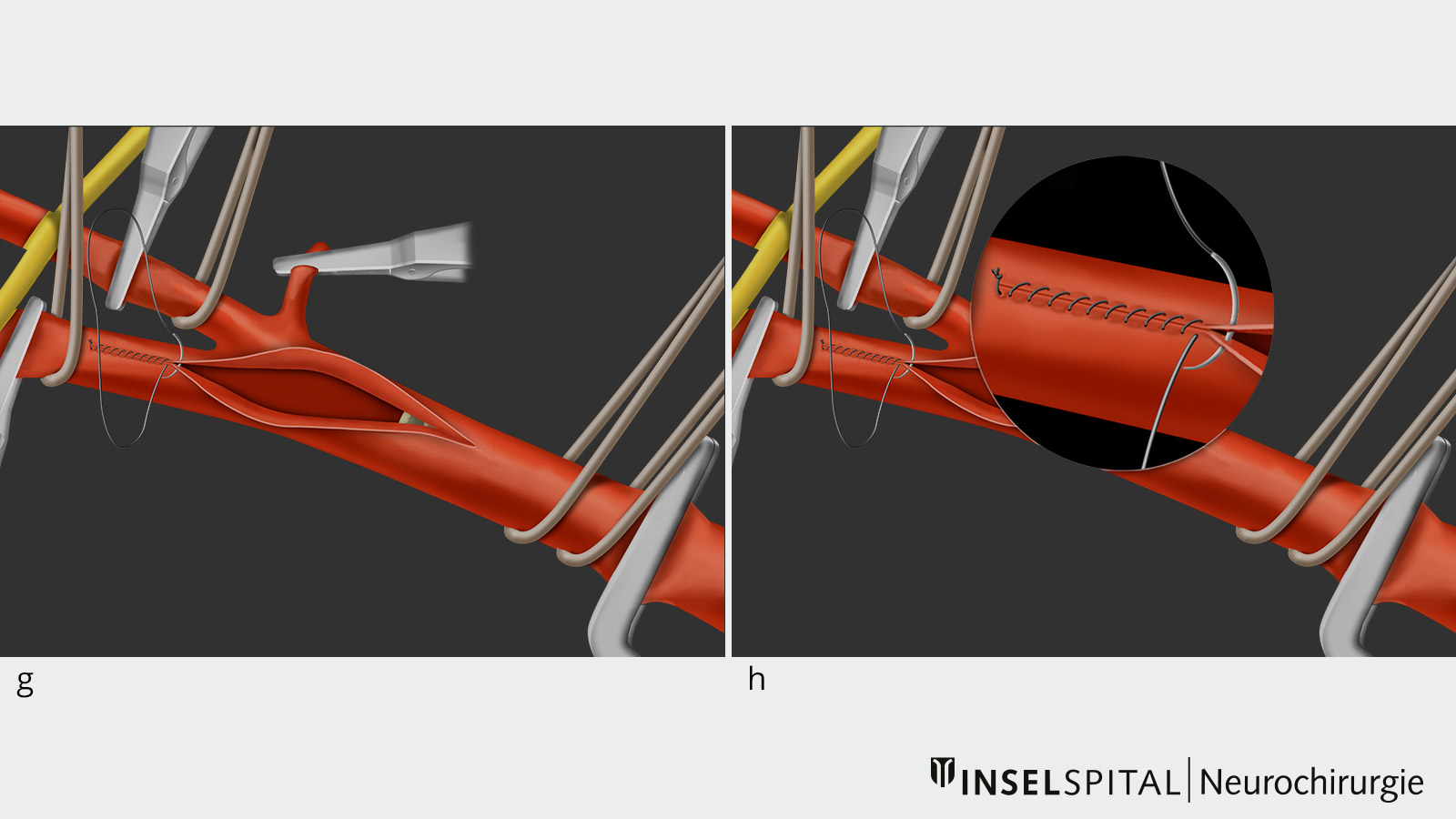
- This step allows the surgeon to make a longitudinal incision from the common carotid artery into the internal carotid artery and expose the atherosclerotic plaque inside the vessel, called the lumen.
- Subsequently, the atherosclerotic plaque is removed under the operating microscope with the help of microinstruments.
- Once the plaque has been completely removed, the vessel is closed again with a microsuture and vented.
- Afterwards, the blood flow can be restored by removing the vascular clamps.
- In a final step, the skin is closed again.
Neuromonitoring during carotid endarterectomy
At the Department of Neurosurgery of the Inselspital Bern, intraoperative neuromonitoring is standard practice throughout the operation and especially during the clamping phase. With the help of this monitoring, it can be ensured that the blood flow to the brain does not fall below a critical value due to the temporary clamping of the common carotid artery and the internal carotid artery. Should this nevertheless happen, a temporary bypass (shunt) is inserted into the arteries, which is removed again after the clamping phase is lifted.
Medical therapy
Medical therapy and control of cardiovascular risk factors (high blood pressure, diabetes mellitus, hypercholesterolemia, obesity, lack of exercise, smoking) play a decisive role in the treatment of carotid artery stenosis and are of great importance both before carotid endarterectomy and after the operation. This also includes therapy with platelet aggregation inhibitors such as aspirin or a similar drug, optimal adjustment of blood pressure and blood sugar, and lowering the lipid and cholesterol levels in the blood.
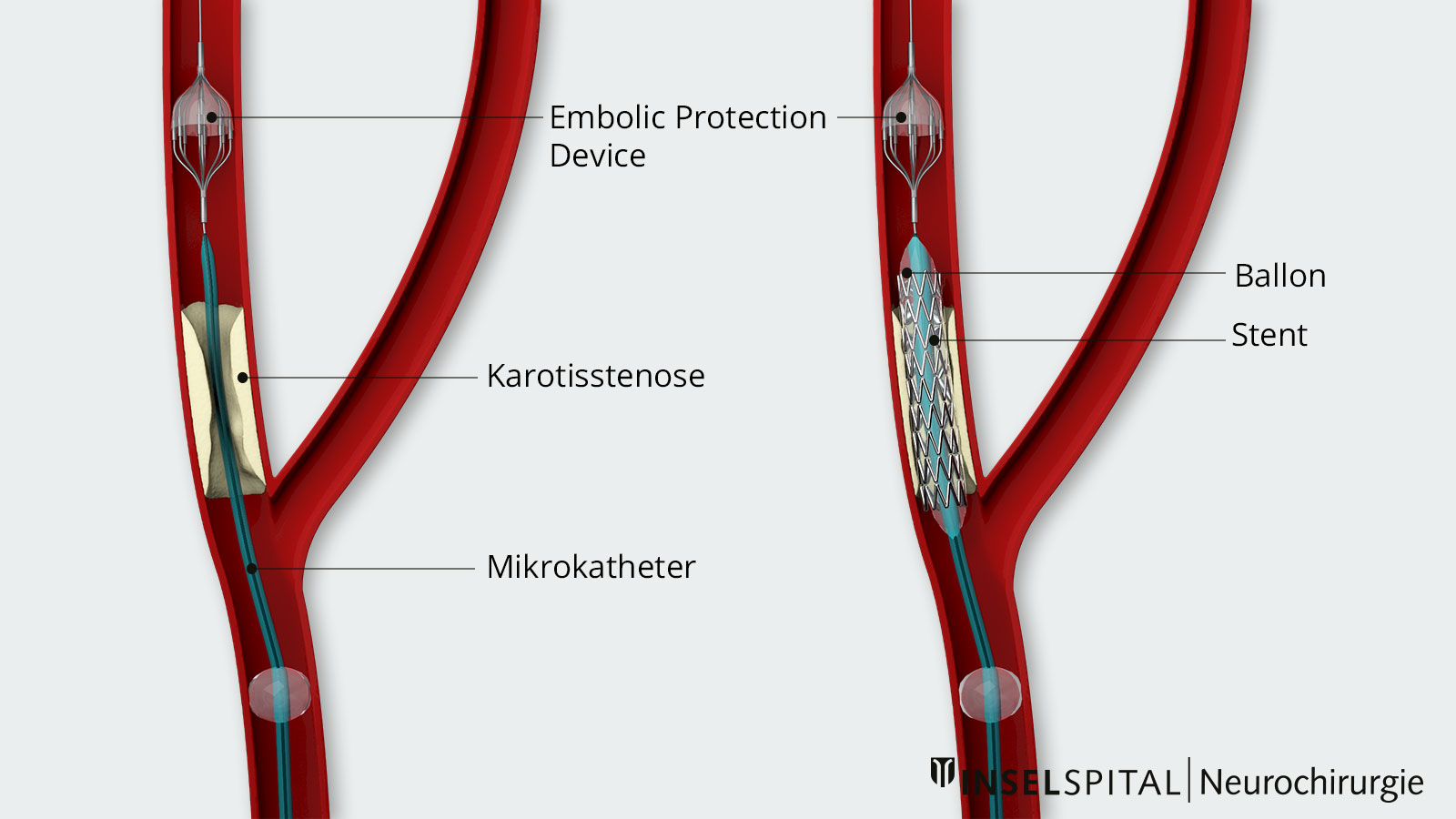
Carotid stent (endovascular treatment)
In certain cases, stenting can be offered as an alternative to carotid endarterectomy. This is an endovascular treatment in which a stent is inserted into the carotid artery by means of a catheter. The stent widens the existing narrowing and separates the plaque from the bloodstream. Various studies have shown that in many cases this treatment is associated with a higher risk of stroke and death than carotid endarterectomy. *, *, *, *, *
However, in individual patients who have an increased risk of surgery (e.g. after radiation in the area of the neck, pre-existing paresis of the recurrent nerve, etc.), stent dilatation is a less invasive treatment alternative than classic carotid endarterectomy.
Why you should seek treatment at Inselspital
In our clinic we perform about 100 carotid endarterectomies per year. The combined mortality and stroke rate before, during and after treatment is less than 3%. *
Intraoperative neuromonitoring, i.e. the monitoring of cerebral functions during surgery, is standard practice at the Department of Neurosurgery at Inselspital. Neuromonitoring makes a decisive contribution to the safety of our patients during surgery.
-
Sandercock PA, Warlow CP, Jones LN, Starkey IR. Predisposing factors for cerebral infarction: The oxfordshire community stroke project. BMJ. 1989;298:75-80
-
Barnett HJ, Taylor DW, Eliasziw M, Fox AJ, Ferguson GG, Haynes RB, et al. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North american symptomatic carotid endarterectomy trial collaborators. The New England journal of medicine. 1998;339:1415-1425
-
Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). The Lancet. 1998;351(9113):1379-1387.
-
Halliday A, Harrison M, Hayter E, Kong X, Mansfield A, Marro J, et al. 10-year stroke prevention after successful carotid endarterectomy for asymptomatic stenosis (acst-1): A multicentre randomised trial. The Lancet. 2010;376(9746):1074-1084.
-
Brott T, Hobson R, Howard G, Roubin G, Clark W, Brooks W et al. Stenting versus Endarterectomy for Treatment of Carotid-Artery Stenosis. New England Journal of Medicine. 2010;363(1):11-23.
-
Carotid Stenting Trialists C, Bonati LH, Dobson J, Algra A, Branchereau A, Chatellier G, et al. Short-term outcome after stenting versus endarterectomy for symptomatic carotid stenosis: A preplanned meta-analysis of individual patient data. Lancet. 2010;376:1062-1073
-
Mas JL, Chatellier G, Beyssen B, Branchereau A, Moulin T, Becquemin JP, et al. Endarterectomy versus stenting in patients with symptomatic severe carotid stenosis. The New England journal of medicine. 2006;355:1660-1671
-
Eckstein HH, Ringleb P, Allenberg JR, Berger J, Fraedrich G, Hacke W, et al. Results of the stent-protected angioplasty versus carotid endarterectomy (space) study to treat symptomatic stenoses at 2 years: A multinational, prospective, randomised trial. The Lancet. Neurology. 2008;7:893-902
-
Muller MD, Lyrer P, Brown MM, Bonati LH. Carotid artery stenting versus endarterectomy for treatment of carotid artery stenosis. The Cochrane database of systematic reviews. 2020;2:CD000515
-
Reinert M, Mono M, Kuhlen D, Mariani L, Barth A, Beck J et al. Restenosis after microsurgical non-patch carotid endarterectomy in 586 patients. Acta Neurochirurgica. 2011;154(3):423-431.