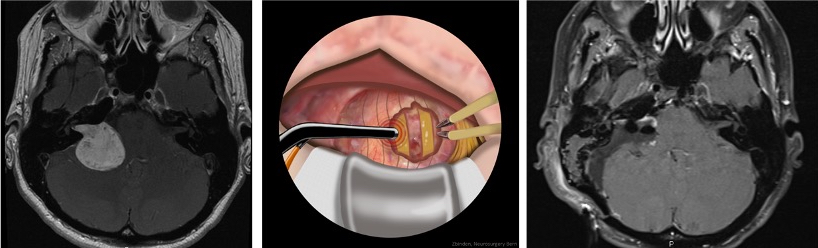
During tumor surgery on the brainstem and skull base, important functional centers and the cranial nerves are in close proximity. Therefore, specialized monitoring procedures are particularly crucial in these areas.
Which brain functions are monitored?
During surgery, we use specialized procedures to monitor the activity of muscles controlled by certain cranial nerves. Routine procedures include monitoring free electromyogram (EMG) and motor evoked potentials (MEP) from cranial nerves such as the facial nerve, the glossopharyngeal nerve, or the vagus nerve, which affect many bodily functions *,*.
In addition, we can specifically localize the motor cranial nerves during the operation. This is called mapping. It allows us to determine important functional areas in the brain or near the tumor in real time.
For tumors that are located deep inside the brain, we search the surface of the brain directly to find the best and safest point for access to the tumor. This allows us to minimize the risk to the patient.
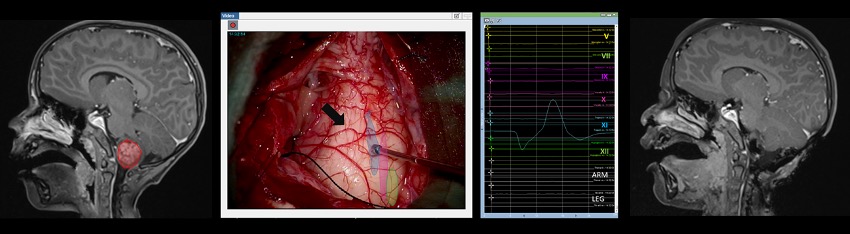
In addition to monitoring motor functions (MEP), we can also measure sensory and sensory information during the operation. To do this, we use procedures such as somatosensory evoked potentials (SEP) for the nerve pathways, auditory evoked potentials (AEP) for the hearing or visual evoked potentials (VEP) for the optic nerves.
In addition, we are actively working on the development of new methods to better monitor the complex neural connections in the brainstem. This includes intraoperative monitoring of reflexes such as:
- blink reflex *, which indicates the protective function of the eyes,
- H-reflex of the masseter *, which checks important chewing nerves,
- and laryngeal adduction reflex *, which measures the function of the laryngeal nerves.
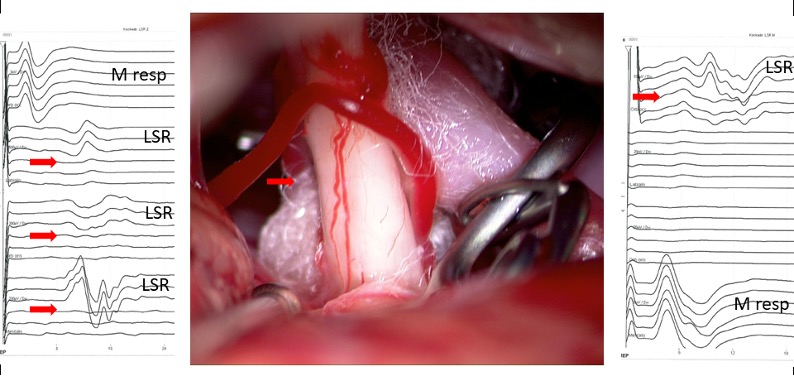
A special form of neuromonitoring is used for patients suffering from hemifacial spasm – an involuntary twitching of the facial muscles. During surgery, success can be verified directly by performing the lateral spread response (LSR) test on the facial nerve (nervus facialis) *. If the overactive muscle responses in the EMG (electromyogram) disappear, this indicates that the operation was successful and the patient is cured.
All these procedures help us to protect nerve pathways and reflexes during brainstem or skull base surgeries, thus minimizing the risk to the patient.
-
Fernandez-Conejero I, Deletis V. Transcranial electrical stimulation and monitoring. Journal of neurosurgery 2014;120:291-292.
-
Dong CC, Macdonald DB, Akagami R, et al. Intraoperative facial motor evoked potential monitoring with transcranial electrical stimulation during skull base surgery. Clinical neurophysiology. 2005;116:588-596.
-
Deletis V, Urriza J, Ulkatan S, Fernandez-Conejero I, Lesser J, Misita D. The feasibility of recording blink reflexes under general anesthesia. Muscle & nerve. 2009;39:642-646.
-
Ulkatan S, Jaramillo AM, Tellez MJ, Goodman RR, Deletis V. Feasibility of eliciting the H reflex in the masseter muscle in patients under general anesthesia. Clinical neurophysiology. 2017;128:123-127.
-
Sinclair CF, Tellez MJ, Tapia OR, Ulkatan S, Deletis V. A novel methodology for assessing laryngeal and vagus nerve integrity in patients under general anesthesia. Clinical neurophysiology. 2017;128:1399-1405.
-
Fernandez-Conejero I, Ulkatan S, Sen C, Deletis V. Intra-operative neurophysiology during microvascular decompression for hemifacial spasm. Clinical neurophysiology. 2012;123:78-83.
