Two methods – one goal
We combine state-of-the-art technology with expert knowledge to sustainably increase patient safety at the Inselspital during operations on the brain or spinal cord. By combining monitoring and localization methods (mapping), postoperative deficits such as paralysis in our patients can be significantly reduced. Our Department of Neurosurgery is a specialized center for this type of surgery.
What is monitoring?
During monitoring, a known functional location is continuously stimulated and measured to see if the signal is transmitted normally along the entire motor pathway. To do this, a monitoring electrode is placed directly on the motor center. A so-called train-of-five impulse is continuously set with a microcurrent via this. This triggers a single movement impulse, which is received in the target muscle with a special needle electrode. Triggering the impulse in the brain and receiving it in the target muscle indicates an intact and functioning motor pathway.
What is mapping?
In contrast, during mapping, the location of the function is unknown. This is the case for most operations below the cerebral cortex. With the help of a special probe, the surgical area is specifically stimulated with a microcurrent and scanned to see if an invisible function is hidden there. If the surgeon comes close to a function, he is warned with an alarm to avoid operating in this area.
This method of dynamic mapping was developed by our working group at Inselspital.
Continuous monitoring during operations on the motor center
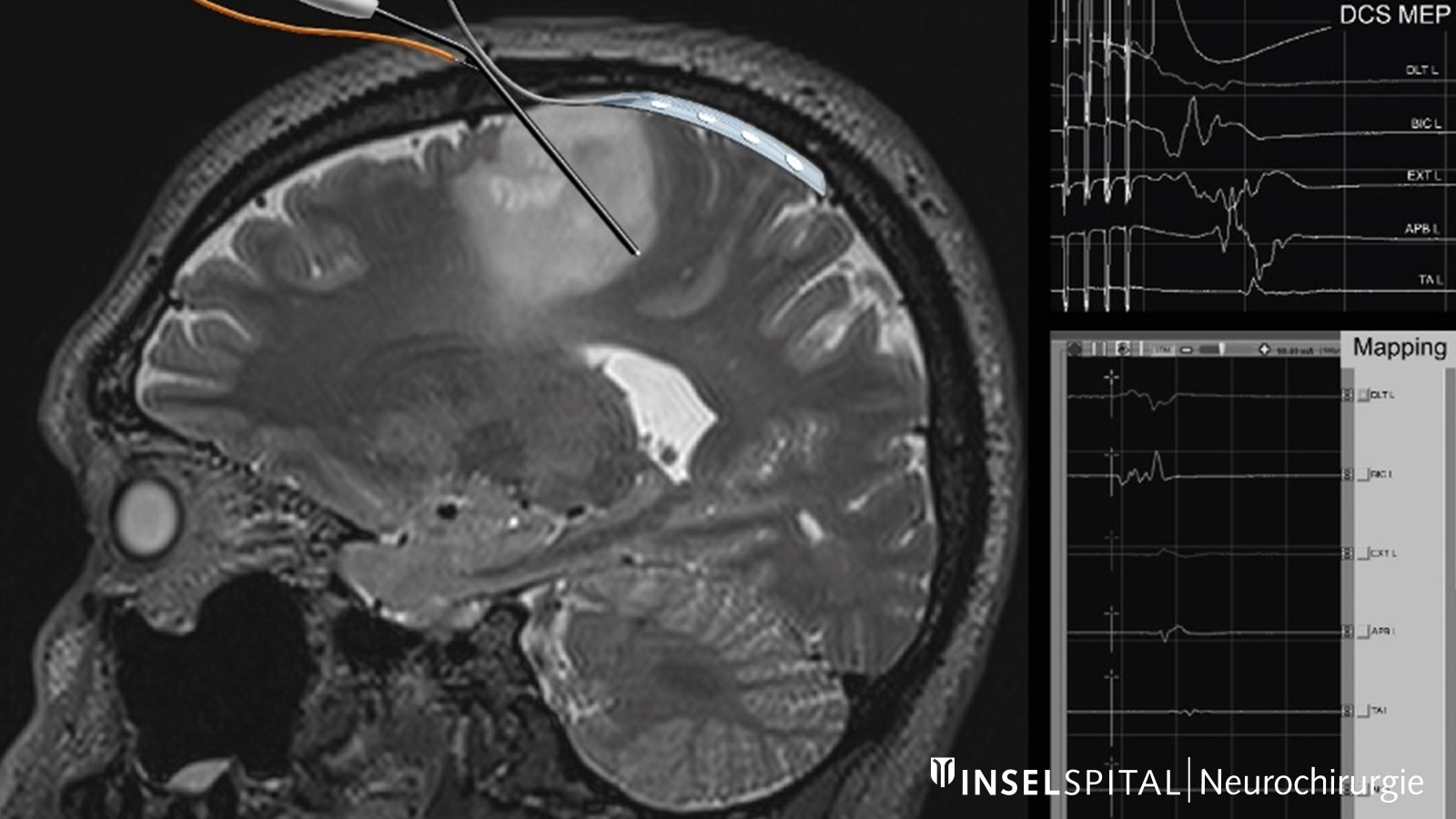
Motor evoked potentials (MEP) are used to monitor motor function and muscle strength during surgery in the vicinity of the precentral brain, the pyramidal tract and the spinal cord. In this process, nerve connections are activated and the electrical potentials are measured either through the skin using special electrodes (transcranial electrical stimulation, TES) or directly on the brain surface using strip electrodes (direct cortical stimulation, DCS) *, *.
Changes in these potentials serve as important warning signals for the surgeon and lead to an adjustment of the surgical procedure in order to significantly reduce the risk of damage to motor functions. This procedure is well established in our neurosurgical clinic at the Inselspital and is used in particular for tumor operations * and brain aneurysm operations *.
Our team has already published several scientific articles on this topic in international journals and presented them at international conferences.
Continuous dynamic mapping during operations on the motor center
The exact location in the brain of an important function such as motor function is often displaced by the tumor and is not visible to the naked eye. These factors mean that the rate of postoperative paralysis after tumor removal with conventional mapping and monitoring is still around 10%. With our development and introduction of special continuous dynamic mapping, we were able to reduce this rate to 3–5% *.
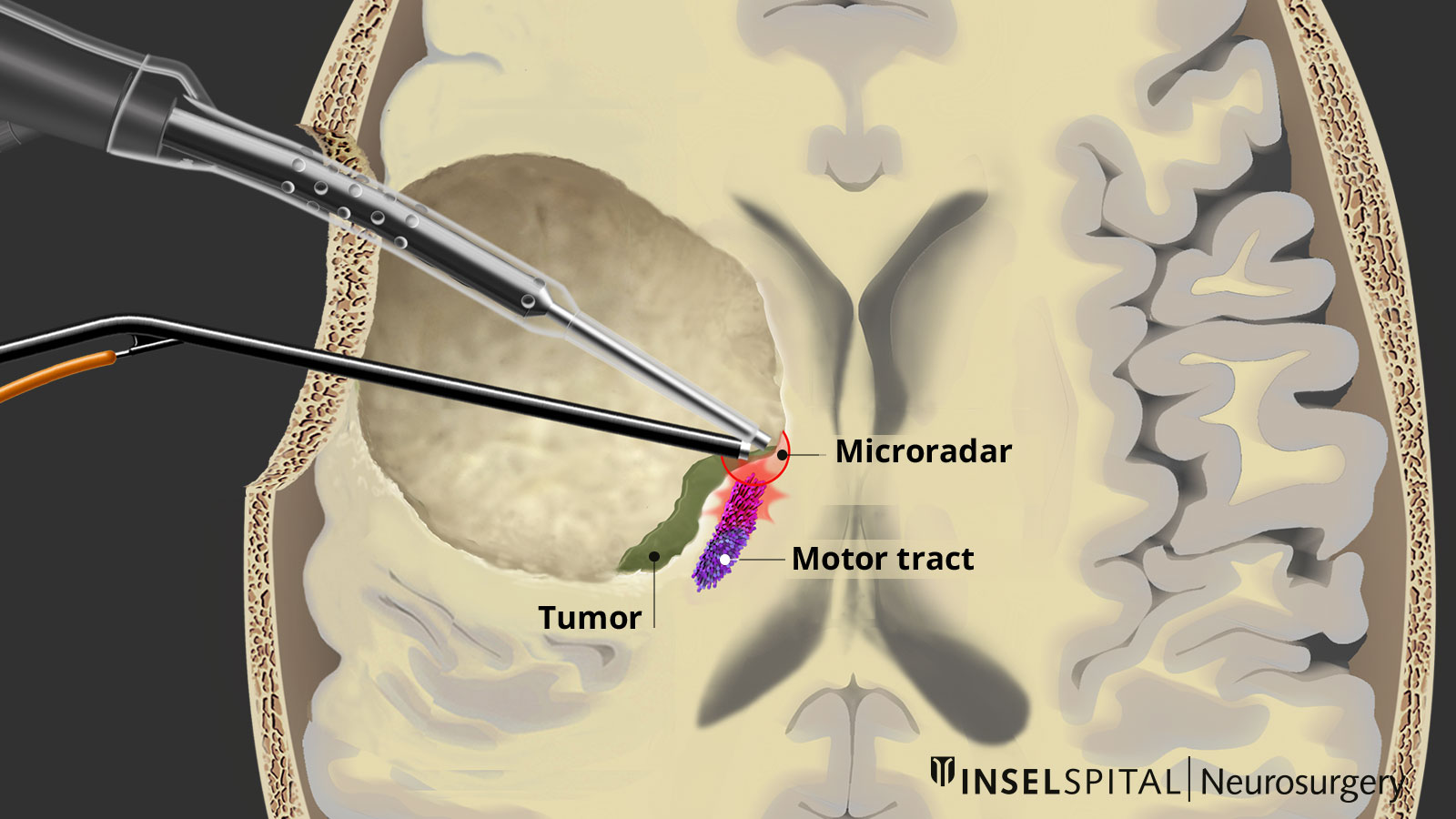
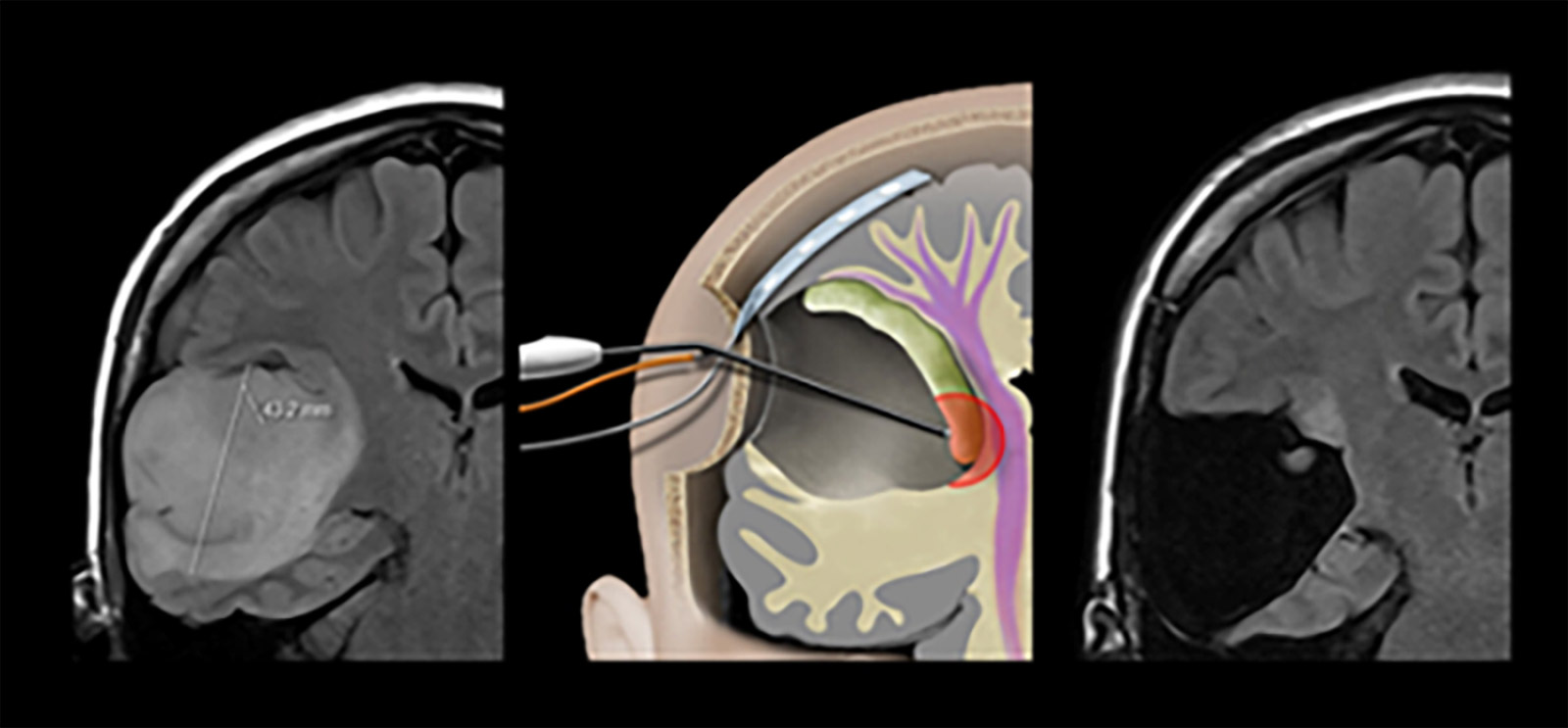
To achieve this, we have developed a tool that enables continuous subcortical stimulation without interrupting the surgical procedure of tumor removal. To do this, we integrated a stimulation probe into a classic surgical suction device. * The classic surgical suction cup can be connected to a stimulation cable at its shaft. Only the tip conducts the current, thus becoming a monopolar mapping probe. A positive MEP response is indicated by an audible tone, providing real-time feedback to the surgeon.
Study results on the safety and reliability of continuous dynamic mapping
In one study, we were able to demonstrate the safety and reliability of the method in tumors in highly sensitive brain regions. The rate of permanent motor deficits was only 3%, due to vascular and not mechanical damage to the pyramidal tract *.
In another study of glioblastomas, the results showed complete resection of contrast-enhancing tumor (CET) in 69% of cases and a permanent deficit rate of 4%, also due to vascular lesions, despite the proximity of the tumor to the pyramidal tract *.
The mini-suction device can be integrated into the surgical instrument, enabling continuous mapping to be used during all surgically important steps, including subpial dissection and hemostasis *, *, *, *.
-
Seidel K, Beck J, Stieglitz L, Schucht P, Raabe A. The warning-sign hierarchy between quantitative subcortical motor mapping and continuous motor evoked potential monitoring during resection of supratentorial brain tumors. Journal of neurosurgery 2013;118:287-296.
-
Landazuri P, Eccher M. Simultaneous Direct Cortical Motor Evoked Potential Monitoring and Subcortical Mapping for Motor Pathway Preservation During Brain Tumor Surgery: Is it Useful? Journal of clinical neurophysiology : official publication of the American Electroencephalographic Society 2013;30:623-625.
-
Raabe A, Seidel K. Prevention of ischemic complications during aneurysm surgery. Journal of neurosurgical sciences 2016;60:95-103.
-
Raabe A, Beck J, Schucht P, Seidel K. Continuous dynamic mapping of the corticospinal tract during surgery of motor eloquent brain tumors: evaluation of a new method. Journal of neurosurgery 2014;120:1015-1024.
-
Schucht P, Seidel K, Beck J, et al. Intraoperative monopolar mapping during 5-ALA-guided resections of glioblastomas adjacent to motor eloquent areas: evaluation of resection rates and neurological outcome. Neurosurgical focus 2014;37:E16.
-
Schucht P, Beck J, Seidel K, Raabe A. Extending resection and preserving function: modern concepts of glioma surgery. Swiss medical weekly 2015;145:w14082.
-
Schucht P, Seidel K, Jilch A, Beck J, Raabe A. A review of monopolar motor mapping and a comprehensive guide to continuous dynamic motor mapping for resection of motor eloquent brain tumors. Neuro-Chirurgie 2017;63:175-180.

