The simulation workshop for intracranial aneurysm microsurgery is being held in Bern for the second time. During this 2-day course on May 14/15, 2024, prospective or completed neurosurgeons can apply and deepen their skills in the field of aneurysm surgery. This innovative workshop will be led by Prof. David Bervini, senior physician and specialist in vascular neurosurgery at Inselspital. The venue is the SITEM, Freiburgstrasse 3 in Bern.
Aneurysm operations are demanding and difficult procedures. A surgeon needs a lot of training and experience to choose the right type of procedure and to plan the path to the aneurysm safely and precisely. This makes it all the more important that every move during the operation on the blood vessel is perfect. At the 2nd Hands-on Aneurysm Clipping Course, this can be practiced in numerous practical exercises on the surgical simulator.
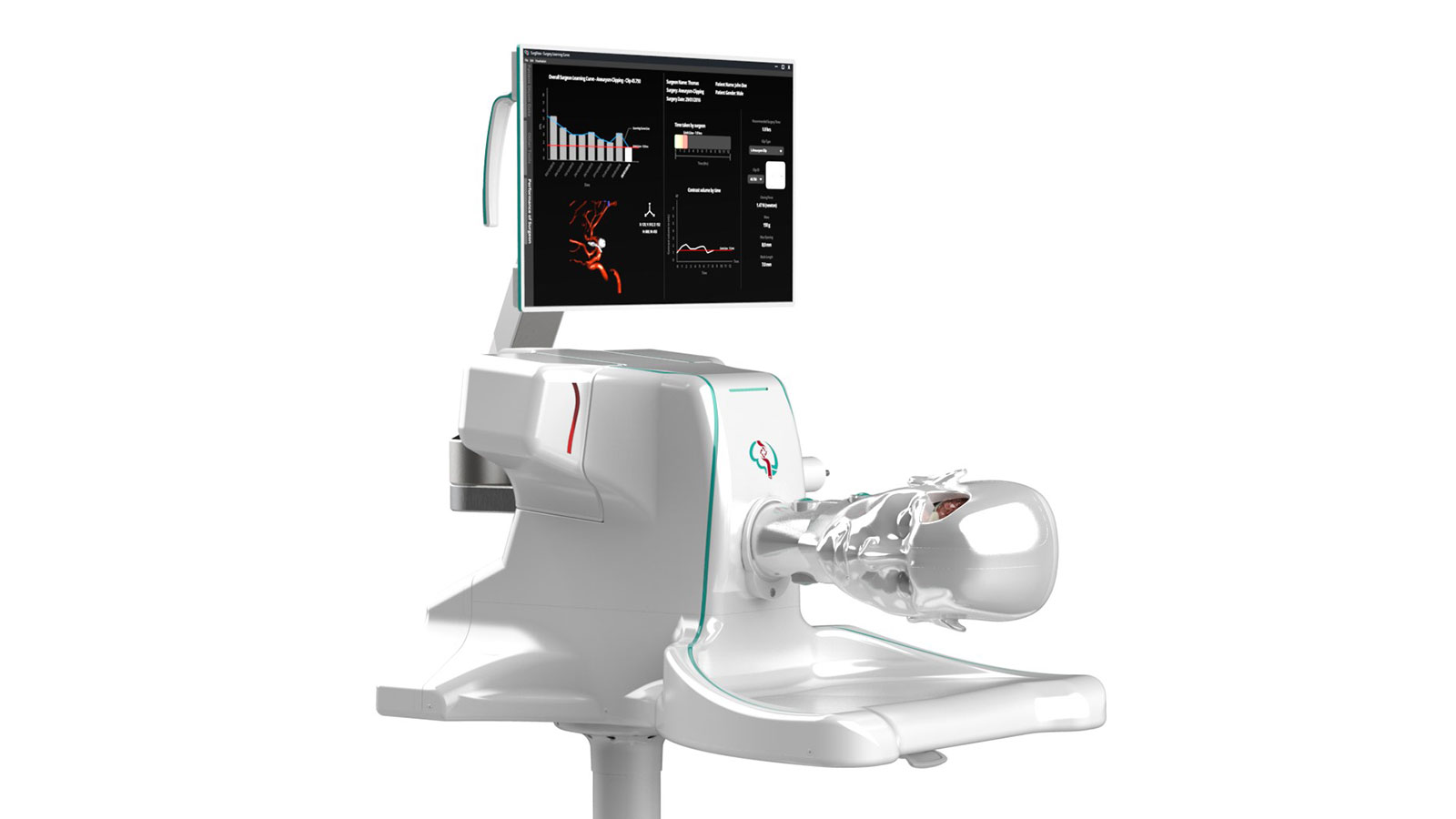
The innovative 4D aneurysm simulator was developed at Inselspital in collaboration with the University of Bern and has brought about a breakthrough in aneurysm surgery in terms of risk minimization and patient safety. Its development was supported by the Swiss innovation promotion agency Innosuisse, the Swiss Heart Foundation, the medical technology company Ypsomed and the start-up funding program Venture Kick.
Interview
As part of the first simulation workshop, we conducted an interview with Prof. David Bervini, which explains the concept and aim of the workshop for interested doctors.
Prof. Bervini, why are aneurysm operations so dangerous?
Bervini: Around 2 to 3 out of 100 adults have an aneurysm – very often without feeling it. Aneurysms are balloon-like dilatations of a cerebral artery that can rupture and cause severe cerebral bleeding. Their neurosurgical removal is extremely challenging. It is therefore essential to carefully weigh up the risk of rupture against the risks of surgery.
Aneurysm operations are particularly delicate because they involve sensitive anatomical structures that are often difficult to access in the brain and also differ from patient to patient. The slightest error or misjudgment can drastically complicate the surgical procedure and lead to serious and potentially catastrophic neurological complications. Minimizing the risks of such a procedure is therefore a top priority.
What exactly does the 4D aneurysm simulator do?
Bervini: The simulator offers a realistic, individualized, visual and haptic training opportunity on a 3D copy of a patient's skull, brain and now also blood vessels. In the simulator, surgeons find themselves in a 1:1 situation that they will later encounter during a real operation.
The extension to a 4D simulation, in which the temporal aspects of blood vessels with pulse and blood flow are also correctly simulated, is unique in the world. The 4D simulator is used both for planning an operation and for real-time exercises on actual cases. By perfecting the planning and practice of a procedure in this way, the surgical risk for patients is significantly reduced.
Who developed the aneurysm simulator?
Bervini: The development is the result of a collaboration between the Department of Neurosurgery at Inselspital Bern and the ARTORG Center for Biomedical Engineering Research at the University of Bern. The project was supported by several research and development funds and won a number of awards. We have since founded the start-up company SurgeonsLab AG to further develop and market the simulator. The simulator can be used not only in vascular neurosurgery, but is also interesting for endovascular interventions or other surgical conditions.
Why did you organize a workshop? What do you learn there?
Bervini: We are convinced that the simulator is an innovative tool that can play an important role in the training of our young surgeons. The rapid development of technology today makes it possible to simulate highly developed brain environments, something that has never been achieved in the past. This is also important because, for various reasons, the new generation of neurosurgeons is coming into less and less contact with these complex operations.
The idea of the workshop is to offer high-quality hands-on teaching. The intraoperative surgical conditions are simulated as realistically as possible. The practical part is supplemented by lectures and case discussions, which allow for discussion and an open exchange between participants and internationally recognized specialists.
For whom is the workshop useful?
Bervini: The workshop is primarily aimed at neurosurgeons who are interested in the treatment of intracranial aneurysms and would like to acquire and/or deepen their microsurgical knowledge in this field. We provide various simulator models of varying complexity at the workshop. This makes it possible to practice microsurgical skills adapted to the individual level of each participant. The workshop is international and is recognized and sponsored by the Swiss Society of Neurosurgery (SGN) and the European Association of Neurosurgical Societies (EANS).
What is the goal for the future?
Bervini: The role of simulation in medicine is highly topical and many specialties have already included simulation in their training curriculum. Simulation is a safe, efficient and innovative way to ensure a high standard of training and care for our patients. Our goal is to further expand access to the simulator for future generations of vascular neurosurgeons. We hope that this workshop can take place on a regular basis and that the Inselspital and the University of Bern will be pioneers in this field.
Related News
- Hands-on Aneurysm Clipping Course28.05.25 - Following the extremely positive feedback from previous years, the «Hands-on Aneurysm Clipping Course» was held for the third time in Bern on May 27…
- Associate professorship for David Bervini20.02.24 - We congratulate our Attending Physician in Neurosurgery, Prof. David Bervini, MD, who has been appointed Associate Professor at the University of…
- Hands-on: aneurysm surgery on the simulator13.03.23 - Aneurysm surgery is challenging. This makes it all the more important to get every move right. This could be practiced at the First Aneurysm…